Introduction
The curative management of head and neck cancer (HNC) requires a multidisciplinary approach that includes multimodality therapy with surgery and/or radiation therapy alone or in combination with chemotherapy, targeted or immunotherapy. Radiotherapy is a critical component of HNC management, requiring precise tumour-targeting to maximize radiation dose to the target volume. Immobilization devices, such as thermoplastic masks, help ensure that the patient’s head and neck region remains in the same position throughout each treatment session, reducing the risk of a geographical miss caused by inadvertent patient motion during treatment. Thermoplastic masks are custom-moulded for each patient, ensuring a comfortably tight fit for reproducible treatment setup, thus minimizing both inter- and intrafraction variation in patient positioning.
However, the use of thermoplastic masks can induce anxiety, discomfort, claustrophobia and psychological distress. Several studies have identified strategies that may be effective for managing thermoplastic mask-induced anxiety such as mindfulness-based stress reduction techniques, cognitive-behavioural therapy and patient education. Reference Aryal, Fogg and Christopher1 The use of effective coping mechanisms can improve treatment compliance, alleviate psychological stress and mitigate the overall emotional impact of wearing thermoplastic masks for radiation treatment. In high-resource settings, various interventions, including pharmacological and non-pharmacological strategies, have been successfully employed to mitigate the impact of thermoplastic mask-induced anxiety. Reference Holland, Andersen and Breitbart2 However, in limited-resource settings, where healthcare infrastructure and support systems are often underdeveloped, effectively addressing anxiety in HNC patients poses a significant challenge.
Despite the significant impact of thermoplastic mask-induced anxiety, little is known about the extent and scope of this challenge among HNC patients managed with radiotherapy in limited-resource settings. Reliable data on effective coping mechanisms used by HNC patients in the Ghanaian context are also scarce. Nevertheless, understanding the psychological effects of using thermoplastic masks remains essential for optimizing patient care, improving treatment efficacy, reducing anxiety-related treatment interruptions, minimizing non-compliance and enhancing the overall treatment experience. The study determined the prevalence and severity of thermoplastic mask-induced anxiety and explored coping mechanisms employed by patients with HNC who were managed with radiotherapy.
Methods
Study design and setting
This was a quantitative cross-sectional study involving patients diagnosed with HNC who received radiotherapy with the use of a thermoplastic mask as an immobilization device. The study was conducted at the largest of three radiotherapy and cancer treatment centres in Ghana.
Study participants
A total population sampling technique was used to recruit eligible patients who received radiotherapy with curative intent between 01 January 2022 and 31 December 2022. Only adult patients > 18 years with HNCs who underwent external beam radiotherapy using thermoplastic immobilization masks were included in the study. Patients with metastatic HNCs were not included in the study, irrespective of the use of thermoplastic masks in their palliative radiation treatment. Also, HNC patients immobilized using other devices such as head straps instead of thermoplastic masks were excluded from the study.
Study size
A total of 262 patients with HNCs, managed at the study site during the study period, were screened for eligibility. Questionnaires were administered to all 160 eligible participants at a response rate of 90·6% (n = 145).
Data sources
Data were retrospectively collected through self-reporting at the end of radiation treatment. A structured questionnaire with three sections was used to collect quantitative data for the study. The demographic section collected basic patient information, such as age and gender, whereas the clinical data section captured details about the patient’s diagnoses, cancer stage and Eastern Cooperative Oncology Group (ECOG) performance status. The third section focused on anxiety experienced during the mask-moulding process and radiation treatment sessions, utilizing a Likert scale of 1–5 to rate anxiety levels at various treatment stages. It also explored coping mechanisms employed by patients, their effectiveness and the support received for managing anxiety. The research tool underwent a piloting phase with a small group of 10 patients to assess clarity, relevance and feasibility, and it was refined based on feedback. In terms of reliability, the instrument was tested using Cronbach’s alpha, which yielded a value of 0·86. While the tool has not been formally validated against established anxiety scales, it was designed to capture specific anxiety triggers relevant to the patient population under study. The decision to develop an in-house tool was made to ensure that the questions were directly aligned with the treatment process and stages experienced by radiotherapy patients.
Statistical methods
Data were analysed using the Statistical Package for Social Sciences software, version 26·0. Patients’ electronic hospital-based medical records were also accessed with consent to retrieve missing clinical and/or demographic data where necessary. Frequency distributions and percentages were used to present the data. Inferential statistical analyses using chi-squared tests and likelihood ratios were used to establish associations between anxiety and age/gender. To account for multiple comparisons and reduce the risk of Type I errors, Bonferroni correction was applied when testing associations between anxiety, age and gender at different treatment stages. The adjusted significance threshold was used to ensure statistical robustness. P-values < 0·05 were considered statistically significant after correction.
Ethical considerations
Ethical approval was obtained from the institutional review board (SBAHS/AA/RAD/10851545/2022–2023). Written informed consent was obtained from the participants, whose data were also analysed anonymously.
Results
Baseline characteristics
In all, there were 145 participants with a male to female sex ratio of 1·9:1 and a median age of 52·8 years (IQR 20·7), ranging from 18 to 82 years. A significant majority (72·3%) were diagnosed with locoregionally advanced disease (stage groups IIIA, IIIB and IIIC) (Table 1).
Table 1. Baseline characteristics (n = 145)
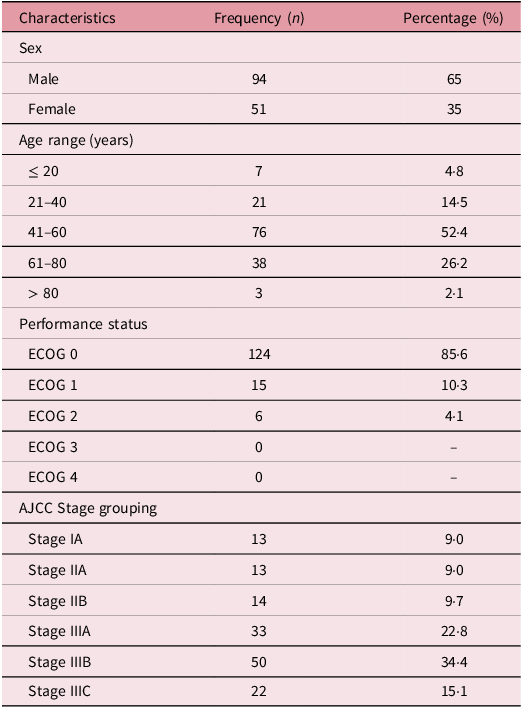
ECOG, Eastern Cooperative Oncology Group; AJCC, American Joint Committee on Cancer.
Prevalence of thermoplastic mask-induced anxiety
There was a high prevalence of anxiety during the mask-moulding process as well as during radiation treatment, 93·8% (n = 136) and 94·5% (n = 137), respectively.
Thermoplastic mask-induced anxiety levels during the radiation therapy process
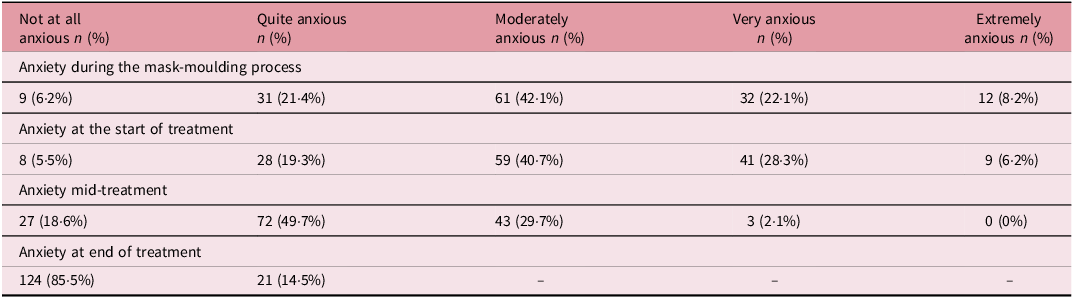
During the mask-moulding process, anxiety levels varied, with 6·2% reporting not being anxious at all, whereas 42·1% felt moderately anxious and 22·1% very anxious. At the start of treatment, 5·5% were not anxious, contrasting with 40·7% moderately anxious and 28·3% very anxious. Mid-treatment, there was a shift with 49·7% feeling quite anxious and 29·7% moderately anxious, whereas at the end of treatment, 85·5% were not anxious at all. Generally, there was a decrease in anxiety levels from the start to the end of treatment (Table 2).
Table 2. Anxiety levels at different stages of the radiation therapy process
Association between age/sex and the incidence and severity of anxiety
Significant associations were found between age and anxiety at the baseline (X 2: 82·677, LR: 80·059, p = 0·001) and mid-way through radiotherapy (X 2: 56·941, LR: 57·966, p = 0·001), as well as general daily anxiety (X 2: 49·064, LR: 50·669, p = 0·027) as summarized in Table 3. Regarding sex, significant relationships were observed for anxiety during the thermoplastic mask-moulding process (X 2 = 5·206, LR = 8·122, p = 0·023), at baseline prior to starting radiotherapy (X 2 = 22·915, LR = 29·847, p = 0·001), mid-way through radiotherapy (X 2 = 18·998, LR = 27·587, p = 0·001) and general daily anxiety levels (X 2 = 16·847, LR = 18·218, p = 0·002).
Table 3. Analysis of age group/sex and anxiety with chi-square, likelihood ratios and p-values
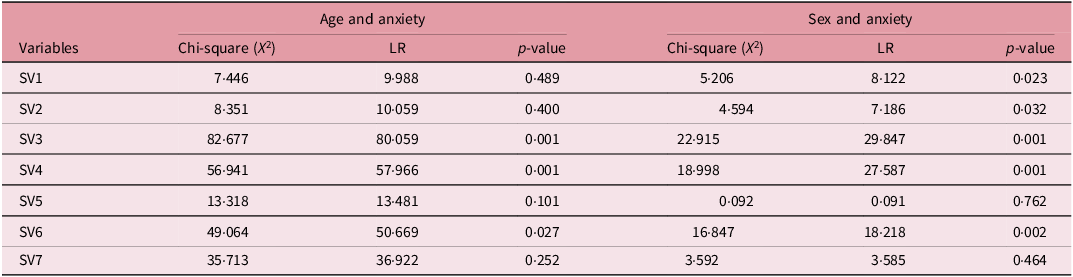
LR, likelihood ratio. SV1 = occurrence of anxiety during mask-moulding process, SV2 = severity of anxiety during mask-moulding, SV3 = severity of anxiety at baseline, SV4 = severity of anxiety mid-treatment, SV5 = severity of anxiety at end of treatment, SV6 = general daily anxiety, SV7 = frequency of occurrence of anxiety during treatment. SV2–SV7 were evaluated with a Likert scale of 1–5.
Awareness and utilization of coping mechanisms
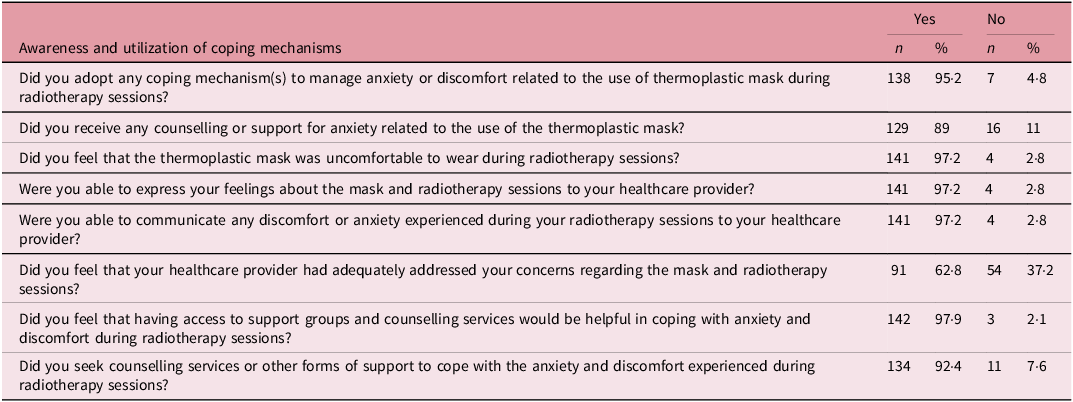
Table 4 summarizes participants’ responses to questionnaire items regarding awareness and utilization of coping mechanisms for thermoplastic mask-induced anxiety. In all, 138 (95·2%) participants adopted various coping mechanisms for anxiety during the radiotherapy process. Most participants, 97·2%, found the mask uncomfortable and were able to express their feelings to healthcare professionals. There was a high level of coping mechanism adoption and communication with healthcare providers, alongside a notable demand for additional support and counselling services.
Table 4. Awareness and utilization of coping mechanisms (n = 145)
Coping mechanisms adopted by participants (n = 145)
Coping mechanisms employed by the participants were not mutually exclusive. Some participants adopted two or more strategies simultaneously as shown in Figure 1. Distraction was the most frequently employed strategy (58%), followed by visualization techniques, adopted by 46%.
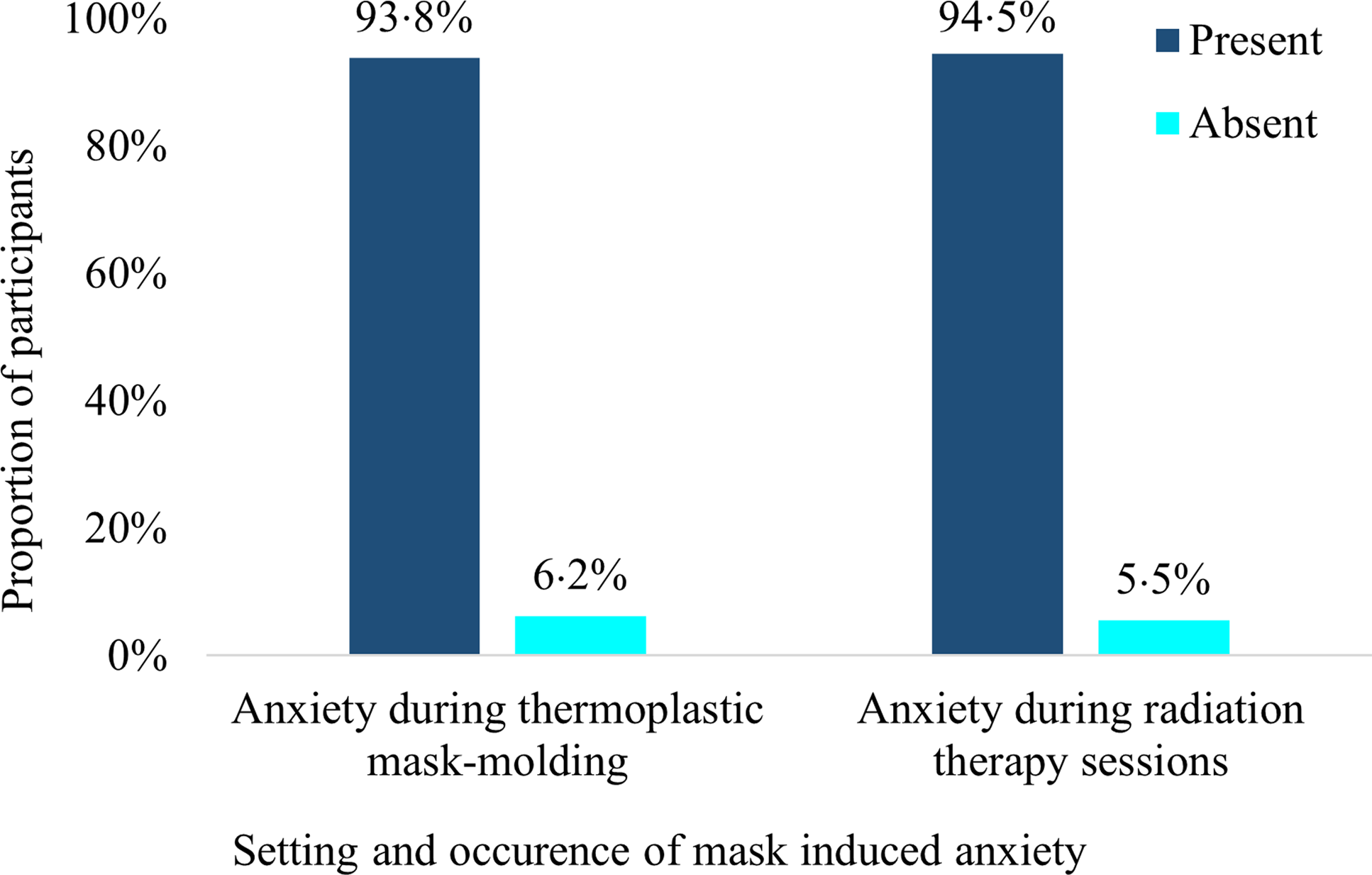
Figure 1. Coping mechanisms adopted by participants.
Discussion
A substantial proportion (52·4%) of the participants were between 41 and 60 years old, consistent with previous studies indicating that HNCs are more common in middle-aged and older adults. Reference Siegel, Miller and Jemal3 A retrospective study by Bansal et al. (2017) on patients receiving radiotherapy for HNCs in a resource-limited setting similarly reported a majority of patients in their 40s and 50s. Reference Bansal, Puri and Mehta4 This age group often represents individuals at the peak of their socioeconomic responsibilities, which can further amplify their anxiety about the impact of HNCs and treatment on their livelihoods. Reference Harris, Gorman and Guttman5 Interestingly, 4·8% of the participants were ≤ 20 years old, which is relatively high for this age group. Also, 2·1% were over 80 years, reflecting the bimodal age distribution sometimes seen in HNCs. Reference Saba, Wong and Kim6 Also, significant associations were found between age and anxiety at both baseline and mid-treatment stages (p = 0·001) as well as general daily anxiety (p = 0·027), suggesting that younger patients tend to experience higher levels of anxiety at these stages, possibly due to differences in emotional resilience or coping capacity across age groups. Reference Stiegelis7 After applying Bonferroni correction for multiple comparisons, reassessment of the statistical significance of these findings ensured that they were not driven by an inflated Type I error rate. The adjusted results remained statistically significant, reinforcing the observed association between younger age and heightened anxiety levels. This highlights the importance of tailoring anxiety interventions to different age groups, particularly in resource-limited settings where structured psychological support may be lacking.
The predominance of advanced-stage presentation (stages IIIA, IIIB and IIIC—72·4%) is alarming but expected. In Low and Middle Income Countries (LMICs), several factors contribute to the late presentation of cancer patients, including low health literacy, cultural beliefs and financial barriers that delay medical consultation. Reference Adeloye8 Early detection rates of cancer in low-resource settings are lower due to limited access to health care, diagnostic delays and lack of routine screening programmes. Reference Sankaranarayanan, Swaminathan and Brenner9 Advanced-stage disease is typically associated with more aggressive treatment regimens, which often result in greater physical and psychological distress, which can exacerbate procedural anxiety, including that related to thermoplastic mask usage during radiotherapy. Reference Kiyohara, Maehar and Motegi10,Reference Sharma, Tripathi and Garg11
The prevalence of thermoplastic mask-induced anxiety was notably high during both the mask-moulding process (93·8%) and radiation therapy sessions (94·5%). These anxiety levels were notably higher than reported in studies from resource-rich settings, where thermoplastic mask-induced anxiety prevalence tends to range from 50 to 70%. Reference Kiyohara, Maehar and Motegi10 Several factors may have contributed to the exceptionally high thermoplastic mask-induced anxiety levels. First, in limited-resource settings, where access to psychological support services may be minimal or absent, patients often face the psychological demands of cancer treatment without adequate counselling or anxiety-reducing interventions, Reference Bansal, Puri and Mehta4 which could explain the near-universal anxiety levels in the study population.
In contrast, studies from Nixon et al. (2019) in more resource-equipped settings also found high levels of mask-related anxiety, with their interventions including pre-treatment education and psychological support to mitigate such distress. Reference Nixon, Brown and Pigott12 These studies suggest that when patients are educated about what to expect, anxiety levels tend to decrease, which aligns with the findings of Bokmand et al. (2019), where providing clear explanations of the treatment process reduced patient anxiety. Reference Bokmand, Andersson and Kjær13 In settings where this education is lacking, the fear of the unknown and uncertainty about the treatment process may amplify anxiety. Additionally, the physical discomfort associated with the use of thermoplastic masks, such as the pressure on the face and breathing difficulty, can increase anxiety. This is especially true for patients with pre-existing claustrophobia or respiratory difficulties, which may have been prevalent in our study population. It is worth noting that the self-reported nature of the anxiety data in this study means that recall bias could have influenced the findings, with patients potentially overstating their anxiety or adjusting their recollection of earlier experiences. However, other studies support the notion that mask-related anxiety is a common challenge across different settings, reinforcing the validity of our findings. Reference Nixon, Cartmill and Turner14,Reference Dhillon and Halkett15
The elevated anxiety during mask moulding highlights the distress patients feel when encountering a thermoplastic mask for the first time. Anxiety levels varied significantly during different stages of the radiotherapy process, decreasing progressively as treatment progressed. This could have been partly because of a lack of familiarity and experience with the radiotherapy process. Cancer patients who are new to radiotherapy may feel anxious due to unfamiliarity with the procedures and equipment involved. This trend suggests that while the initial phases of radiotherapy are highly anxiety-inducing, patients tend to adapt over time, resulting in lower anxiety levels as they become more accustomed to the treatment process. These findings highlight the importance of providing psychological support, especially during the early stages of treatment, to help manage and mitigate anxiety in HNC patients undergoing radiotherapy. Studies from similar resource-limited environments have shown that when patients are adequately informed and prepared, anxiety levels decrease significantly. Reference Schoenfeld16 Simple interventions such as pre-treatment tours of the radiation therapy unit or brief relaxation exercises before mask moulding can significantly reduce anxiety levels, even in resource-constrained settings. Reference Hu17 The progressive reduction in anxiety reflects the adaptability of patients over time and aligns with findings from other studies, where patients reported becoming more accustomed to the treatment environment, reducing their anxiety levels over time. Reference Nixon, Brown and Pigott12,Reference Spalding18 The most significant reduction in anxiety was observed at the end of treatment, with 85·5% of participants reporting no anxiety, suggesting that completing the prescribed radiotherapy regimen may evoke a sense of relief and accomplishment in patients. Additionally, patients might feel reassured by the completion of their prescribed treatment, reducing uncertainty and emotional distress. Reference Kumar19 There were significant associations between age and anxiety at both baseline and mid-treatment stages of radiotherapy (p = 0·001), as well as general daily anxiety (p = 0·027), suggesting that younger patients tend to experience higher levels of anxiety at these stages, possibly due to differences in emotional resilience or coping capacity across age groups. Reference Stiegelis7
While nearly all patients (97·2%) were able to express their discomfort and anxiety, only 62·8% felt that the healthcare professionals adequately addressed these challenges. This gap between communication and resolution highlights a significant challenge in resource-constrained environments: even when patients can articulate their anxiety, providers may lack the time, training or resources to respond effectively. Reference Batista20 In all, 92·4% of the participants sought counselling or other forms of support, which indicates that patients are not only aware of their need for help but are also proactive in seeking it. Despite the high utilization of coping mechanisms (95·2%) and the willingness of most patients to communicate their concerns, there remains a need for structured psychological interventions, which would not only reduce treatment-related anxiety but also increase adherence to therapy. Reference Wu21 This finding is consistent with the findings of a study that emphasized the need for systematic screening and psychological support in radiotherapy settings. Reference Holtzman, Pereira and Yeung22
Many HNC patients employed more than one strategy simultaneously, which aligns with the understanding that coping is a dynamic and multifaceted process, particularly in high-stress situations like radiotherapy. Distraction (58%) was the most frequently employed coping mechanism, encompassing techniques such as focusing on specific thoughts, memories or tasks that effectively divert attention away from sources of distress and anxiety. Distraction offers a practical and accessible strategy that patients can adopt independently. In the context of radiotherapy, where patients must remain immobile and may experience feelings of confinement due to the thermoplastic mask, distraction offers a way to manage both the physical discomfort and emotional distress. Visualization was the second most popular strategy, employed by 46%, which involved mentally imagining pleasant or relaxing scenarios to counteract the stress and discomfort of being in the immobilized position required for radiotherapy. Visualization is a self-administered, cost-free coping mechanism that can be easily taught to patients during pre-treatment consultations. Encouraging the use of such techniques can help enhance patient comfort during radiotherapy. Social support also plays a crucial role in alleviating anxiety in medical settings, particularly for patients undergoing long-term treatments like radiotherapy. Reference Kandasamy23 In all, 34% adopted the strategy of talking to a loved one or friend during radiotherapy sessions. Having someone to talk to can provide emotional comfort, reassurance and a sense of connection, which can counteract the anxiety and isolation patients may feel during their treatment sessions.
The widespread use of informal coping mechanisms underscores the importance of empowering patients with self-help strategies. Healthcare providers need to play a proactive role in educating patients about coping strategies before treatment begins, to ensure they have practical tools to manage their anxiety and discomfort, particularly in settings with limited mental health services. Training of healthcare providers on effective communication strategies to address patient discomfort and anxiety is very essential.
Limitations
The cross-sectional design limits the ability to infer causality between the use of thermoplastic masks and anxiety levels. Longitudinal studies are needed to establish temporal relationships and assess long-term psychological impacts. The reliance on self-reported data may introduce response and recall biases, with the possibility of participants under- or overreporting anxiety levels.
Conclusions
The high prevalence of thermoplastic mask-induced anxiety highlights a critical aspect of HNC patient care that may be overlooked in resource-limited settings. There was a high level of awareness and utilization of coping mechanisms among HNC patients undergoing radiotherapy. However, the gap between patient communication and the resolution of concerns suggests a need for more structured support services. The high demand for counselling and support groups further emphasizes the importance of integrating mental health care into HNC treatment protocols.
Recommendations
It is crucial to implement targeted interventions that address the anxiety experienced by patients undergoing radiotherapy with thermoplastic masks, particularly in resource-limited settings. Given that certain coping mechanisms were found to be valuable, these could be recommended and proactively coached to patients prior to the mask-moulding process and treatment sessions. Simple and cost-effective interventions, such as distraction techniques (e.g. music or video), should be considered. Prospective identification of patients with higher anxiety or support needs could also be beneficial, allowing healthcare providers to offer individualized support, such as in-the-moment coaching, before or during the procedure. Training healthcare providers to recognize signs of anxiety and providing them with easy-to-implement tools, such as guided relaxation or distraction techniques, would allow for timely intervention. Such approaches would help reduce anxiety without requiring significant financial resources, while also improving patient comfort and the overall treatment experience. Future research could investigate the feasibility of patient-customized masks, open-face masks or other positioning techniques that maintain treatment accuracy while enhancing patient comfort.
Competing interests
The author(s) declare that they have no conflict of interest.







