Refine search
Actions for selected content:
86 results
Shared and distinct alterations of thalamic subregional functional connectivity in early- and late-onset obsessive-compulsive disorder
-
- Journal:
- Psychological Medicine / Volume 55 / 2025
- Published online by Cambridge University Press:
- 01 September 2025, e258
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Progressive gray matter reduction in schizophrenia patients with persistent auditory hallucinations by causal structural covariance network analysis
-
- Journal:
- Psychological Medicine / Volume 55 / 2025
- Published online by Cambridge University Press:
- 29 August 2025, e255
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Exploring connectivity and volume alterations in the Pulvinar’s subnuclei: insights into the neuropathological role in obsessive-compulsive disorder (OCD)
-
- Journal:
- Psychological Medicine / Volume 55 / 2025
- Published online by Cambridge University Press:
- 21 July 2025, e206
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Thalamus as a neural marker of cognitive reserve in bilinguals with frontotemporal dementia
-
- Journal:
- Bilingualism: Language and Cognition , First View
- Published online by Cambridge University Press:
- 22 April 2025, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Chapter 40 - The Pathophysiology of Tremor
- from Section 3: - Hyperkinetic Movement Disorders
-
-
- Book:
- International Compendium of Movement Disorders
- Published online:
- 07 January 2025
- Print publication:
- 06 February 2025, pp 499-512
-
- Chapter
- Export citation
Longitudinal association between depressive symptoms and cognitive function: the neurological mechanism of psychological and physical disturbances on memory
-
- Journal:
- Psychological Medicine / Volume 54 / Issue 13 / October 2024
- Published online by Cambridge University Press:
- 14 October 2024, pp. 3602-3611
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Common neural deficits across reward functions in major depression: a meta-analysis of fMRI studies
-
- Journal:
- Psychological Medicine / Volume 54 / Issue 11 / August 2024
- Published online by Cambridge University Press:
- 23 May 2024, pp. 2794-2806
-
- Article
- Export citation
98 Cognitive Outcomes Following Bilateral Focused Ultrasound Thalamotomy for Tremor
-
- Journal:
- Journal of the International Neuropsychological Society / Volume 29 / Issue s1 / November 2023
- Published online by Cambridge University Press:
- 21 December 2023, pp. 197-198
-
- Article
-
- You have access
- Export citation
Mindfulness training and exercise differentially impact fear extinction neurocircuitry
-
- Journal:
- Psychological Medicine / Volume 54 / Issue 4 / March 2024
- Published online by Cambridge University Press:
- 01 September 2023, pp. 835-846
-
- Article
- Export citation
Chapter 14 - Motor Thalamic Interactions with the Brainstem and Basal Ganglia
- from Section 6: - Motor Control
-
-
- Book:
- The Thalamus
- Published online:
- 12 August 2022
- Print publication:
- 01 September 2022, pp 269-283
-
- Chapter
- Export citation
Chapter 16 - The Thalamus in Cognitive Control
- from Section 7: - Cognition
-
-
- Book:
- The Thalamus
- Published online:
- 12 August 2022
- Print publication:
- 01 September 2022, pp 307-323
-
- Chapter
- Export citation
Chapter 10 - Corticothalamic Feedback in Vision
- from Section 5: - Sensory Processing
-
-
- Book:
- The Thalamus
- Published online:
- 12 August 2022
- Print publication:
- 01 September 2022, pp 206-213
-
- Chapter
- Export citation
The thalamus and its subregions – a gateway to obsessive-compulsive disorder
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, pp. S77-S78
-
- Article
-
- You have access
- Open access
- Export citation
Chapter 9 - Thalamocortical Interactions in the Primary Visual Cortex
- from Section 5: - Sensory Processing
-
-
- Book:
- The Thalamus
- Published online:
- 12 August 2022
- Print publication:
- 01 September 2022, pp 187-205
-
- Chapter
- Export citation
The Clinical and Cognitive Spectrum of Artery of Percheron Infarction: 1-Year Follow-Up
-
- Journal:
- Canadian Journal of Neurological Sciences / Volume 49 / Issue 6 / November 2022
- Published online by Cambridge University Press:
- 10 September 2021, pp. 774-780
-
- Article
-
- You have access
- HTML
- Export citation
Alpha-Mannosidosis: A Novel Cause of Bilateral Thalami and Dentate Nuclei Hyperintensity
-
- Journal:
- Canadian Journal of Neurological Sciences / Volume 49 / Issue 5 / September 2022
- Published online by Cambridge University Press:
- 06 September 2021, pp. 704-705
-
- Article
-
- You have access
- HTML
- Export citation
11 - Processes of Utterance Interpretation: For a Neuropragmatics
- from Part IV - The Processing of Speech Meaning
-
- Book:
- The Study of Speech Processes
- Published online:
- 14 January 2021
- Print publication:
- 21 January 2021, pp 220-238
-
- Chapter
- Export citation
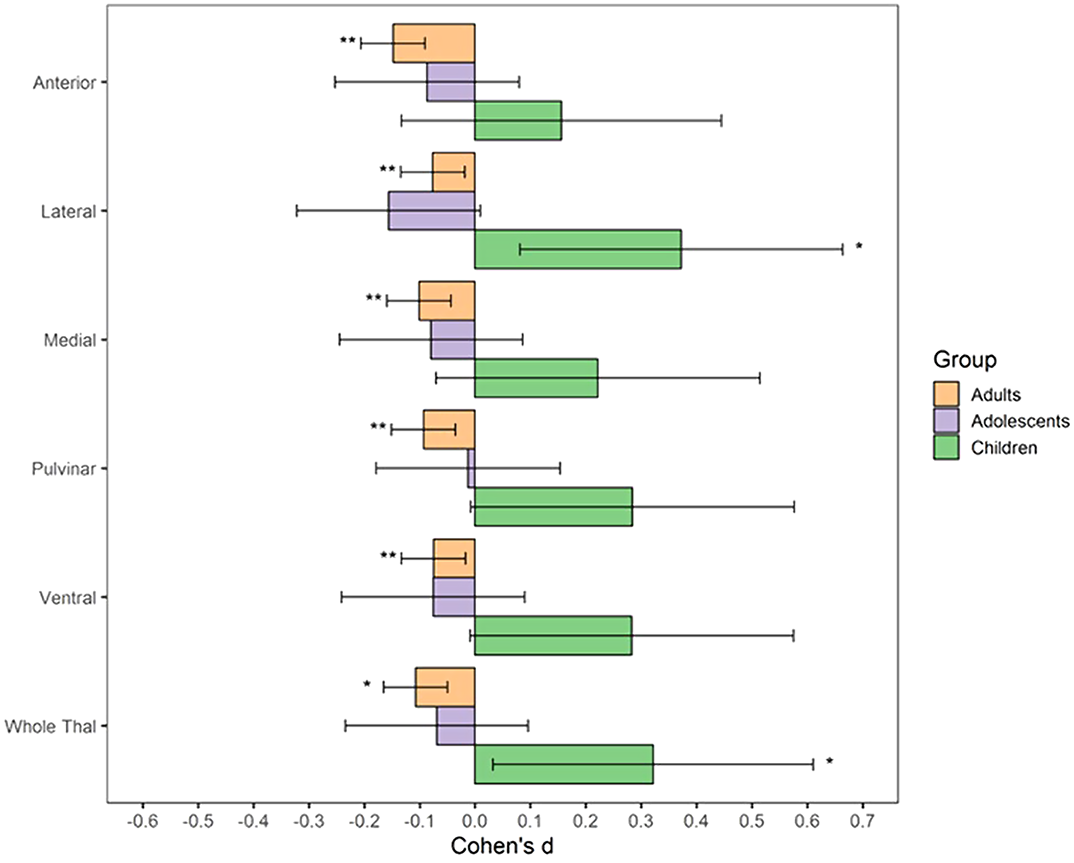
The impact of childhood trauma on thalamic functional connectivity in patients with obsessive–compulsive disorder
-
- Journal:
- Psychological Medicine / Volume 52 / Issue 13 / October 2022
- Published online by Cambridge University Press:
- 20 November 2020, pp. 2471-2480
-
- Article
- Export citation
Stimulation of the Anterior Nucleus of the Thalamus for Epilepsy: A Canadian Experience
- Part of
-
- Journal:
- Canadian Journal of Neurological Sciences / Volume 48 / Issue 4 / July 2021
- Published online by Cambridge University Press:
- 16 October 2020, pp. 469-478
-
- Article
-
- You have access
- HTML
- Export citation
Neural effects of a short-term virtual reality self-training program to reduce social anxiety
-
- Journal:
- Psychological Medicine / Volume 52 / Issue 7 / May 2022
- Published online by Cambridge University Press:
- 03 September 2020, pp. 1296-1305
-
- Article
- Export citation