Introduction
The advanced practice provider role, including physician assistants and nurse practitioners, facilitates continuity of care within specific patient populations or care settings, improves quality metrics, and improves patient and care team satisfaction. Reference Hoerst, Bakar and Cassidy1–Reference Andre, Zachary and Elhoff5 Advanced practice providers are essential team members in the care of paediatric cardiac patients, often providing care in various cardiology subspecialties across inpatient and outpatient settings. Reference Willis, Hoerst and Hart2,Reference Torzone and Birely4 Many inpatient cardiac care settings, including cardiac intensive care units and acute care cardiology units, leverage advanced practice providers in their care model. In a recent network-wide survey by the Pediatric Acute Care Cardiology Collaborative (PAC3), over 90% of participating paediatric heart centres reported employing these providers. Reference Hoerst, Bakar and Cassidy1 Additionally, utilisation of advanced practice providers within the acute care cardiology units was correlated with higher surgical volumes, care of higher acuity patients on the unit, and shorter postoperative length of stay. Reference Willis, Hoerst and Hart2
Paediatric cardiology is a highly complex specialty that addresses a diverse spectrum of cardiac anatomy and cardiovascular physiology. Furthermore, available interventions for children and adults with congenital heart disease are constantly evolving. Reference Andre, Zachary and Elhoff5 Physicians typically complete a three-year paediatrics residency followed by a three-year categorical cardiology fellowship and often pursue additional year(s) of subspecialty training. Reference Frank, Glickstein and Brown6 In contrast, advanced practice providers enter the workforce with highly variable training and prior clinical experiences. Reference Kleinpell, Grabenkort and Kapu3,Reference Andre, Zachary and Elhoff5,Reference Justice, Callow and Loomba7–Reference McBride, Alden and Sorce10 Physician assistant programmes are two to three years and provide limited exposure to paediatrics, often only a single rotation that varies in length by programme, and individuals enter training programmes with variable prior clinical experience. Nurse practitioners begin their careers as nurses before pursuing a master’s or doctorate degree. Some may have years of experience in a paediatric cardiac intensive care unit, while others may only complete a paediatric-focused academic programme where exposure to congenital heart disease is not a requirement. This emphasises the importance of effective onboarding for both roles upon hire. Reference McBride, Alden and Sorce10 Standardised curricula and ongoing education initiatives have been noted to optimally prepare advanced practice providers to care for these specialised populations. Reference Justice, Florez and Diller8,Reference McGrath, Jacobs and Watts9 At present, there are no national board certifications or associated curricula universally provided to advanced practice providers seeking inpatient acute care specialisation within paediatric cardiology. While structured subspecialty training opportunities are slowly increasing in popularity for midlevel providers, a significant educational gap persists for novice practitioners entering highly specialised fields. Reference McGrath, Jacobs and Watts9
PAC3 is a learning collaborative aiming to improve outcomes and optimise care quality in acute care cardiology. Reference Hoerst, Bakar and Cassidy1,Reference Kipps, Cassidy and Strohacker11 As a learning network, PAC3 is uniquely poised to leverage multicentre collaboration to improve the provision of paediatric cardiac care. We sought to understand the current state of advanced practice provider education and onboarding in paediatric acute care cardiology units within the PAC3 network. This needs assessment also sought to identify opportunities for curricular improvements.
Materials and methods
This was a multi-institutional, cross-sectional, descriptive study to assess current practices of education and onboarding of advanced practice providers within participating PAC3 heart centres. This study was reviewed by the University of Texas Southwestern Institutional Review Board and determined to be exempt. Four faculty members from the University of Texas Southwestern, Stanford University, and the University of Cincinnati with expertise in adult education convened a collaborative focus group to develop and test survey items using cognitive interview and pilot testing prior to distribution. Reference Artino, La Rochelle and Dezee12 Survey items were primarily multiple choice with categorical and numeric interval responses and a five-point Likert rating scale to assess agreement level. Free response questions were included to capture strengths and improvement opportunities related to current institutional onboarding practices. At the time of the study, 47 institutions across the United States and Canada participated in PAC3, representing a range of programme sizes and characteristics. The survey was electronically distributed from 1 May to 31 May 2023 to institutional representatives from each PAC3 programme (N = 47) to be directed to leaders managing the onboarding of newly hired advanced practice providers. One response per institution was requested. Incomplete responses and those reflecting non-acute care settings were excluded from the analysis.
Descriptive statistics were utilised for categorical variables. Inductive qualitative methods were used for the free-text responses. Two researchers (L.H. and A.B.) independently applied inductive open coding to derive and assign codes to each text response. Codes were compared, and discrepancies were reconciled between the two researchers. Thematic analysis was applied based on code content to determine onboarding practice themes. Reference Kiger and Varpio13
Results
Programme characteristics
There were a total of 28 survey respondents, reflecting 24 out of 47 paediatric heart centres, with a response rate of 51%. Out of the respondents, 19 were included in the final analysis of advanced practice provider onboarding to paediatric acute care cardiology units, representing 19 active PAC3 paediatric heart centres. Of those excluded, seven reflected primarily cardiac intensive care onboarding, one response was incomplete, and one programme had two respondents, of which only the first response was included. All the respondents were active participants in the onboarding of advanced practice providers, with a majority identifying as nurse practitioners (94.7%) and one physician respondent.
Programme size and characteristics varied widely (Table 1). Unit size, as reflected by the number of acute care cardiology beds, ranged from 6–10 beds (15.8%, n = 3) to > 30 beds (15.8%, n = 3). Most programmes reported unit size > 15 beds (57.9%, n = 11). A majority of units reported advanced practice provider cohorts of ≤ 10 team members (63.2%, n = 12). Cohort sizes ranged from 1–5 advanced practice providers (42.1%, n = 8) to > 20 providers (15.8%, n = 3). The typical staffing ratio for advanced practice provider assignments was 5 to 6 patients per provider (73.7%, n = 14).
Table 1. Acute care cardiology unit programme characteristics

ACCU = acute care cardiology unit; APP = advanced practice provider.
Current onboarding practices
From March 2022 to March 2023, 79% (n = 15) of programmes reported onboarding at least one newly hired advanced practice provider, with nearly half of the programmes (47.4%, n = 9) onboarding three or more. The most frequently cited length of orientation required prior to independent practice was 3–4 months (57.9%, n = 11). At the completion of the orientation period, 36.8% (n = 7) of centres reported using a formal evaluation or competency-based assessment.
Programmes incorporated a variety of learning methods into their orientation process (Figure 1). All programmes utilised standard precepting methods, defined as experienced practitioners providing supervision and feedback to a clinical trainee. Shadowing, when a trainee strictly observes an experienced practitioner, was also common (78.9%, n = 15). Most programmes (78.9%) provided dedicated time with relevant cardiology subspecialties outside of their primary unit. Other methods included in-person didactics (73.7%, n = 14), online lecture-based videos (63.2%, n = 12), or use of other online educational resources (73.7%, n = 14). Some programmes augmented onboarding with physician or senior practitioner mentorship (47.4%, n = 9), graduated autonomy (63.2%, n = 12), and simulation experiences (26.3%, n = 5).

Figure 1. Methods utilised in onboarding advanced practice providers.
Most respondents (84.2%, n = 16) agreed or strongly agreed that new hires are prepared for independent practice after onboarding completion, and 68.4% (n = 13) agreed or strongly agreed that their onboarding programme meets all new hire learning needs. All respondents indicated that the addition of an online curriculum for onboarding would be beneficial (Figure 2).
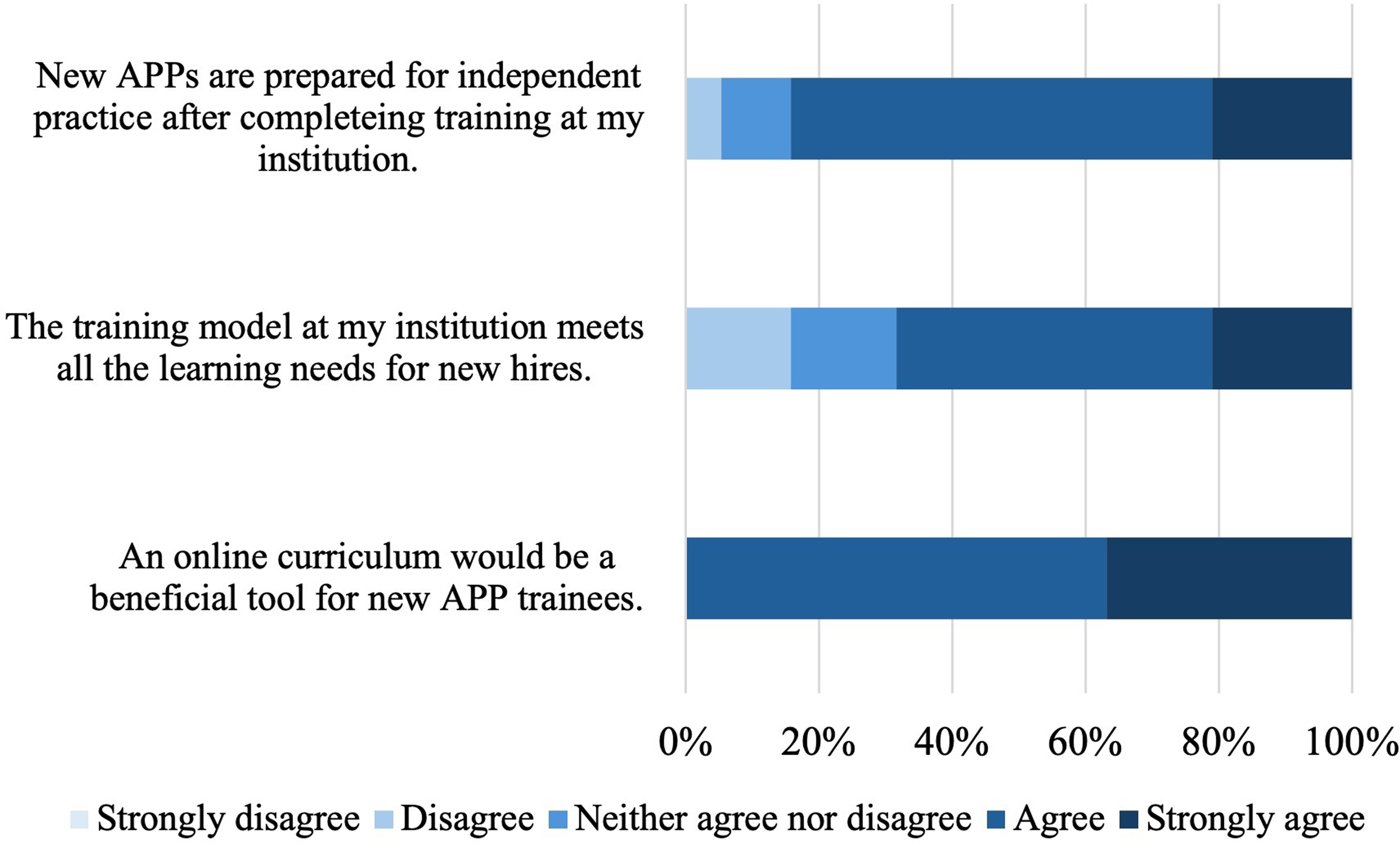
Figure 2. Respondent perception of current onboarding model. APP = Advanced practice provider.
Key onboarding elements
Strengths of the institution’s current onboarding model and perceived opportunities for improvement were elicited in two open-ended questions. Three main themes were identified as important components of onboarding models: (1) structure, (2) individualised learning, and (3) team support. These themes were further divided into specific elements with selected quotes from free-text responses representing strengths or opportunities for improvements in the onboarding process (Table 2).
Table 2. Thematic analysis of key onboarding elements
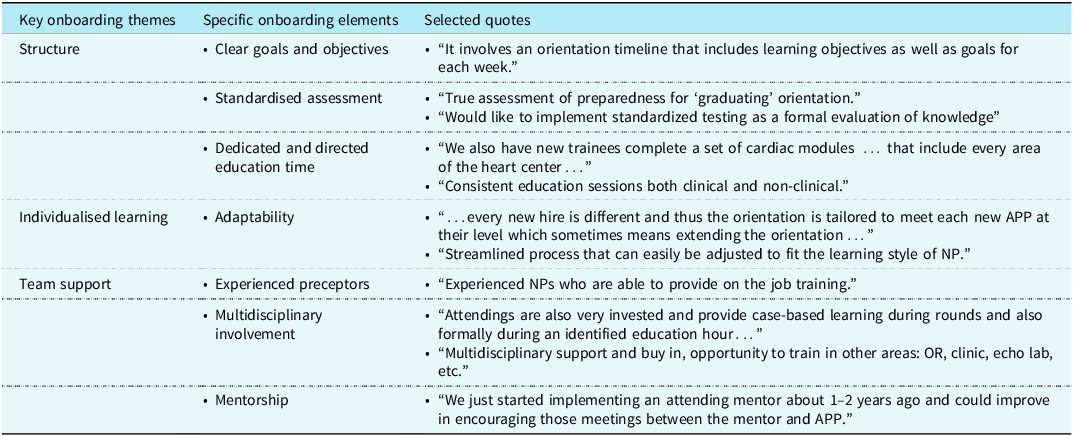
APP = advanced practice provider; NP = nurse practitioner; OR = operating room.
The first theme that was identified was a need for a structured onboarding process. Within this, three specific domains emerged, including setting specific goals and objectives, an assessment mechanism, and dedicated education time. Several respondents referenced needing a more “uniform,” “structured,” or “standardised” onboarding process. These comments infer a current lack of an organised curriculum. Other respondents highlighted that having a formalised orientation outline with timely and specific goals and objectives was important. Additionally, there were frequent comments regarding the need for a structured assessment tool, reinforcing that only 36.8% (n = 7) of centres utilise a formal assessment instrument. Several respondents referenced needing a way to assess a trainee for “readiness” at the end of the onboarding process prior to transitioning them to independence. Some specifically wanted a competency-based assessment tool, and others were looking for a knowledge-based tool. The need for dedicated and structured education time for the trainees was of high value for many respondents. Over half of respondents (63.2%) specifically commented on the importance of a lecture-based curriculum or learning modules. A few respondents indicated having a well-developed, organised didactic curriculum as part of their onboarding. However, others indicated they have no formal teaching sessions or structure to didactics offered. Less often mentioned was incorporating experiential learning opportunities such as simulation or case-based learning.
While structure appeared to be a high priority, a second theme identified was the importance of individualised learning. New hire advanced practice providers have variable backgrounds, clinical experience, and learning needs. The ability to tailor the experience to the trainee with flexibility in the process was important to respondents. One respondent commented on a time-variable approach that may require extending the onboarding process for individuals with less experience. Another respondent acknowledged necessary adaptability within the structured curriculum to meet the needs of different learning styles.
The third theme identified was team support from experienced preceptors and with multidisciplinary involvement and mentorship. Several respondents commented on the importance of experienced, engaged, and knowledgeable preceptors as a key component of onboarding. While most preceptors are experienced advanced practice providers, multidisciplinary support from physicians and other subspecialties is highly valued. Many indicated a desire to have further involvement by physicians as mentors to new advanced practice providers.
Discussion
In this study, we affirm that paediatric acute care cardiology teams commonly utilise advanced practice providers and frequently onboard new practitioners, often with variable backgrounds and experience. This study highlights key elements and gaps for successful onboarding of advanced practice providers to a subspecialty like paediatric cardiology. A barrier for some programmes was a lack of formalised onboarding and curriculum for new hires. Important aspects of a structured onboarding curriculum were clear goals and objectives, dedicated learning opportunities, trainee assessment, and the ability to prioritise individualised learning. Supporting the trainee with experienced and knowledgeable preceptors was a key element and a strength for many programmes. Multidisciplinary support and mentorship were also valuable components. Justice et al. Reference Justice, Callow and Loomba7 reported similar findings of variable orientation practices for cardiac intensive care advanced practice providers. There was limited use of orientee assessment, and orientees desired more structured didactic education with clear objectives, management guidelines, and more simulation.
There are opportunities for improvement in onboarding, with 32% of respondents conveying that their current model does not meet all the needs of new hires. While many agreed that orientees are prepared to transition to independent practice after orientation, there was significant variability in time dedicated to onboarding. In addition, many respondents who considered their model to be adequate to transition a new hire to safe practice still identified opportunities for improvement in the structure of the curriculum, assessment, adaptability, or mentorship. This suggests opportunities to improve current models in quality, efficiency, or efficacy, though additional study is needed.
These gaps can be addressed by individual institutions. However, there are significant opportunities for national organisations to support these efforts with widely accessible educational content, curriculum resources, and a framework for assessment that can be tailored to the unique needs of institutions and advanced practice provider orientees. There are models that provide detailed curriculum outlines and assessment tools that programmes can adopt for intensive care advanced practice provider programmes. Reference Sorce, Simone and Madden14,Reference Luckianow, Piper and Kaplan15 In response to the identified gap by Justice et al., Reference Justice, Callow and Loomba7 a committee of the Pediatric Cardiac Intensive Care Society created a peer-reviewed curriculum with educational resources for learners, a didactic course, and simulation scenarios that improved attendee-perceived knowledge and confidence to practice. Reference Justice, Florez and Diller8
A widely accessible, standardised, lecture-based curriculum for advanced practice providers would be valuable and meet a need for many programmes. Online learning has become a common and effective educational modality in paediatric cardiology. Reference Motonaga, Sacks and Olson16,Reference Tretter, Windram and Faulkner17 Most programmes presently utilise online educational resources (73.7%) or online lecture-based videos (64.3%), and all programmes endorse that an online curriculum would be beneficial. These platforms improve access to education for a wide range of learners. An online lecture-based curriculum could supplement existing models by increasing available standardised content and creating new opportunities for formal knowledge-based assessment. This modality also permits learners to self-pace their education and may help promote individualised learning. Specifically, learners could spend more time with the content that is felt to be most difficult or review content needed “just-in-time” for an encounter or procedure, stimulating motivation and reinforcing new learning. Reference Rock18 While there are some existing online resources in this field, we could not identify an existing online curriculum created specifically for advanced practice providers new to acute care cardiology.
Standardised assessment tools were also an important need, with 63.2% of programmes without a formal trainee assessment before transition to independent practice after onboarding. There are many frameworks for evaluation and assessment in medical education. Entrustable professional activities are a method for competency-based assessment where supervisors evaluate the level of supervision required to perform a specific skill by a trainee. Reference Kim, Tretter and Wilmot19 Competency-based assessment emphasises skill attainment over cumulative time spent, allowing learners to progress at different rates and focus on educational gaps. Reference McBride, Alden and Sorce10 This model has been adopted by the Accreditation Council for Graduate Medical Education and has been incorporated in residency and fellowship programmes. This could be a model for advanced practice providers. The benefits of incorporating competency-based assessments include the provision of structured curriculum scaffolding and the promotion of personalised learning.
In recent years, there have been a select number of subspecialty fellowship training programmes developed for postgraduate advanced practice providers, including in paediatric cardiology. The Advanced Practice Provider Fellowship Accreditation was created in 2022 as a credentialing body for postgraduate training programmes of advanced practice providers. Reference Brown, Cartright-Stoupe and Cato20 They promote a framework to create comprehensive programmes for advanced practice providers to obtain the knowledge and skills in their specialty area. Further development of these evidence-based fellowship programmes will likely accelerate the improvement of existing centre-specific onboarding programmes. They also offer the benefits of increased job satisfaction, increased confidence, and higher retention with associated cost savings. Reference Koppolu, Van Graafeiland and Hansen21
There are several limitations of this study. Survey submissions represent the perspectives of the individual respondent at an institution and do not necessarily reflect the broad perspectives of the respective institution nor of advanced practice providers who have completed the onboarding process, which should be a future area of investigation. While most medium to large centres are members of PAC3, this survey does not reflect the experiences of all centres nationwide. As a voluntary study, there is selection bias for those who elected to complete the survey. This was a survey-based study with possible response bias in the survey questions and the inability to explore the context of respondents’ answers. Further study with focus groups or interviews would allow for additional insights.
In conclusion, we found there is no standardised, national educational curriculum for advanced practice providers entering paediatric acute care cardiology practice. Structure, individualised learning, and team support are key themes in successful advanced practice provider onboarding. There are opportunities to develop a flexible, formalised curriculum with a structured learner assessment, which could be modified at the institutional or learner level to enhance current onboarding practices. Curriculum development is a current initiative being addressed by a task force within PAC3 in response to this needs assessment.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951125001866.
Acknowledgements
The authors would like to thank Ashley Yacobozzi of Heart University and the members of the PAC3.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.
Ethical standard
Not applicable.






