Introduction
Traumatic brain injury (TBI) presents a significant public health concern. Each year, approximately 40,000 Canadians visit the emergency room, 20,000 are hospitalized, and 3800 die following a TBI (Public Health Agency of Canada, 2020). Depending on the severity and location of the injury, residual outcomes vary, but may include functional, cognitive, behavioural, and emotional disturbances (Kinnunen et al., Reference Kinnunen, Greenwood, Powell, Leech, Hawkins, Bonnelle, Patel, Counsell and Sharp2011; Ryan and Warden, Reference Ryan and Warden2003). Such long-term challenges may partially explain why individuals who have experienced a TBI appear more vulnerable to depression (Koponen et al., Reference Koponen, Taiminen, Portin, Himanen, Isoniemi, Heinonen, Hinkka and Tenovuo2002; Perry et al., Reference Perry, Sturm, Peterson, Pieper, Bullock, Boeve, Miller, Guskiewicz, Berger, Kramer and Welsh-Bohmer2016); as many as 60% develop depression symptoms post-injury (Kim et al., Reference Kim, Lauterbach, Reeve, Arciniegas, Coburn, Mendez, Rummans and Coffey2007).
Mindfulness-based cognitive therapy (MBCT) holds promise for individuals with TBI who live with depression. This assertion is supported by accumulating evidence, including trials conducted by our own research group (Bédard et al., Reference Bédard, Felteau, Gibbons, Klein, Mazmanian, Fedyk and Mack2005, Reference Bédard, Felteau, Marshall, Dubois, Gibbons, Klein and Weaver2012, Reference Bédard, Felteau, Marshall, Cullen, Gibbons, Dubois, Maxwell, Mazmanian, Weaver, Rees, Gainer, Klein and Moustgaard2014). The core skill taught in MBCT is the ability ‘to recognize and disengage from mind states characterized by self-perpetuating patterns of ruminative, negative thought’ (Segal et al., Reference Segal, Williams and Teasdale2002; p. 74). In this way, participants are encouraged to ‘reclaim’ their lives as they accept limitations stemming from their injuries (Kangas and McDonald, Reference Kangas and McDonald2011).
As with any treatment approach for depression, MBCT may not be a good fit for everyone – not all individuals will respond to treatment the same way. Understanding the factors that are associated with a good treatment response facilitates treatment plans tailored to the individual and increases the likelihood of favourable outcomes. In considering this, several baseline characteristics have been associated with a successful response to MBCT for depression. Examples include lower severity of depression symptoms, shorter time since symptom onset, and higher mindfulness levels (Kuyken et al., Reference Kuyken, Warren, Taylor, Whalley, Crane, Bondolfi, Hayes, Huijbers, Ma, Schweizer, Segal, Speckens, Teasdale, Van Heeringen, Williams, Byford, Byng and Dalgleish2016). There is also reason to believe that characteristics like younger age (Tunvirachaisakul et al., Reference Tunvirachaisakul, Gould, Coulson, Ward, Reynolds, Gathercole, Grocott, Supasitthumrong, Tunvirachaisakul, Kimona and Howard2018) and less severe pain (Bair et al., Reference Bair, Robinson, Katon and Kroenke2003) could play a role, given their associations with success in other types of behavioural therapy for depression. Furthermore, while both men and women appear to benefit from behavioural therapy for depression, the mechanisms behind treatment success may vary by gender (Cuijpers et al., Reference Cuijpers, Weitz, Twisk, Kuehner, Cristea, David, DeRubeis, Dimidjian, Dunlop, Faramarzi, Hegerl, Jarrett, Kennedy, Kheirkhah, Mergl, Miranda, Mohr, Segal, Siddique and Hollon2014; Thase et al., Reference Thase, Reynolds, Frank, Simons, McGeary, Fasiczka, Garamoni, Jennings and Kupfer1994). This stands to reason, given our understanding of how the disorder develops and manifests differently for men and women (Nolen-Hoeksema, Reference Nolen-Hoeksema2001; Salk et al., Reference Salk, Hyde and Abramson2017).
However, with TBI, we must also consider additional layers of responders’ characteristics. For example, MBCT requirements include the cognitive ability to recognize and disengage from negative thought patterns and build emotional regulation techniques (Lubbers et al., Reference Lubbers, Geurts, Hanssen, Huijbers, Spijker, Speckens and Cladder-Micus2022; Wang et al., Reference Wang, Ren, Gao and Yu2022). Such skills call upon processes of executive function and cognitive control, which are commonly affected in individuals who have experienced a TBI (Krpan et al., Reference Krpan, Levine, Stuss and Dawson2007; Swick et al., Reference Swick, Honzel, Larsen, Ashley and Justus2012). To our knowledge, these, or any type of MBCT responders’ characteristics have yet to be explored in a population with TBI.
The current study serves to examine the characteristics of responders to an MBCT intervention within a sample with TBI. This study draws from the results of an earlier multi-site, parallel group randomized controlled trial (RCT) using a clinical sample of adults with a TBI who were experiencing depression symptoms. We explored the associations between several baseline characteristics (demographic, emotional, physical, and cognitive) and improvements in depression scores.
Method
Original research study
The analyses in the current study are based on results from a multi-site RCT previously conducted by the research team (Bédard et al., Reference Bédard, Felteau, Marshall, Cullen, Gibbons, Dubois, Maxwell, Mazmanian, Weaver, Rees, Gainer, Klein and Moustgaard2014). Inclusion criteria for this study consisted of a score of 16 or greater on the Beck Depression Inventory (BDI-II; Beck et al., Reference Beck, Steer and Brown1996), a history of TBI, ability to speak and read English, aged 18 or older, and completion of all standard treatments for their injury. Conditions that might interfere with the intervention (e.g. substance abuse, suicidal ideation) and concurrent major mental illness (e.g. schizophrenia, psychosis) constituted criteria for exclusion. Participants were initially recruited through community channels that included out-patient neurology and rehabilitation programs, brain injury associations, and health care practitioners.
Following informed consent, participants provided details on demographics (gender, age, relationship and employment status, education level); weekly alcohol intake; pain frequency (over previous 2 weeks); and years since injury. In addition to self-reporting their depression symptoms (BDI-II; Beck et al., Reference Beck, Steer and Brown1996), participants completed Likert-type measures of their mental and physical health-related quality of life (the RAND version of the Short-Form Health Survey, RAND-36; Hays et al., Reference Hays, Sherbourne and Mazel1993); mindfulness levels (Toronto Mindfulness Scale, TMS; Lau et al., Reference Lau, Bishop, Segal, Buis, Anderson, Carlson, Shapiro, Carmody, Abbey and Devins2006); and life satisfaction (Satisfaction with Life Scale, SWLS; Diener et al., Reference Diener, Emmons, Larsen and Griffin1985). Higher scores on these latter measures are considered better. A measure of psychological problems symptomology (the Global Severity Index of the Symptom Checklist-90-Revised, SCL-90; Derogatis, Reference Derogatis1994) provided insight into levels of overall psychological distress. A number of measures were used to assess facets of cognition. Specifically, the free recall portions of the California Verbal Learning Test 3 (CVLT; Delis et al., Reference Delis, Kramer, Kaplan and Ober2000) as a measure of verbal learning and memory; the Controlled Oral Word Association Test (COWAT; Benton et al., Reference Benton, Hamsher and Sivan2017) as a measure of verbal fluency; Trail-Making Tests A&B (TMT; Reitan, Reference Reitan1958) as measures of visual attention and task switching; and the Digit Span and Similarities subtests of Wechsler Adult Intelligence Scale IV (WAIS; Wechsler, Reference Wechsler1997) as measures of working memory and verbal comprehension, respectively. Except for the TMT (where scores indicate time to completion), higher scores on cognitive tests indicate better cognitive performance.
A total of 105 participants were randomized to intervention (n=57) and control (n=48) arms balanced by BDI scores, age, and sex. The MBCT intervention consisted of ten weekly 1.5-hour group sessions, with a curriculum grounded in works from Segal et al. (Reference Segal, Williams and Teasdale2013) and Kabat-Zinn (Reference Kabat-Zinn2009). Adaptations for TBI included shorter meditation sessions, more frequent review, and simplified language. The control arm participants were instructed to continue with their normal routines and were offered the opportunity to cross over and receive the intervention following their control periods.
Seventy-six participants (38 from each arm) completed post-intervention measures and were included in the parallel analysis. Results indicated that compared with the control arm, intervention participants experienced greater decreases in BDI-II scores (6.63 versus 2.13, p=0.029; d=0.56). Follow-up on intervention participants and the control arm participants who initially crossed over to receive the intervention indicated that reductions in BDI-II scores were maintained at 3-month follow-up. See Bédard et al. (Reference Bédard, Felteau, Marshall, Cullen, Gibbons, Dubois, Maxwell, Mazmanian, Weaver, Rees, Gainer, Klein and Moustgaard2014) for further details.
Current research study
For the current study, 60 participants were included. These numbers represent the 38 participants who completed the intervention arm of the original study, along with 22 of the 38 control arm participants who completed the wait period and then elected to cross over and complete the intervention. Analyses to examine baseline predictors of improvement in depression scores post-intervention were completed over two stages. First, baseline characteristics of males and females were compared utilizing t-tests and chi-square tests of independence. Second, zero-order and partial correlations were conducted to examine the relationships between baseline characteristics and change in BDI-II scores; partial correlations permitted adjustments for gender. Specifically, Pearson correlation, phi, and point-biserial correlation coefficients were calculated for continuous variables, dichotomous variables, and combinations of the two, respectively. Bootstrapped confidence intervals (95%) were computed using 1000 iterations; this included random number generation (Matsumoto and Nishimura, Reference Matsumoto and Nishimura1998) with seeding to facilitate replication. Analyses were performed using SPSS v28.
For all correlations, BDI-II scores were considered (1) as a continuous variable (BDI raw change; pre score – post score, positive scores indicate improvement), and (2) as a dichotomous variable (BDI clinically significant change, 0=not improved, 1=improved; defined as a pre–post difference that met a three-criterion standard: reliable change, a minimum 5-point reduction in BDI scores, and a reduction of BDI severity category) (Ozen et al., Reference Ozen, Dubois, Gibbons, Short, Maxwell and Bédard2016). As needed, skewed variables were transformed for the correlation analyses. First, this included the log10 of years since injury (positively skewed). Second, weekly alcohol intake (positively skewed) was transformed into categories due to large frequencies of zero values (56.7%). Categorization of weekly alcohol intake aligned with the Canadian Centre on Substance Use and Addiction (2023) recommendations: 0 drinks=no risk, 1–2=low risk of alcohol-related health consequences, 3–6=increased risk, and ≥7=significantly increased risk. Pain frequency (negatively skewed) was also categorized due to large frequencies of zero values (10.0%). Initially expressed on a visual analogue scale [from zero (not at all) to 100 (all the time)], pain frequency was transformed into four categories (<20, 21–40, 41–60, and >60).
Results
Thirty-five men and 25 women completed the intervention. Baseline characteristics for these participants are presented in Table 1 by gender. There was one statistically significant difference between male and female participants at baseline in that males reported lower levels of pain over the previous 2 weeks (47.54/100 versus 60.08/100 for females; t=–1.73, p=.044). At follow-up, BDI total scores decreased by a mean of 7.30 points (SD=8.34); half of the sample met our criteria for a clinically important change. There were no differences in BDI total score reductions between men and women [7.86 (SD=8.10) versus 6.52 (SD=8.76), t 58=0.61, p=.545]. Congruently, similar proportions of clinically important changes were observed for men and women (54.3% versus 44.0%, χ2(1)=0.62, p=.432).
Table 1. Baseline characteristics by gender with independent samples t-tests/chi-squared tests
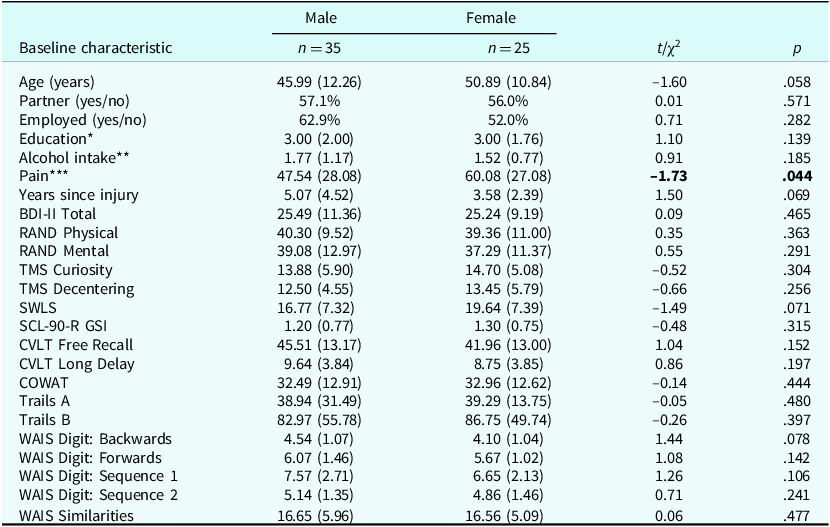
* 1, low (high school or less); 2, mid (college or some university); 3, high (university complete).
** Based on Health Canada Recommendations: 1, no risk (0 drinks/week); 2, low risk (≥2 drinks/week); 3, increased risk (3–6 drinks/week); 4, significantly increased risk (≥7 drinks/week).
*** On a scale of 0 (no pain at all) to 100 (pain all the time) over the last 2 weeks.
Zero-order correlations indicated that BDI raw change (continuous; higher scores reflect greater improvement) was negatively associated with categorized pain levels (r=–.279, 95% CI [–0.482, –0.043]) and positively associated with higher RAND physical subscale scores (r=–.286, 95% CI [0.033, 0.532]). BDI clinically significant improvement (yes/no) was also associated with higher RAND physical subscale scores (r=.324, 95% CI [0.053, 0.547]). These findings were mirrored in partial correlations (adjusting for gender): r=–.268; 95% CI [–0.477, –0.039]; r=0.284, 95% CI [0.039, 0.520]; and r pb=0.321, 95% CI [0.051, 0.542], respectively. No other baseline characteristics were associated with statistically significant change in BDI measures. See Table 2.
Table 2. Zero-order and partial correlations between baseline characteristics and change in depression symptoms
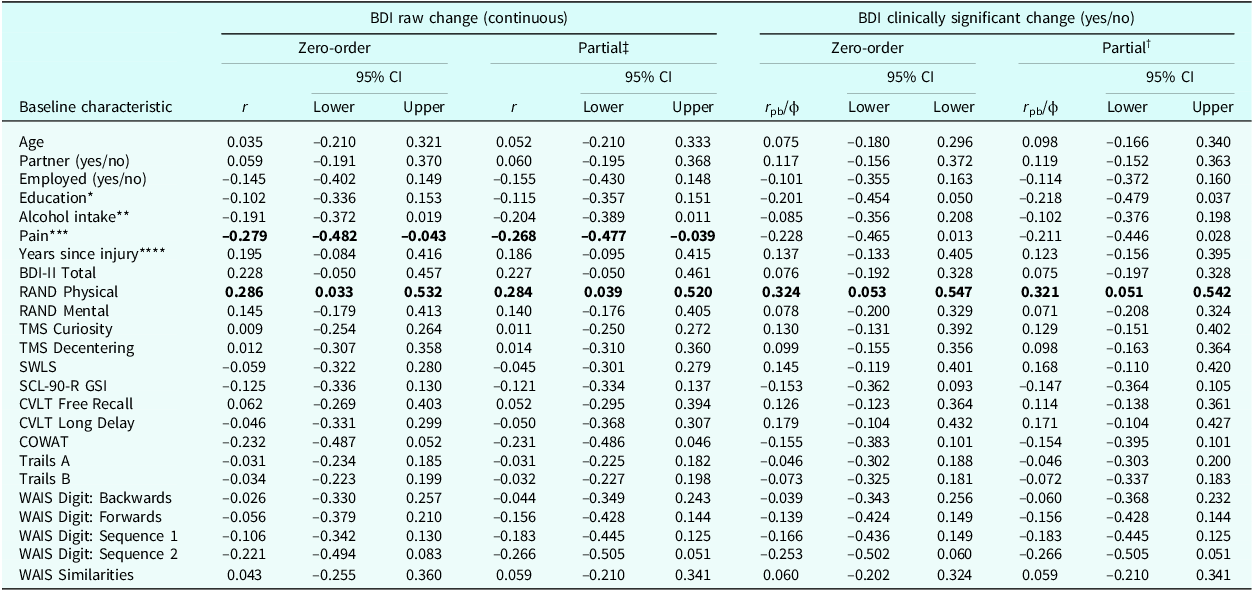
* 1, low (high school or less); 2, mid (college or some university); 3, high (university complete).
** Based on Health Canada Recommendations: 1, no risk (0 drinks/week); 2, low risk (≥2 drinks/week); 3, increased risk (3–6 drinks/week); 4, significantly increased risk (≥7 drinks/week).
*** On a scale of 0 (no pain at all) to 100 (pain all the time) over the last two weeks; intervals of <20, 21–40, 41–60, >60.
**** Log10 of years since injury.
‡ Adjusted for gender.
Discussion
The results presented here indicate that the success of an MBCT intervention for depression in a sample with TBI was largely independent of baseline factors. Of the variables examined, only higher pain levels and lower scores on the physical component of the RAND (where pain is measured) were associated with a less successful response to the intervention. This aligns with previous research showing that pain has the potential to negatively impact depression outcomes (Bair et al., Reference Bair, Robinson, Katon and Kroenke2003). While the complex, bi-directional relationship between pain and depression is beyond the scope of the current work, the recognition of this association within our sample is an important consideration for health care providers and their patients with TBI seeking to build effective treatment plans for depressive symptoms.
Women in our study reported higher levels of pain at baseline, but gender did not appear to have a strong influence on the association between pain and response to the intervention. That men and women disclose and experience pain differently, something most likely due to a mix of biological and psychosocial factors, is documented in the literature (Bartley and Fillingim, Reference Bartley and Fillingim2013). So, while our findings align with the concept that gender plays a role in pain, our findings do not support the notion that such gender differences extend to influence the relationship between pain and response to MBCT for depression. In fact, gender did not play an important role in any of the relationships between baseline characteristics and treatment response. This supports work by Cuijpers et al. (Reference Cuijpers, Weitz, Twisk, Kuehner, Cristea, David, DeRubeis, Dimidjian, Dunlop, Faramarzi, Hegerl, Jarrett, Kennedy, Kheirkhah, Mergl, Miranda, Mohr, Segal, Siddique and Hollon2014) whose meta-analysis suggested that gender does not modify successful responses to cognitive behavioural therapy for depression.
Given that TBI may involve changes in cognition and MBCT calls upon cognitive skills, the fact that our results show no relationship between baseline measures of cognitive performance and treatment response is encouraging. Our intervention did involve minor adaptations designed to support the cognitive challenges experienced by individuals who have experienced a TBI (aimed at facilitating focus, memory, and understanding). However, further research would be required to determine whether these adaptations played a role in the success of the MBCT intervention within this population.
Conclusion
Overall, this work suggests that MBCT should be considered an option for treatment of depression symptoms in most individuals with TBI. Furthermore, our results suggest that the effective treatment of pain symptoms may increase the effectiveness of MBCT for depression.
Data availability statement
The data that support the findings of this study are available from the corresponding author, H.M., upon reasonable request.
Acknowledgements
The authors wish to thank research interns Rebecca Scott and Erica Sawula for their assistance with data collection, management, and analysis.
Author contributions
Hillary Maxwell: Formal analysis (lead), Investigation (equal), Project administration (equal), Writing - original draft (lead); Sacha Dubois: Conceptualization (supporting), Formal analysis (supporting), Methodology (supporting), Writing - review & editing (equal); Dwight Mazmanian: Investigation (supporting), Methodology (supporting), Supervision (supporting), Writing - review & editing (equal); Lana Ozen: Conceptualization (supporting), Formal analysis (supporting), Writing - review & editing (equal); Carrie Gibbons: Data curation (equal), Project administration (equal), Writing - review & editing (equal); Michel Bédard: Conceptualization (lead), Funding acquisition (lead), Methodology (lead), Supervision (lead), Writing - review & editing (equal).
Financial support
Study funding was provided by the Ontario Neurotrauma Foundation (grant ABI-MIND-476); Lana Ozen was funded through post-doctoral fellowships by the Alzheimer Society of Canada and the Canadian Frailty Network (Technology Evaluation in the Elderly Network; supported by the Government of Canada through the Networks of Centres of Excellence program); Michel Bédard was funded through the Canada Research Chair Program.
Competing interests
The authors declare none.
Ethical standards
Research conformed to the Declaration of Helskini and Canada’s Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. Research Ethics Board approval was granted by St Joseph’s Care Group (2007023) and Lakehead University (106 07-08) in Thunder Bay, Ontario; the University Health Network (08-047) in Toronto, Ontario; and the Ottawa Hospital (2009 913-01H) in Ottawa, Ontario.
Key practice points
-
(1) MBCT offers a promising treatment option for most individuals experiencing depression symptoms following TBI.
-
(2) Treatment response to MBCT did not vary by cognitive impairment levels.
-
(3) As with other types of CBT, the response to MBCT may mitigated by pain levels.




Comments
No Comments have been published for this article.