Refine search
Actions for selected content:
47842 results in Zoology
α-Linolenic acid ameliorates pentylenetetrazol-induced neuron apoptosis and neurological impairment in mice with seizures via down-regulating JAK2/STAT3 pathway
-
- Journal:
- British Journal of Nutrition / Volume 132 / Issue 1 / 14 July 2024
- Published online by Cambridge University Press:
- 22 May 2024, pp. 1-12
- Print publication:
- 14 July 2024
-
- Article
-
- You have access
- HTML
- Export citation
Eating out of home in Portugal: characterisation and effects on dietary intake
-
- Journal:
- British Journal of Nutrition / Volume 132 / Issue 2 / 28 July 2024
- Published online by Cambridge University Press:
- 22 May 2024, pp. 169-181
- Print publication:
- 28 July 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Within- and between-person associations of time-varying determinants with snacking in older adults: an ecological momentary assessment study
-
- Journal:
- British Journal of Nutrition / Volume 132 / Issue 2 / 28 July 2024
- Published online by Cambridge University Press:
- 20 May 2024, pp. 236-247
- Print publication:
- 28 July 2024
-
- Article
-
- You have access
- HTML
- Export citation
Association between plant-based diet quality and chronic kidney disease in Australian adults
-
- Journal:
- Public Health Nutrition / Volume 27 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 17 May 2024, e142
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Chronic administration of hydrolysed pine nut oil to mice improves insulin sensitivity and glucose tolerance and increases energy expenditure via a free fatty acid receptor 4-dependent mechanism
-
- Journal:
- British Journal of Nutrition / Volume 132 / Issue 1 / 14 July 2024
- Published online by Cambridge University Press:
- 16 May 2024, pp. 13-20
- Print publication:
- 14 July 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Effects of front-of-package nutrition labelling systems on objective understanding and purchase intention in Panama: results from a multi-arm parallel-group randomised controlled trial
-
- Journal:
- Public Health Nutrition / Volume 27 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 16 May 2024, e192
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
A 12-week double-blind randomised controlled trial investigating the effect of dietary supplementation with 125 μg/d vitamin D in adults with asthma
-
- Journal:
- British Journal of Nutrition / Volume 132 / Issue 6 / 28 September 2024
- Published online by Cambridge University Press:
- 16 May 2024, pp. 738-749
- Print publication:
- 28 September 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Dietary diversity moderates household economic inequalities in the double burden of malnutrition in Tanzania
-
- Journal:
- Public Health Nutrition / Volume 27 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 16 May 2024, e141
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Managing malnutrition and multimorbidity in primary care: dietary approaches to reduce treatment burden
- Part of
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue 4 / December 2025
- Published online by Cambridge University Press:
- 16 May 2024, pp. 381-389
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Oral health and multimorbidity: is diet the chicken or the egg?
- Part of
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue 4 / December 2025
- Published online by Cambridge University Press:
- 14 May 2024, pp. 332-339
-
- Article
- Export citation
Editorial
- Part of
-
- Journal:
- Proceedings of the Nutrition Society / Volume 84 / Issue 4 / December 2025
- Published online by Cambridge University Press:
- 14 May 2024, pp. 327-331
-
- Article
-
- You have access
- HTML
- Export citation
‘Healthier options tend to get lost in the noise of online’ – Australian shoppers’ experiences with online grocery platforms
-
- Journal:
- Public Health Nutrition / Volume 27 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 14 May 2024, e134
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Childhood obesity accelerates biological ageing: is oxidative stress a link?
-
- Journal:
- British Journal of Nutrition / Volume 132 / Issue 2 / 28 July 2024
- Published online by Cambridge University Press:
- 13 May 2024, pp. 227-235
- Print publication:
- 28 July 2024
-
- Article
-
- You have access
- HTML
- Export citation
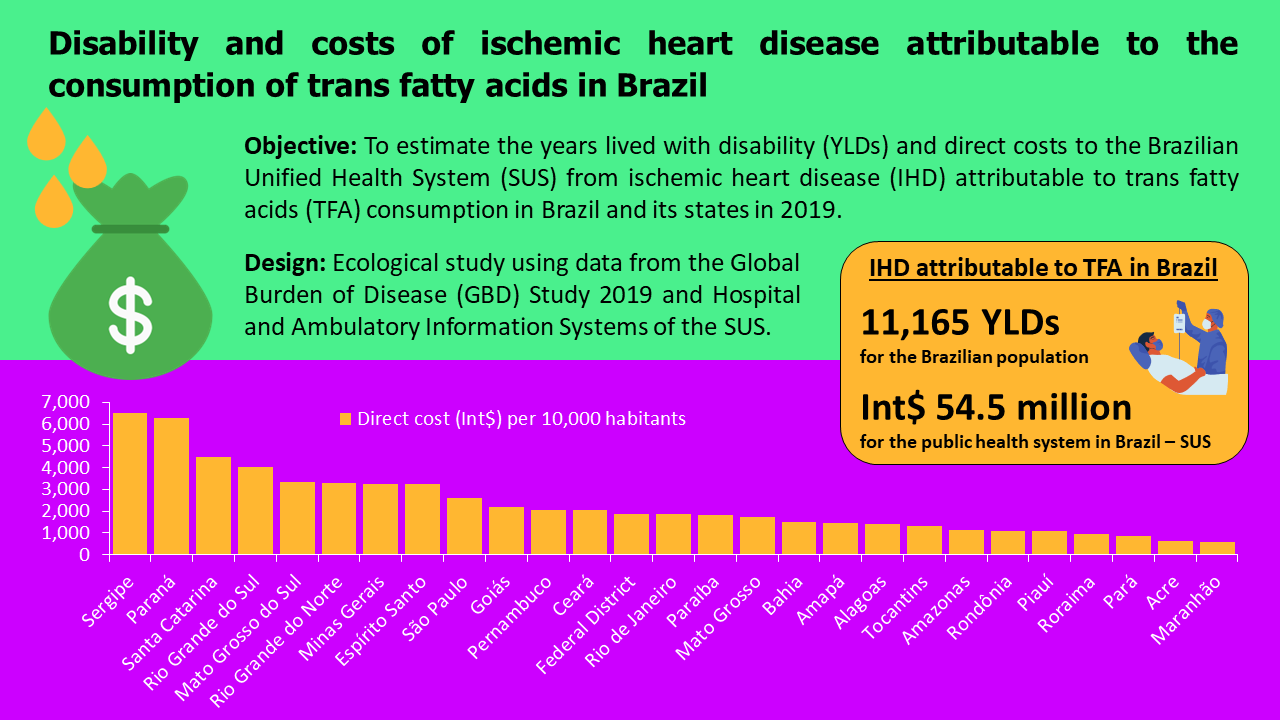
Disability and costs of IHD attributable to the consumption of trans-fatty acids in Brazil
-
- Journal:
- Public Health Nutrition / Volume 27 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 10 May 2024, e132
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Does continuous glucose monitoring influence adherence to time-restricted eating?
-
- Journal:
- Proceedings of the Nutrition Society / Volume 83 / Issue OCE1 / April 2024
- Published online by Cambridge University Press:
- 07 May 2024, E125
-
- Article
-
- You have access
- Export citation
Barriers and enablers to a healthy lifestyle in people with infertility: a mixed-methods systematic review
-
- Journal:
- Proceedings of the Nutrition Society / Volume 83 / Issue OCE1 / April 2024
- Published online by Cambridge University Press:
- 07 May 2024, E84
-
- Article
-
- You have access
- Export citation
Bitter taste sensitivity and frequency of bitter food intake in healthy Australian adults: a cross-sectional, mixed-methods study
-
- Journal:
- Proceedings of the Nutrition Society / Volume 83 / Issue OCE1 / April 2024
- Published online by Cambridge University Press:
- 07 May 2024, E138
-
- Article
-
- You have access
- Export citation
Changes in psychological outcomes and sleep quality following energy restriction with and without almonds
-
- Journal:
- Proceedings of the Nutrition Society / Volume 83 / Issue OCE1 / April 2024
- Published online by Cambridge University Press:
- 07 May 2024, E76
-
- Article
-
- You have access
- Export citation
Dietary intake of adolescent rowers - analysis of energy intake
-
- Journal:
- Proceedings of the Nutrition Society / Volume 83 / Issue OCE1 / April 2024
- Published online by Cambridge University Press:
- 07 May 2024, E43
-
- Article
-
- You have access
- Export citation
Macronutrient intakes of adolescent rowers for growth, development and sports performance
-
- Journal:
- Proceedings of the Nutrition Society / Volume 83 / Issue OCE1 / April 2024
- Published online by Cambridge University Press:
- 07 May 2024, E44
-
- Article
-
- You have access
- Export citation