Highlights:
-
• There is a lack of systematic comparative evidence linking PC settings to vaccine uptake
-
• PC strength seems important for influenza vaccine uptake, but not for COVID-19
-
• COVID-19 vaccine coverage appears to be influenced by PC spending
-
• Robust theoretical concepts needed to correctly express PC settings
1. Introduction
Vaccination is recognised as one of the major public health achievements and crucial for infectious disease management. Vaccine uptake (VU), the extent to which vaccines are utilised, is shaped by a multitude of factors, and the COVID-19 pandemic has revealed new dynamics influencing vaccine acceptance (Karafillakis et al., Reference Karafillakis, Van Damme, Hendrickx and Larson2022).
The determinants of VU frequently intersect with public health system characteristics, including the organisation of healthcare delivery, the availability of vaccine services and primary care providers, and vaccine distribution. Additionally, public trust in both the healthcare system and health professionals is widely recognised as a crucial factor influencing vaccine acceptance (Attwell et al., Reference Attwell, Rizzi and Paul2022; Zimmermann et al., Reference Zimmermann, Hagen, Braun, Rubeis and Krones2023). However, levels of trust vary significantly across countries, reflecting historical, political, and sociocultural differences in healthcare governance and public perceptions of medical institutions (Jamison et al., Reference Jamison, Quinn and Freimuth2019; Bockstal et al., Reference Bockstal, Delaruelle, Ceuterick and Bracke2021). These contextual differences, in turn, contribute to the existence of a ‘geography of VU’, where VU patterns are shaped not only by individual attitudes but also by systemic and structural factors unique to each country.
In addition, a substantial body of research has demonstrated that the factors influencing VU vary between vaccines (Verger et al., Reference Verger, Fressard and Collange2015; Dubé et al., Reference Dubé, Laberge, Guay, Bramadat, Roy and Bettinger2013; Larson et al., Reference Larson, Jarrett, Eckersberger, Smith and Paterson2014). Factors influencing the VU of the COVID-19 and influenza vaccines in 29 countries across Europe were examined in this study. These two vaccines seem to have some similar characteristics: they are not compulsory (except in Austria), remain voluntary, are mostly publicly financed and are highly recommended (not only but mainly) for the at-risk 60+ population.
A considerable number of studies regarding COVID-19 and influenza uptake have been published with inconsistent results regarding the determinants influencing VU (Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017; Graffigna et al., Reference Graffigna, Palamenghi, Boccia and Barello2020; Detoc et al., Reference Detoc, Bruel, Frappe, Tardy, Botelho-Nevers and Gagneux-Brunon2020; Karlsson et al., Reference Karlsson, Soveri, Lewandowsky, Karlsson, Karlsson, Nolvi, Karukivi, Lindfelt and Antfolk2021; Schwarzinger et al., Reference Schwarzinger, Watson, Arwidson, Alla and Luchini2021). Furthermore, other studies have examined factors influencing the intention to get both vaccines in the US (Mercadante and Law, Reference Mercadante and Law2021), Italy (Caserotti et al., Reference Caserotti, Girardi, Rubaltelli, Tasso, Lotto and Gavaruzzi2021) and Hungary (Dombrádi et al., Reference Dombrádi, Joó, Palla, Pollner and Belicza2021). All three studies indicate that people seem to better accept the COVID-19 vaccine compared to influenza vaccine.
Unlike routine vaccination programmes, the COVID-19 vaccination was characterised by unique circumstances, including the rapid development and deployment of multiple vaccine types produced by different manufactures, the unprecedented scale of vaccine distribution, and varying public perceptions of vaccine safety, effectiveness, and necessity (Attwell et al., Reference Attwell, Rizzi and Paul2022). These circumstances likely influenced VU determinants, intertwining systemic and psychological factors in novel ways. Although this study does not address vaccine-specific uptake differences, it acknowledges the role of vaccine type in shaping public attitudes and logistical challenges.
In sum, it appears that there exist both a geography of VU at the country level and that VU varies by vaccines (Verger et al., Reference Verger, Fressard and Collange2015). Determinants of VU are multifaceted, representing a confluence of individual and sociocultural determinants (MacDonald, Reference MacDonald2015), alongside economic (Walker et al., Reference Walker, Rentsch and Harris2021), logistical (Lastrucci et al., Reference Lastrucci, Lorini, Del Riccio, Gori, Bonaccorsi and Bonanni2022), behavioural (Thomson et al., Reference Thomson, Robinson and Vallée-Tourangeau2016), and systemic factors (Walker et al., Reference Walker, Rentsch and Harris2021). Still, one factor influencing vaccine acceptance remains common – the central role of health professionals, especially those involved in primary care (Karafillakis et al., Reference Karafillakis, Van Damme, Hendrickx and Larson2022). Therefore, it seems to us that the primary care (PC) system and its settings could have a decisive impact on the level of VU. The relevant literature in this area focuses primarily on the relationship of general practitioners (GPs) themselves to vaccination, recognising that they may also be vaccine-hesitant, which could influence their patients’ perceptions of vaccines. There is also a wealth of literature in paediatric care on the role of health professionals in relation to the parents (Verger et al., Reference Verger, Fressard and Collange2015; Paterson et al., Reference Paterson, Meurice, Stanberry, Glismann, Rosenthal and Larson2016).
Nevertheless, access to systematic comparative evidence examining the relationship between PC settings and VU is limited in the relevant literature. This study responds to this gap by placing particular emphasis on the role of PC settings in COVID-19 and influenza VU in 29 countries across Europe.
First, an explanation based on the literature is provided for why PC settings may be perceived as one of the factors influencing VU. Second, based on ten variables extracted from various public datasets mapping PC settings and general health system designs in 29 European countries, multiple linear regression is used to analyse the relationship between COVID-19 and influenza VU and PC settings.
2. Background
The COVID-19 pandemic highlighted the critical importance of VU in managing a global health crisis. The uptake of the COVID-19 and influenza vaccines varies from country to country. For COVID-19, 66% of the world’s population has received at least one dose of the vaccine (Mathieu et al., Reference Mathieu, Ritchie and Ortiz-Ospina2021). The majority (80%) of those who have received at least one dose of COVID-19 live in high-income countries, while only 16% of those living in low-income countries have received it (Mathieu et al., Reference Mathieu, Ritchie and Ortiz-Ospina2021). For influenza, despite widespread international policy recommendations by the World Health Assembly (Resolution WHA 56.19) to achieve 75% vaccination coverage for the 65+ age group (WHO 2009), achieving this high level of coverage remains a challenge in the European Region (only two EU countries are above 70% – Ireland and Greece – OECD 2020).
A geography of VU at the country level thus appears to exist. This means that contextual (i.e., historical, political and sociocultural) factors may play an important role in understanding vaccination acceptance, as reported by various authors (Dubé et al., Reference Dubé, Laberge, Guay, Bramadat, Roy and Bettinger2013; Jamison et al., Reference Jamison, Quinn and Freimuth2019; Larson, Reference Larson2020). To explain these variations, the MacDonald (Reference MacDonald2015) vaccine hesitancy determinant Matrix can be used. Based on the Matrix, there are three categories of determinants influencing vaccine attitudes and behaviours: (1) individual and group determinants, (2) vaccine/vaccination-specific determinants and (3) contextual determinants. The individual determinants such as risk perception, (dis)trust, gender, age, education, religion and ethnicity have been the primary focus of most studies to date (Salmon et al., Reference Salmon, Dudley, Glanz and Omer2015). Vaccine-specific determinants such as the (mandatory or voluntary) nature of vaccination, vaccination schedule, role of healthcare providers and the strength of the recommendation may be cited as examples (MacDonald, Reference MacDonald2015). The present article specifically focuses on the third category: contextual determinants of vaccine acceptance. Even if this category is less described and the theoretical as well as the empirical exploration remain scarce, there are studies stating that the contextual factors do have an impact on vaccine acceptance and confidence (Jamison et al., Reference Jamison, Quinn and Freimuth2019; Makarovs and Achterberg, Reference Makarovs and Achterberg2017). According to these authors, understanding vaccination would be challenging, if not impossible, without analysing the historical, political and sociocultural context in which it is embedded (Bockstal et al., Reference Bockstal, Delaruelle, Ceuterick and Bracke2021).
According to Bockstal et al. (Reference Bockstal, Delaruelle, Ceuterick and Bracke2021), three types of contextual factors influence vaccination: (1) outcome-specific factors (e.g., the actors involved in immunisation programmes, the affordability of vaccines and the mandatory nature of vaccines), (2) broader societal characteristics (e.g., trust in institutions, corruption, past disease exposure, unemployment, fake news on social media and in mass media) and (3) healthcare-system-specific factors (e.g., national coverage rates, trust in the healthcare system, healthcare corruption, PC systems, success of prevention programmes). Data representing all three types of contextual factors were combined to conduct this study with a specific focus on PC and general healthcare system settings, which remain the central areas of interest in the study.
PC practitioners play an important role in advocating and administrating childhood and adult vaccination. In general, healthcare workers are typically considered among the most trustworthy sources of medical information (Hesse et al., Reference Hesse, Nelson, Kreps, Croyle, Arora, Rimer and Viswanath2005). Physicians, especially GPs, are the cornerstones of vaccination implementation in most countries, and their recommendations play an influential role in their patients’ vaccine behaviour (Verger et al., Reference Verger, Fressard and Collange2015; Freed et al., Reference Freed, Clark, Cowan and Coleman2011; Schwarzinger et al., Reference Schwarzinger, Watson, Arwidson, Alla and Luchini2021). In a study covering six European countries, the GP, pharmacy and local hospital were listed as being the most trustworthy sources of health alerts or information about medicines (Paterson et al., Reference Paterson, Meurice, Stanberry, Glismann, Rosenthal and Larson2016). At the same time, GPs are often faced with situations where the risks of administering a vaccine may seem to outweigh its benefits (Ngoh and Ng, Reference Rechel, Priaulx, Richardson and Mckee2016) and/or many of them are vaccine-hesitant themselves and are, therefore, unlikely to dispel their patients’ concerns and doubts about vaccination (MacDonald, Reference MacDonald2015). This can be perceived as one of the major barriers in addressing VU in relation to the role of GPs (Graffigna et al., Reference Graffigna, Palamenghi, Boccia and Barello2020).
In summary, VU may be influenced by the PC setting and the envisioned institutional role of GP in the national immunisation programme regarding COVID-19 and influenza vaccines. Thus, the PC setting may represent a contextual determinant of VU and potentially influence vaccination rates, acceptance and confidence. This article aims to study the relationship between PC settings and the uptake of the COVID-19 and influenza vaccines in 29 European countries. Three research questions (RQs) were addressed:
RQ1 What role does the PC setting play in COVID-19 and influenza vaccination uptake?
RQ2 Is PC setting more important for influenza vaccination uptake or for COVID-19 vaccination uptake?
RQ3 What other contextual factors (Bockstal et al., Reference Bockstal, Delaruelle, Ceuterick and Bracke2021) influence influenza and COVID-19 vaccination uptake?
3. Study data and methods
3.1 Study design and data sources
This study uses a cross-sectional comparative design to analyse the relationship between primary care (PC) settings and vaccine uptake (VU) for COVID-19 and influenza across 29 European countries.
The analysis draws on secondary data from publicly available sources, including Eurostat, OECD Health Statistics, Our World in Data (OWID), and the European Health Consumer Index (EHCI). To minimise reverse causality, we selected indicators that reflect pre-pandemic or early-pandemic conditions (mainly from 2018 to 2020).
Data availability varied across countries. Where data were missing for one or more variables, listwise deletion was applied. This resulted in final analytical samples of 17 countries for the COVID-19 model and 19 countries for the influenza model.
3.2 Rationale for the selection of variables
The selection of variables was guided by previous research on PC systems (e.g. Hansen et al., Reference Hansen, Groenewegen, Boerma and Kringos2015; Kringos et al., Reference Kringos, Boerma and Bourgueil2013; Lim et al., Reference Lim, Ong, Tong, Groenewegen and Sivasampu2021), vaccination behaviour (e.g. Schwartz, Reference Schwartz2012; MacDonald and Dubé, Reference MacDonald and Dubé2015;Karafillakis et al., Reference Karafillakis, Van Damme, Hendrickx and Larson2022; MacDonald, Reference MacDonald2015; Salmon et al., Reference Salmon, Dudley, Glanz and Omer2015; Bockstal et al., Reference Bockstal, Delaruelle, Ceuterick and Bracke2021), and cross-national health policy comparisons (e.g. Burau and Blank, Reference Burau and Blank2006; Toth, Reference Toth2016).
The independent variables were grouped into three categories, based on the conceptual framework by Bockstal et al. (Reference Bockstal, Delaruelle, Ceuterick and Bracke2021):
-
• general healthcare system factors,
-
• broader societal factors, and
-
• one outcome-specific factor.
Vaccine uptake (VU) served as the dependent variable and was measured separately for COVID-19 and influenza:
-
• COVID-19 VU: the percentage of the total population that completed the initial vaccination protocol.
-
• Influenza VU: the percentage of the population aged 65 and over who received the seasonal influenza vaccine.
The general healthcare system factors included:
-
• PC spending (as a percentage of total health expenditure),
-
• number of general practitioners (GPs) per 100,000 population,
-
• GP-to-specialist ratio,
-
• strength of PC (coded as 0 = weak, 1 = medium, 2 = strong),
-
• total health expenditure (% of GDP),
-
• EHCI score (health system performance).
The broader societal variables included:
-
• share of the population with tertiary education (%),
-
• share of the population aged 65 and over (%),
-
• Gross Domestic Product (GDP, in million euros).
The outcome-specific factor was:
-
• COVID-19 vaccination policy, constructed by the authors based on national regulations, and coded as 0 (voluntary), 1 (mandatory for specific groups), or 2 (universal mandate).
All variable definitions and data sources are summarised in Table 1.
Table 1. Key measures used in the analysis
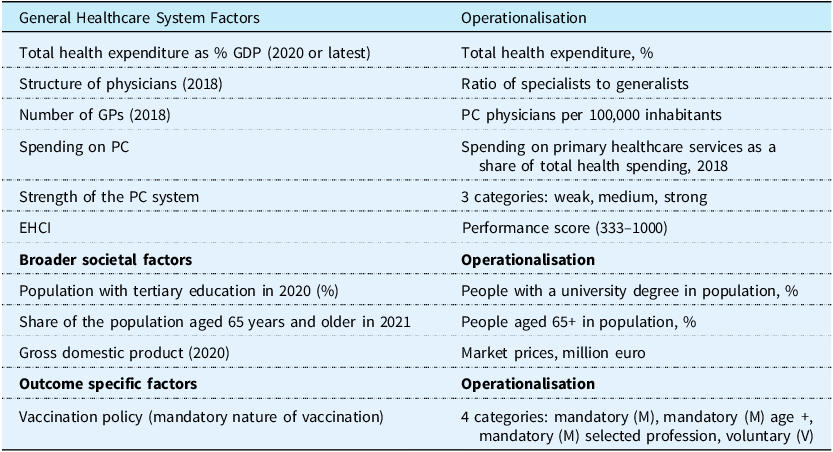
Source: Authors’ compilation based on Eurostat, OECD, OWID, EHCI and national data.
3.3 Model specification and statistical analysis
To examine the associations between contextual factors and vaccine uptake (VU), two separate multiple linear regression models were estimated: one for COVID-19 VU (defined as the percentage of the total population that completed the initial vaccination protocol) and one for influenza VU (defined as the percentage of the population aged 65 and older who received the seasonal influenza vaccine).
The general model takes the following form:
where VU i denotes the vaccine uptake rate in country i, X 1 to X k represent the contextual variables described above, and ϵ i is the error term.
As the analysis is based on a cross-sectional dataset with one observation per country, neither fixed nor random effects were applied. Given the cross-national design and potential variability in residual variances across countries, heteroscedasticity-robust standard errors were used to ensure the validity of statistical inference, particularly regarding hypothesis testing and confidence interval estimation.
All models were estimated using STATA version 17. Variables were included simultaneously (no stepwise selection was applied). Due to missing values on some independent variables, listwise deletion was used. As a result, the COVID-19 model includes 17 countries and the influenza model includes 19 countries, down from the initial pool of 29 countries.
In addition to the regression analysis, bivariate Pearson correlations were calculated to explore pairwise associations between vaccine uptake and selected explanatory variables.
4. Results
The results showed the VU of COVID-19 and influenza vaccines in 29 European countries in relation to PC settings. The findings are structured into three parts: a descriptive overview of all variables used in the models, followed by regression results from two separate multiple linear models – one for COVID-19 VU and one for influenza VU.
4.1 Descriptive overview
Table 2 presents summary statistics for all variables included in the analysis. The data show marked variation across European countries in key contextual factors that may influence VU.
Table 2. Descriptive statistics for variables related to COVID-19 and influenza VU (n = 29)
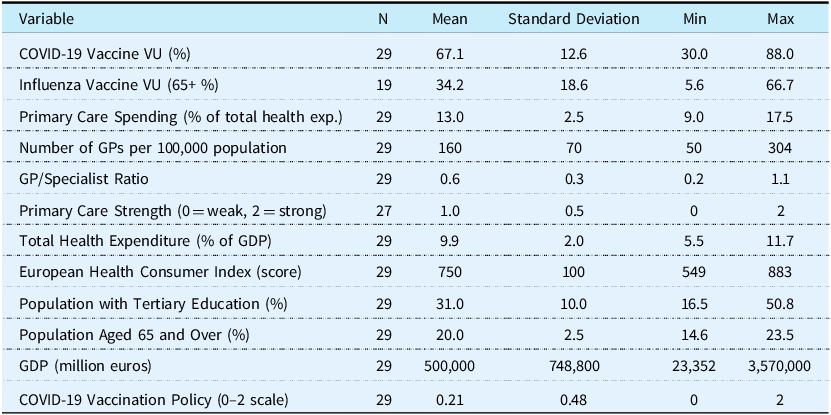
N = number of countries with available data. Influenza vaccine VU data were available for 19 countries (2019). The Primary Care Strength index was not reported for two countries, hence N = 27 for that variable. Primary Care Strength is coded 0 = weak, 1 = medium, 2 = strong. COVID-19 Vaccination Policy is coded 0 = voluntary, 1 = mandatory for specific groups, 2 = universal mandate. Data sources include OECD, Eurostat, Our World in Data, and the European Health Consumer Index.
Source: Authors’ calculations based on data from Eurostat, OECD, OWID, EHCI and national sources.
The share of the population with tertiary education ranged from 18% (Italy) to 48% (Ireland), while the proportion of the population aged 65 and over ranged from 12% (Ireland) to 23% (Italy). GDP levels also varied widely, from €23 billion in Malta to €3.5 trillion in Germany.
COVID-19 vaccination policies also differed: most countries adopted voluntary vaccination strategies, while some (e.g. Austria) implemented short-term or group-specific mandates.
4.2 Regression results: COVID-19 VU
The proportion of the population that completed the initial COVID-19 vaccination protocol served as the dependent variable in the regression model. Table 3 presents the main findings based on 17 European countries. The model showed a high adjusted R-squared (0.93), indicating that a substantial share of the variation in VU was explained by the included variables.
Table 3. Results from multiple linear regression model estimating COVID-19 VU (n = 17)
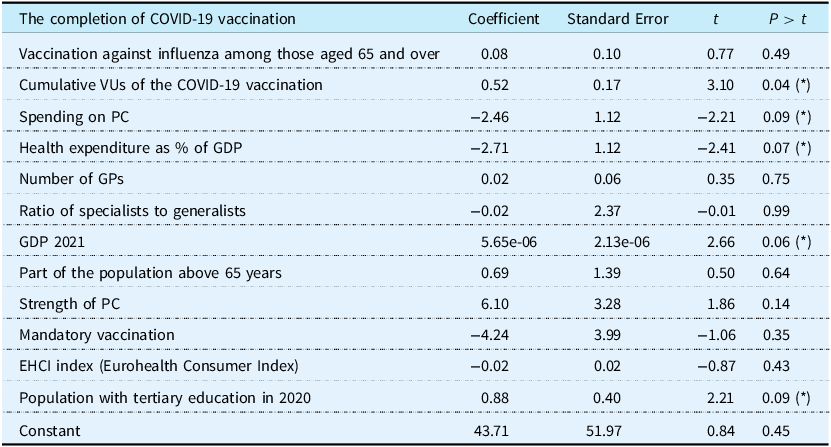
For the significant results p < 0.001 (***)/p < 0.01 (**)/p < 0.1 (*).
Number of observations (17)/(F /12, 4) = 18.01/Prob > F = 0.01/R 2 = 0. 98/Adjusted R 2 = 0. 93/Root MSE = 3.35.
The variable “mandatory vaccination” was encoded in a degressive way from mandatory to voluntary politics (voluntary = 0; mandatory = 1). Therefore, there is a negative coefficient. The strength of PC was encoded in the following way (weak = 0; medium = 1; strong = 2).
Among the tested predictors, GDP demonstrated a statistically significant and positive association with VU (β = 0.39), suggesting that wealthier countries tended to achieve higher coverage. Similarly, PC spending showed a positive and statistically significant association. However, the coefficients for other PC indicators – including the number of GPs, the ratio of specialists to GPs, and the strength of PC – were not statistically significant in the multivariate model.
Interestingly, the share of the population with tertiary education was positively correlated with VU (β = 0.42), but the effect was not statistically significant in the model. Furthermore, total health expenditure as a share of GDP showed a negative coefficient (β = –0.43), indicating that higher spending was not necessarily associated with higher VU in this context.
The strength of PC systems, as measured by the Kringos Index, showed a positive but non-significant coefficient (β = 0.40), suggesting a possible but inconclusive relationship. The variable representing mandatory vaccination policy had a negative coefficient (β = –4.24), but this effect was also not statistically significant.
Finally, the model found no specific relationship between influenza and COVID-19 VU, suggesting that past vaccination behaviour may not directly predict VU in the case of COVID-19.
To complement the regression model, bivariate Pearson correlations were calculated to explore the strength and direction of pairwise relationships between VU and individual explanatory variables. These are shown in Table 4 and visualised in Figure 1.
Table 4. Binary Correlations with COVID-19 VU (n = 29)

Source: Binary correlations obtained with the STATA (version 17).
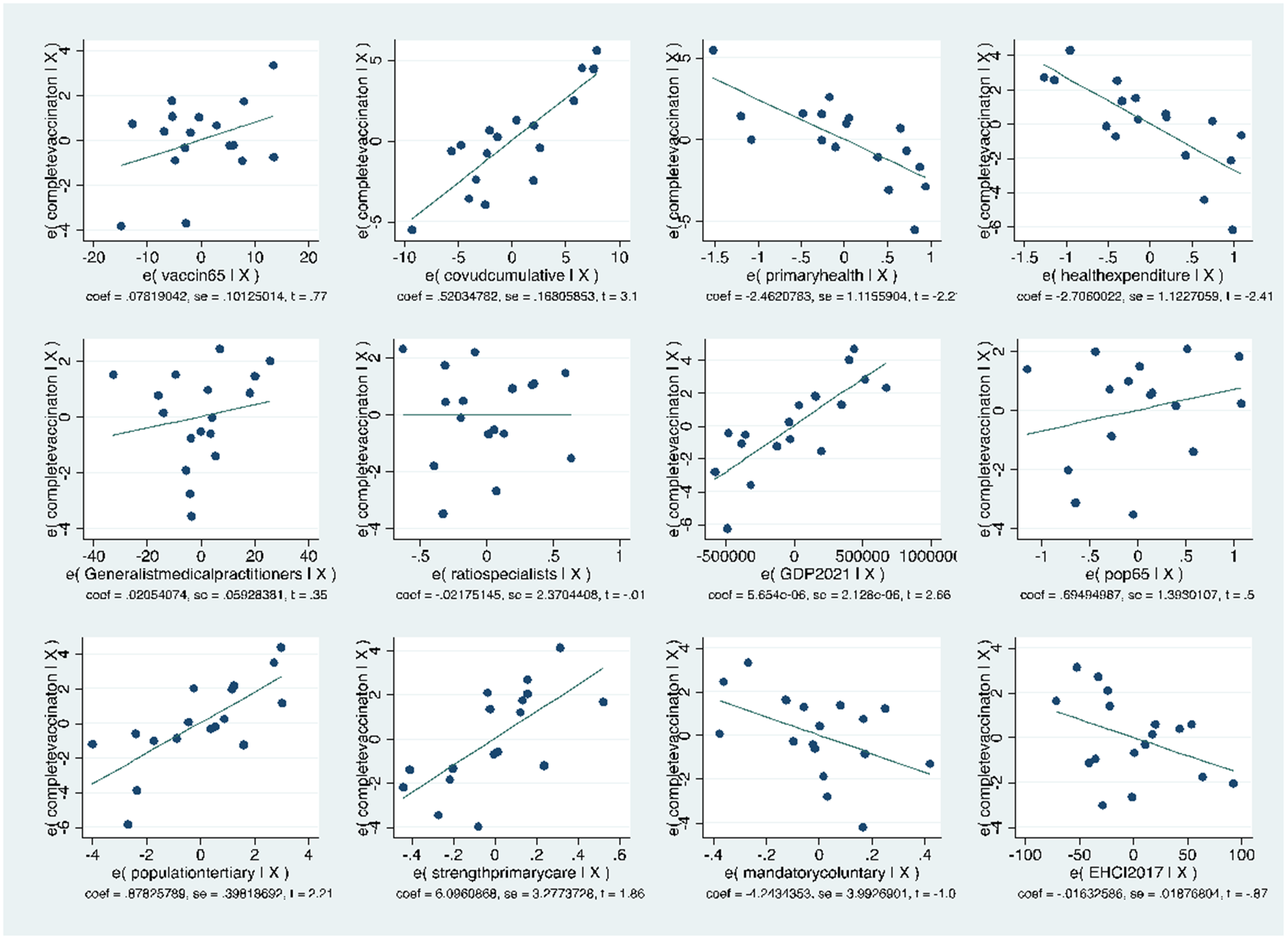
Figure 1. Binary correlations between COVID-19 vaccine uptake and selected explanatory variables (n = 29).
Source: Authors’ visualisations using STATA.
For example, COVID-19 and influenza VU were highly correlated (r = 0.77), indicating that individuals or systems open to one vaccine tended to be receptive to another. A similar positive correlation was observed between the number of GPs and COVID-19 VU (r = 0.46), even though this relationship did not remain significant in the regression model. Likewise, tertiary education was moderately correlated with VU (r = 0.42), highlighting its potential relevance at the bivariate level.
The correlations also revealed that PC spending and total health expenditure were both positively associated with VU on a bivariate level, despite having negative or non-significant coefficients in the regression model. This discrepancy may suggest interaction effects or collinearity with other variables.
Overall, the correlation analysis highlights that several variables are associated with VU in simple pairwise comparisons, even if they do not retain significance when modelled jointly.
4.3 Regression results: Influenza VU
The influenza vaccine was chosen as a comparative example to ascertain whether similar tendencies exist across different countries, as it represents a long-established and widely used vaccination practice. The first observation is that people do not behave in the same way towards COVID-19 as they do towards influenza vaccination. The regression model tested with the influenza vaccination for the population aged 65 and over revealed only one explanatory factor: the strength of PC. Table 5 presents the results of a multiple linear regression based on 19 countries with complete data. The model produced an adjusted R-squared of 0.54, indicating a moderate level of explanatory power.
Table 5. Results from multiple linear regression model estimating influenza vaccine uptake among 65+ population (n = 19)
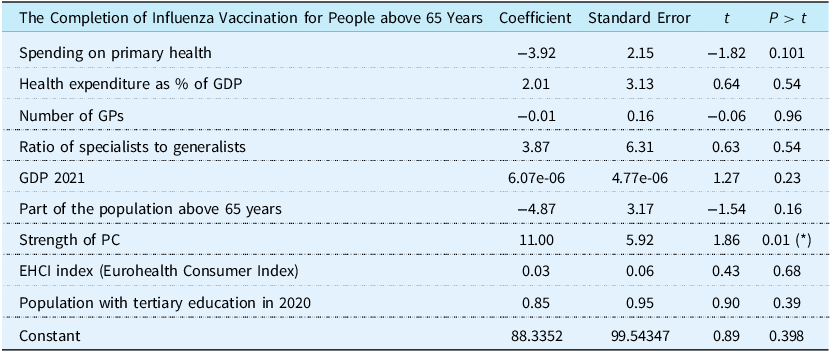
Number of observations = 19; F(9,9) = 3.38/ p > F =0.0421/R 2 =0.7715/ Adjusted R 2 = 0.5430/Root MSE = 12.231.
Countries with stronger PC had higher vaccination rates among older adults (p < 0.05). This supports the notion that robust PC systems play a key role in delivering routine vaccination programmes such as influenza.
In contrast, variables that were relevant in the COVID-19 model – such as PC spending, total health expenditure, GDP, or tertiary education – did not show significant associations with influenza VU. Moreover, cumulative COVID-19 VU was not included in the influenza model, as it is not considered an explanatory factor for this outcome.
These findings suggest a fundamental behavioural and systemic distinction between emergency vaccination campaigns (like COVID-19) and long-standing programmes such as influenza vaccination. While PC strength did not play a decisive role in COVID-19 VU, it was the key determinant in explaining uptake for influenza.
4.4 Summary of findings
The purpose of this study was to examine the relationship between PC settings and the VU of COVID-19 and influenza vaccines across 29 European countries. The results confirmed that PC settings play a role in both cases (RQ1), but also that people respond differently to the two vaccination programmes.
The main finding is that there was no direct relationship between PC strength and COVID-19 VU, whereas PC strength emerged as the only statistically significant factor associated with influenza VU (RQ2). However, in both models, some indicators reflecting PC settings were partially relevant to VU: in the case of COVID-19, it was PC spending, while in the case of influenza, it was the Kringos PC strength index. In addition, five indicators drawn from the two groups of contextual factors identified by Bockstal et al. (Reference Bockstal, Delaruelle, Ceuterick and Bracke2021) – the general healthcare system and broader societal factors – were found to play a role in influencing VU. These included PC spending, total health expenditure, PC strength, educational attainment, and GDP (RQ3). The outcome-specific factor – the nature of national COVID-19 vaccination policy – did not show a significant association with VU in the model.
A comparison of the two models highlights fundamental differences in how populations respond to emergency versus routine vaccination campaigns. In the case of COVID-19, VU was associated with GDP, educational attainment, and lower levels of health expenditure and PC spending. PC strength was not significant. For influenza, however, PC strength was the key explanatory factor, while no association was found with health expenditure or PC spending. This may suggests that robust PC systems are more influential in sustaining routine vaccination, whereas broader systemic and societal factors may drive uptake during health emergencies.
5. Discussion
Based on the belief that understanding the context in which vaccination takes place is an important determinant of VU, the study explores the contextual determinants of VU – in particular, the role of PC. The main finding is that, for COVID-19, the PC strength does not seem to be a decisive factor in increasing immunisation. However, for both COVID-19 and influenza, some of the indicators expressing PC settings were partially relevant to vaccine uptake: PC spending in the case of COVID-19 and Kringros PC strength in the case of influenza.
5.1 The predominance of extraordinary circumstances
People behave differently in the case of COVID-19 than they do in the case of influenza. Many studies (MacDonald and Dubé E, Reference MacDonald and Dubé2015; Verger et al., Reference Verger, Fressard and Collange2015; Dubé et al., Reference Dubé, Laberge, Guay, Bramadat, Roy and Bettinger2013; Larson et al., Reference Larson, Jarrett, Eckersberger, Smith and Paterson2014) have demonstrated that vaccine acceptance varies from vaccine to vaccine and that people may reject some vaccines but accept others. Our results are consistent with this. Studies focusing specifically on influenza and COVID-19 demonstrate that the uptake of annual influenza vaccination seems to be low compared to that of COVID-19 vaccination. Some studies also mention that the COVID-19 pandemic may have led to a more positive intention to vaccinate against influenza worldwide (Graffigna et al., Reference Graffigna, Palamenghi, Boccia and Barello2020; Karlsson et al., Reference Karlsson, Soveri, Lewandowsky, Karlsson, Karlsson, Nolvi, Karukivi, Lindfelt and Antfolk2021; Detoc et al., Reference Detoc, Bruel, Frappe, Tardy, Botelho-Nevers and Gagneux-Brunon2020; Schwarzinger et al., Reference Schwarzinger, Watson, Arwidson, Alla and Luchini2021; Schmid et al., Reference Schmid, Rauber, Betsch, Lidolt and Denker2017; Davis et al., Reference Davis, Vanchiere, Sewell, Davis, Wolf and Arnold2022; Kong et al., Reference Kong, Lim, Chin, Ng and Amin2022). When it comes to the determinants of VU there are no consistent results across studies. The unprecedented circumstances of the COVID-19 pandemic, coupled with the novelty and rapid development of COVID-19 vaccines, as well as the availability of multiple vaccine types from different manufacturers, likely influenced the determinants of VU. This is because VU is closely linked to public perceptions of vaccine risk, effectiveness, and safety. (Davis et al., Reference Davis, Vanchiere, Sewell, Davis, Wolf and Arnold2022).
5.2 Outcome-specific factor
The outcome-specific factor (type of COVID-19 vaccination policy) does not appear to be a determinant of VU, according to the findings of this study. However, while most countries in the study characterised their COVID-19 vaccination policy as voluntary, the practical consequences of this policy varied across countries. In some countries, voluntary vaccination was accompanied by significant public restrictions on the unvaccinated (Zimmermann et al., Reference Zimmermann, Hagen, Braun, Rubeis and Krones2023), effectively blurring the lines between voluntary and mandatory access. Conversely, Austria, which had opted for a mandatory vaccination policy for a brief period during the pandemic, never actually implemented it (Attwell et al., Reference Attwell, Rizzi and Paul2022). This stresses the necessity of considering not only the formal labelling of a policy but also its actual impacts, which may significantly influence public attitudes and behaviour concerning vaccination (Paul et al., Reference Paul, Eberl and Partheymüller2021).
5.3 Broader societal factors
Our results suggest that COVID-19 vaccination coverage is correlated with level of education and reflects overall economic performance as measured by GDP. The more a population has completed the COVID-19 vaccination, the higher the GDP and the higher the proportion of the population with tertiary education. On the contrary, our study found that neither the level of education nor GDP was a determining factor in influenza vaccination uptake.
Evidence from the literature on the influence of educational level on vaccine uptake is mixed. Some studies (Watson et al., Reference Watson, Barnsley, Toor, Hogan, Winskill and Ghani2022; Lazarus et al., Reference Lazarus, Wyka and White2023) suggest that better education generally leads to higher vaccine acceptance in the population. Others have found the opposite trend (i.e., that VH is associated with lower levels of education - Dubé et al., Reference Dubé, Laberge, Guay, Bramadat, Roy and Bettinger2013). Other studies have found no association between education and VH (Jamison et al., Reference Jamison, Quinn and Freimuth2019; Lim et al., Reference Lim, Ong, Tong, Groenewegen and Sivasampu2021).
It seems that there may be an association with the type of vaccine. Studies show that the decision not to vaccinate against influenza may be associated with lower levels of education (Takayama et al., Reference Takayama, Wetmore and Mokdad2012; Damiani et al., Reference Damiani, Federico, Visca, Agostini and Ricciardi2007), while the opposite pattern has been found for willingness to vaccinate against COVID-19 – the more educated people are, the more willing they are to vaccinate against COVID-19 (Kreidl et al., Reference Kreidl, Šťastná, Kocourková, Dzúrová, Hamanová, Zvoníček and Slabá2021). The latter is consistent with the results of our study suggesting that the more educated people are, the more likely they are to be vaccinated in exceptional circumstances such as during a COVID-19 pandemic.
Regarding GDP, our study suggests that richer societies tend to have better VU in exceptional pandemics. The results of studies in this area are scarce and therefore difficult to compare. However, some studies highlight the important role of national income in determining the uptake of the COVID-19 vaccine (Moradpour et al., Reference Moradpour, Shajarizadeh, Carter, Chit, Grootendorst and Afoakwah2023). Furthermore, some studies consider both GDP and education levels, claiming that education is the most important factor in expanding the campaign and that the economic strength of economies leads to higher vaccination rates (Ngo et al., Reference Ngo, Zimmermann, Nguyen, Huynh and Nguyen2022).
Some studies mention that younger age groups are less likely than older age groups to have positive vaccination views, while others (Dubé et al., Reference Dubé, Laberge, Guay, Bramadat, Roy and Bettinger2013) found that opposition to vaccination was found more frequently among older people (aged 50–64). This generational perspective is important but was not verified in our model.
5.4 General health system factors
For COVID-19, there is a correlation between the resources allocated both to the health system as a whole and directly to PC and the proportion of the population who have received the vaccine. In the case of COVID-19, the lower the expenditure on the health system and PC, the higher the vaccination coverage. For influenza, on the other hand, no relationship was found between the total health expenditure, PC spending and vaccination coverage. The results of studies in this area are limited, but studies show an association between vaccination rates and health expenditure (Castillo-Zunino et al., Reference Castillo-Zunino, Keskinocak, Nazzal and Freeman2021; Monrad et al., Reference Monrad, Quaade and Powell-Jackson2022).
Some studies mention that willingness to vaccinate correlates with access to healthcare during the COVID-19 crisis, suggesting a strong synergy between health system performance during the crisis and vaccine promotion. In our study, no relationship was found between vaccination coverage and health system performance (measured by the EHCI) for either COVID-19 or influenza.
The strength of PC – the main focus of our study – was found to be highly important in relation to influenza vaccination rates, but no association was found for COVID-19.
This discrepancy may be attributed to the pivotal role of public health agencies during the pandemic, as they organised mass vaccination campaigns and utilised their infrastructure for the rapid distribution of vaccines. As a result, the influence of PC seems to be neglected in the exceptional circumstances caused by the COVID-19 pandemic. Given that trust in healthcare professionals is a well-documented determinant of VU (Hilton et al., Reference Hilton, Hunt, Langan, Bedford and Petticrew2011, Zimmermann et al., Reference Zimmermann, Hagen, Braun, Rubeis and Krones2023), the limited involvement of PC settings may represent a missed opportunity to capitalise on established relationships between patients and GPs.
Furthermore, our findings revealed the relative invisibility of GPs in both COVID-19 and influenza vaccination, with their influence not emerging as a decisive factor in either case. This is particularly striking given the expectation that GPs, due to their long-standing relationships with patients and ability to provide tailored vaccine recommendations, would play a central role in facilitating VU. While people tend to trust their GPs and value their medical guidelines, the pandemic health restrictions – such as limited mobility and reduced contact with GPs – must be considered as potential modifiers of GPs influence on vaccine decision-making.
In the early stages of the COVID-19 vaccination rollout, mass vaccination centres became the primary sites of administration, potentially limiting GP-patient interactions and thereby reducing the immediate impact of GP on VU. However, as the pandemic progressed and vaccination strategies shifted from emergency response to routine healthcare delivery, a transition occurred from specialised vaccination centres back to standard medical practice, allowing GPs to regain their role in supporting VU (Dubé and MacDonald, Reference Dubé and MacDonald2022).
As demonstrated by qualitative research (e.g. Brabin et al., Reference Brabin, Roberts, Stretch, Jackson, Elton and Baxter2011), variability in vaccine uptake can be partly explained by organisational factors. In case of COVID-19, the vaccination setting itself may also be a key explanatory factor. While individuals predominantly receive the influenza vaccine in GP practices (Rechel et al., Reference Rechel, Priaulx, Richardson and Mckee2019; Palmer, Reference Palmer2022), the COVID-19 vaccines were more frequently administered in temporary vaccination centres, specifically established for this purpose. Surprisingly, our findings suggest that even for influenza, GPs did not appear to be significantly associated with successful vaccination campaigns, contradicting existing literature on the role of PC in facilitating vaccine acceptance.
This inconsistency is of particular interest given the numerous studies that emphasise the pivotal role of GPs in addressing VU. In some, the increasing number of GPs is seen as an important tool for addressing people’s doubts about vaccine efficacy (Verger et al., Reference Verger, Fressard and Collange2015). Others suggest that GPs play a critical role in ensuring VU, possibly through counselling and building trust and partnerships with their patients in the local community (Wilkinson et al., Reference Wilkinson, Jetty, Petterson, Jabbarpour and Westfall2021). However, some studies argue that there is a lack of empirical evidence on the impact of a PC-led approach to vaccine distribution on VU and equity (Aggarwal et al., Reference Aggarwal, Kokorelias, Glazier, Katz, Shiers-Hanley and Upshur2023).
In conclusion, the contextual factors of COVID-19 and influenza vaccine uptake were examined. The key factor in the study – PC settings, consisting of spending on PC, the number and structure of GPs and the Kringos strength of PC (Kringos et al., Reference Kringos, Boerma and Bourgueil2013) – was found to influence vaccine uptake only partially and never as a whole. The interpretation of this result should take into account the different roles of GPs in vaccination between national contexts and types of vaccination, the unique circumstances of the COVID-19 pandemic and other contextual factors not studied here. In particular, the role of trust – whether in individual healthcare providers, the broader health system, or public health messaging – remains a crucial element warranting further investigation (Bockstal et al., Reference Bockstal, Delaruelle, Ceuterick and Bracke2021; Zimmermann et al., Reference Zimmermann, Hagen, Braun, Rubeis and Krones2023). Simultaneously, further research is needed to discuss which indicators are appropriate to express PC settings. The message is that systematic comparative evidence on the relationship between PC and vaccine uptake could help researchers better understand the different factors influencing vaccination behaviour.
5.5 Limitations of the study
This study was conducted in Europe, where the contrast between countries with efficient health systems and others with less efficient systems may not be as obvious from a global perspective. From a European perspective, however, the study includes data from 29 European countries and may not fully capture the diversity of individual health care systems, which could result in an oversimplification of national contexts. Furthermore, the study does not distinguish between the different types of available vaccines, which may have affected VU. The selection of PC indicators was based on established frameworks but did not include all potential dimensions of PC on VU. Multiple linear regression analysis is useful to capture some trends so that further studies can ask about the relationship between PC profile and VU.
6. Conclusion
This study examined the relationship between primary care (PC) settings and vaccine uptake (VU) for COVID-19 and influenza across 29 European countries. PC settings were operationalised using four indicators: spending on PC, the number and structure of general practitioners (GPs), and the Kringos index of PC strength. Our findings suggest that PC settings influence VU only partially, with no single indicator consistently shaping uptake across both vaccines. Instead, different aspects of PC were relevant: PC spending was more influential for COVID-19 vaccination, whereas PC strength played a greater role in influenza vaccine uptake.
These findings have important implications for health policy and research. First, there is a need to establish a robust theoretical framework to determine which indicators best capture the role of PC in vaccination efforts. Second, further research on the relationship between PC settings and VU could enhance our understanding of the broader determinants influencing vaccination behaviour.
While PC plays a crucial role in routine immunisation programmes such as influenza vaccination, its impact on emergency vaccination efforts appears more limited. Policymakers should consider strategies to better integrate PC into future pandemic preparedness plans, particularly by leveraging the trust between general practitioners and their patients. Future research should explore how PC can be more effectively incorporated into vaccination campaigns to maximise vaccine uptake across diverse healthcare systems.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1744133125100108
Acknowledgements
We would like to thank to Markéta Páleníková for her support during different phases of the research.
Financial support
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 965280.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethic statement
Not applicable.








