Refine search
Actions for selected content:
47844 results in Zoology
Biological properties of vitamins of the B-complex, part 2 – vitamins B6 and B7 (biotin, vitamin H)
-
- Journal:
- Nutrition Research Reviews / Volume 38 / Issue 2 / December 2025
- Published online by Cambridge University Press:
- 30 May 2025, pp. 791-824
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Factors associated with meal quality among schoolchildren in three Brazilian cities
-
- Journal:
- British Journal of Nutrition / Volume 133 / Issue 10 / 28 May 2025
- Published online by Cambridge University Press:
- 02 June 2025, pp. 1374-1384
- Print publication:
- 28 May 2025
-
- Article
- Export citation
BJN volume 133 issue 10 Cover and Front matter
-
- Journal:
- British Journal of Nutrition / Volume 133 / Issue 10 / 28 May 2025
- Published online by Cambridge University Press:
- 08 July 2025, pp. f1-f2
- Print publication:
- 28 May 2025
-
- Article
-
- You have access
- Export citation
BJN volume 133 issue 10 Cover and Back matter
-
- Journal:
- British Journal of Nutrition / Volume 133 / Issue 10 / 28 May 2025
- Published online by Cambridge University Press:
- 08 July 2025, pp. b1-b2
- Print publication:
- 28 May 2025
-
- Article
-
- You have access
- Export citation
Exploring the role of diet in reducing cancer risk in UK firefighters: Mediterranean pattern and the potential for targeted nutritional strategies
-
- Journal:
- Nutrition Research Reviews / Volume 38 / Issue 2 / December 2025
- Published online by Cambridge University Press:
- 28 May 2025, pp. 777-790
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
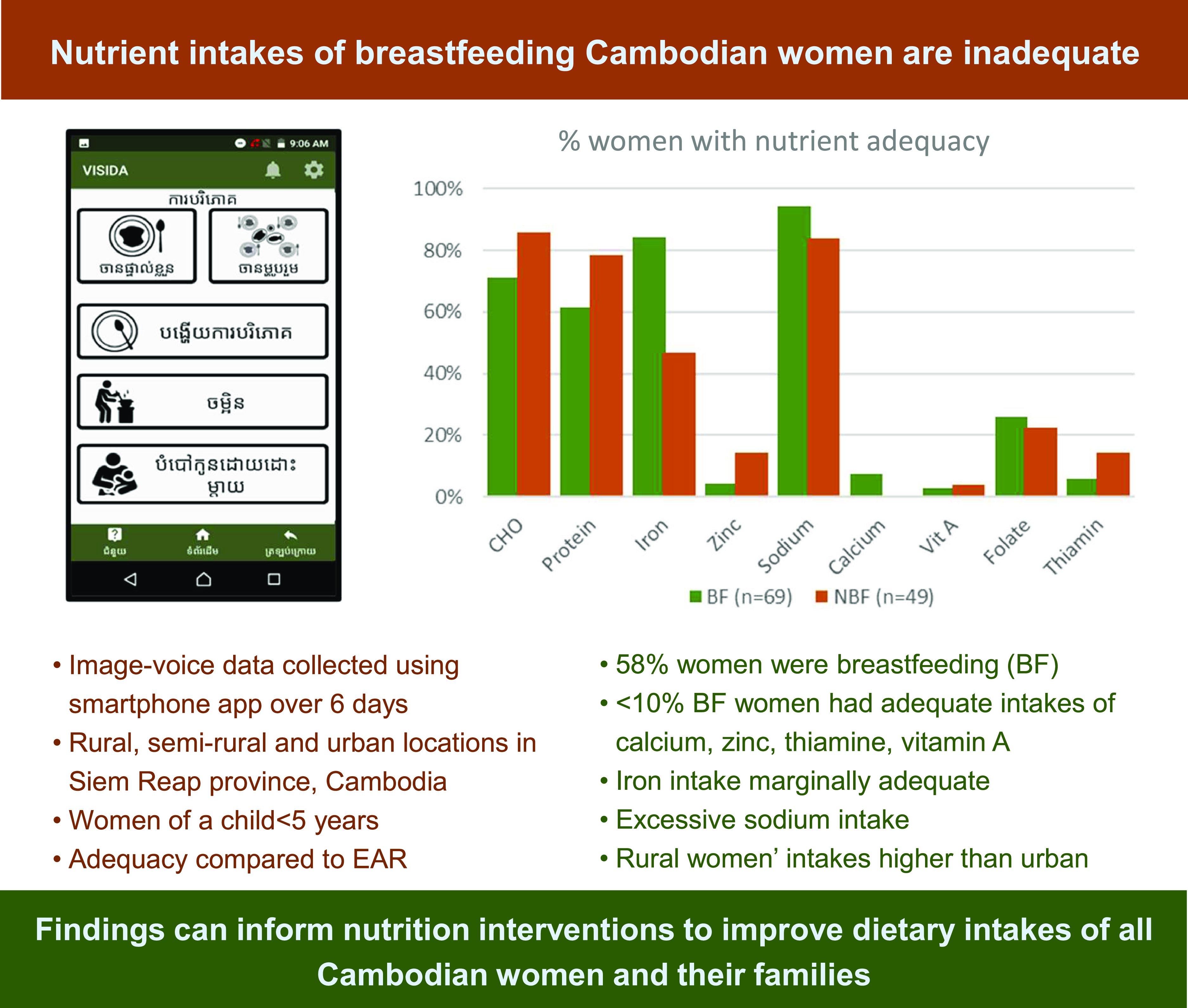
Dietary assessment using a novel image-voice-based system indicates nutrient inadequacies in Cambodian women’s dietary intake
-
- Journal:
- Journal of Nutritional Science / Volume 14 / 2025
- Published online by Cambridge University Press:
- 28 May 2025, e37
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Temporal meal patterns in the Swedish population and associations with socio-demographic variables and nutrient intakes: a cross-sectional study
-
- Journal:
- British Journal of Nutrition / Volume 133 / Issue 10 / 28 May 2025
- Published online by Cambridge University Press:
- 26 May 2025, pp. 1363-1373
- Print publication:
- 28 May 2025
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Healthy dietary patterns, cognition and dementia risk: current evidence and context
-
- Journal:
- Proceedings of the Nutrition Society , First View
- Published online by Cambridge University Press:
- 23 May 2025, pp. 1-11
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
List of Reviewers: 1st November 2023–31st October 2024
-
- Journal:
- Journal of Nutritional Science / Volume 14 / 2025
- Published online by Cambridge University Press:
- 22 May 2025, e36
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
‘My kids have them 5 days a week…’ A survey of the frequency, types, parental experiences, and sociodemographic characteristics of squeeze pouch use in Tasmanian infants and children
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E41
-
- Article
-
- You have access
- Export citation
Hospital food service experiences among older patients—a pilot comparison between Australian-born and culturally and linguistically diverse patients
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E102
-
- Article
-
- You have access
- Export citation
Fat-based dietary patterns are not associated with risk of a first clinical diagnosis of central nervous system demyelination in Australian adults
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E134
-
- Article
-
- You have access
- Export citation
The effectiveness of a 10-week family-focused e-Health healthy lifestyle program for school-aged children with overweight or obesity
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E6
-
- Article
-
- You have access
- Export citation
What do people with irritable bowel syndrome seek from dietetic care? An evaluation of people’s experiences with a dietitian-led low fermentable oligosaccharide, disaccharide, monosaccharide and polyol diet
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E147
-
- Article
-
- You have access
- Export citation
Consumers attitudes about public health interventions to promote portion control of discretionary food: a qualitative focus group study
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E5
-
- Article
-
- You have access
- Export citation
Australian adults’ experiences of running out of food during COVID-19 pandemic restrictions
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E20
-
- Article
-
- You have access
- Export citation
Assessing hand grip strength as a nutritional indicator in hemodialysis patients: reliability and agreement between pre-dialysis and mid-dialysis measurements
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E35
-
- Article
-
- You have access
- Export citation
Testing an audit tool to measure food served and wasted in early childhood education settings
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E77
-
- Article
-
- You have access
- Export citation
Exploring the determinants of food choice in Chinese immigrants living in Australia and Chinese people living in mainland China: a qualitative study
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E1
-
- Article
-
- You have access
- Export citation
Validation and reproducibility of a novel flavonoid food frequency dietary assessment tool against multiple 24hr-recall over 12 months
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue OCE1 / April 2025
- Published online by Cambridge University Press:
- 21 May 2025, E45
-
- Article
-
- You have access
- Export citation