During childhood, a substantial number of children are exposed to potentially traumatic events, such as domestic violence, natural disasters and sexual abuse. In 2007, Copeland and colleagues Reference Copeland, Keeler, Angold and Costello1 reported that more than two-thirds of children have experienced at least one potentially traumatic event. Similarly, Lewis and colleagues Reference Lewis, Arseneault, Caspi, Fisher, Matthews and Moffitt2 found that 31% of children had experienced such events, and Alisic and colleagues Reference Alisic, van der Schoot, van Ginkel and Kleber3 reported a rate of 14%. Although it is evident that not all trauma-exposed children and adolescents actually develop post-traumatic stress disorder (PTSD), prevalence estimates for PTSD vary considerably, depending on the study sample, the assessment methods employed and the type of events evaluated.
PTSD is associated with serious personal and societal health burdens. Children and adolescents with PTSD are at increased risk of comorbid physical and psychiatric disorders, self-harm, functional impairment in school and family dynamics, and suicidality. Reference Lewis, Arseneault, Caspi, Fisher, Matthews and Moffitt2,Reference Luoni, Agosti, Crugnola, Rossi and Termine4,Reference Panagioti, Gooding, Triantafyllou and Tarrier5 Comorbid psychopathology is often maintained or worsened by untreated PTSD, and the prognosis for recovery without adequate treatment is poor. Reference Meiser-Stedman, Smith, Yule, Glucksman and Dalgleish6,Reference Norton, Barrera, Mathew, Chamberlain, Szafranski and Reddy7 Insight into current PTSD prevalence rates could sharpen awareness of the risk of onset after potentially traumatic events, as well as recognition of the disorder’s debilitating effects. Such knowledge would enhance the early detection of trauma-related symptoms in children and adolescents.
Evolving PTSD prevalence estimates
The most recent meta-analysis by Alisic and colleagues, Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 which included more than 70 studies published between 1994 and 2012, estimated that approximately 16% (95% CI 8–33%) of children and adolescents develop PTSD after exposure to a potentially traumatic event. Since the publication of that analysis in 2012, many new studies have been conducted on PTSD prevalence in children and adolescents. More advanced meta-analytic strategies have also become available that can deliver refined prevalence estimates. Moreover, revised diagnostic criteria for PTSD were adopted in 2013 in the new DSM-5. 9 It introduced significant changes in the symptom structure and symptom criteria for PTSD, including removal of the A2 stressor criterion and the expansion of symptom clusters. 9,10 The revised diagnostic criteria have also been described as more developmentally sensitive. Reference De Young and Landolt11 The impact of these changes on prevalence rates is ambiguous, with studies yielding mixed results. Although some studies suggest that the broader criteria in DSM-5 have led to higher prevalence rates in certain age groups, Reference Mikolajewski, Scheeringa and Weems12 other studies report minimal differences in PTSD between the DSM-IV and DSM-5. Reference Sims, Scheeringa and Mikolajewski13
Study rationale and objectives
A meta-analytic review that incorporates these developments had yet to be conducted. Acquiring more precise estimates of PTSD prevalence rates among children and adolescents can enhance the allocation of mental health resources, thereby improving efficiency. Such estimates are also crucial for informing early intervention strategies for young individuals who have experienced potentially traumatic events. Moreover, an updated meta-analysis will illuminate the potential effects of the revised PTSD diagnostic criteria introduced in DSM-5. By periodically updating prevalence rates using meta-analytic strategies, researchers can also track long-term trends in PTSD prevalence. This is crucial for understanding whether the incidence of PTSD is increasing, decreasing or stabilising over time, and why such trends occur.
Our aim is, therefore, to provide an updated estimation of PTSD rates among trauma-exposed children and adolescents by combining the studies identified in the 2012 meta-analysis Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 with those published since 2013 into a single database. We analyse PTSD according to both DSM-IV and DSM-5 criteria. Similarly to the analysis by Alisic et al, we test whether the prevalence estimate shows variability across the moderators type of traumatic event, gender, informant of the assessment and choice of diagnostic method. The findings of Alisic et al Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 reflect how differences in type of traumatic event and gender significantly influences PTSD prevalence estimates. This aligns with other meta-analytic work in youth. Reference Dai, Liu, Kaminga, Deng, Lai and Wen14–Reference Woolgar, Garfield, Dalgleish and Meiser-Stedman16 No significant moderating effect was found in the work of Alisic et al Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 for the assessment informant and choice of diagnostic method, adding to a mixed body of findings. Reference Rezayat, Sahebdel, Jafari, Kabirian, Rahnejat and Farahani17, Reference Meiser-Stedman, McKinnon, Dixon, Boyle, Smith and Dalgleish18 We also assess time since trauma exposure as an additional possible moderator affecting the PTSD prevalence estimate, as research in both adults and children suggests that prevalence rates tend to decline around 3 months following trauma exposure. Reference Diamond, Airdrie, Hiller, Fraser, Hiscox and Hamilton-Giachritsis19,Reference Hiller, Meiser-Stedman, Fearon, Lobo, MacKinnon and Fraser20
Method
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines for systematic reviews and meta-analyses, Reference Moher, Liberati, Tetzlaff and Altman21 and was registered with PROSPERO (registration number CRD42024522041).
Search strategy
Building on the previous search by Alisic et al, Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 we conducted a systematic literature search across five databases: PsycINFO (Ovid), Medline (Ovid), EMBASE (Ovid), the Web of Science Core Collection and PTSDpubs (ProQuest). The complete search syntax for each database is available in the Supplementary Material (available at https://doi.org/10.1192/bjp.2025.30), under Search Strategy. In addition, we searched the reference lists of relevant reviews Reference Dai, Liu, Kaminga, Deng, Lai and Wen14,Reference Woolgar, Garfield, Dalgleish and Meiser-Stedman16,Reference Rezayat, Sahebdel, Jafari, Kabirian, Rahnejat and Farahani17,Reference Blackmore, Boyle, Fazel, Ranasinha, Gray and Fitzgerald22 to ensure comprehensiveness, but no additional suitable records were found. Duplicates were removed, and the researchers I.V. and H.D. independently screened titles and abstracts of all remaining records for eligibility, using the web application Rayyan (Rayyan, Cambridge, MA, USA; www.rayyan.ai). Reference Ouzzani, Hammady, Fedorowicz and Elmagarmid23 Full-text articles were retrieved for all potentially eligible records, and these were then independently reviewed by I.V. and H.D. If eligibility remained unclear, the primary study authors were contacted to obtain additional information. Throughout the screening process, any disagreements and questions were resolved by consulting at least one senior member of the research team (M.v.d.M., R.K., I.H. and R.J.L.L.).
Selection criteria
We included all records previously identified by Alisic et al Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 between 1996 and 2012, except for four records that did not meet the inclusion criteria upon review. For our own search for studies published from January 2013 to February 2024, we restricted our selection to empirical studies that had undergone peer review and were reported in English. The search was conducted on 8 February 2024. Following the Alisic approach, we focused on studies that had adopted one of the following diagnostic interviews to assess PTSD: Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA); Anxiety Disorders Interview Schedule for DSM-IV, Child Version; Diagnostic Interview for Children and Adolescents (DICA); Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version (K-SADS) and Children’s PTSD Inventory (CPTSDI). Primary study results were eligible for inclusion if they were obtained via interviews based on the PTSD criteria described in either the fourth or fifth edition of the DSM. In addition, given the DSM-5 inclusion of a new subtype called ‘pre-school PTSD’, studies based on the Diagnostic Infant and Preschool Assessment were also deemed eligible.
Furthermore, and in line with the Alisic et al meta-analysis, Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 our studies had to meet the following criteria: (a) the study sample was based on at least ten participants; (b) all participants had been exposed to a potentially traumatic event according to the A1 criterion for PTSD in DSM-IV or the A criterion in DSM-5, or separate data were available on trauma-exposed participants; (c) the study participants were aged 18 years or younger at time of PTSD assessment; (d) the participants were not part of a mental health clinical population, such as patients referred for psychiatric care; (e) the PTSD diagnostics were performed at least 1 month after the trauma; (f) psychometric evaluation of the diagnostic interview was not the sole purpose of the study; (g) the primary study was not an intervention or effectiveness study; and (h) the article and/or the study authors provided sufficient information to extract or calculate the percentage of participants meeting the criteria for PTSD diagnosis. See Fig. 1 for the complete flowchart of the selection process. The studies identified in our latest search underwent independent quality assessments by I.V. and H.D., using the Joanna Briggs Institute critical appraisal tools. 24 All studies were deemed satisfactory in accordance with their respective critical appraisal checklists (see Tables S3–6, available in the Supplementary Material).
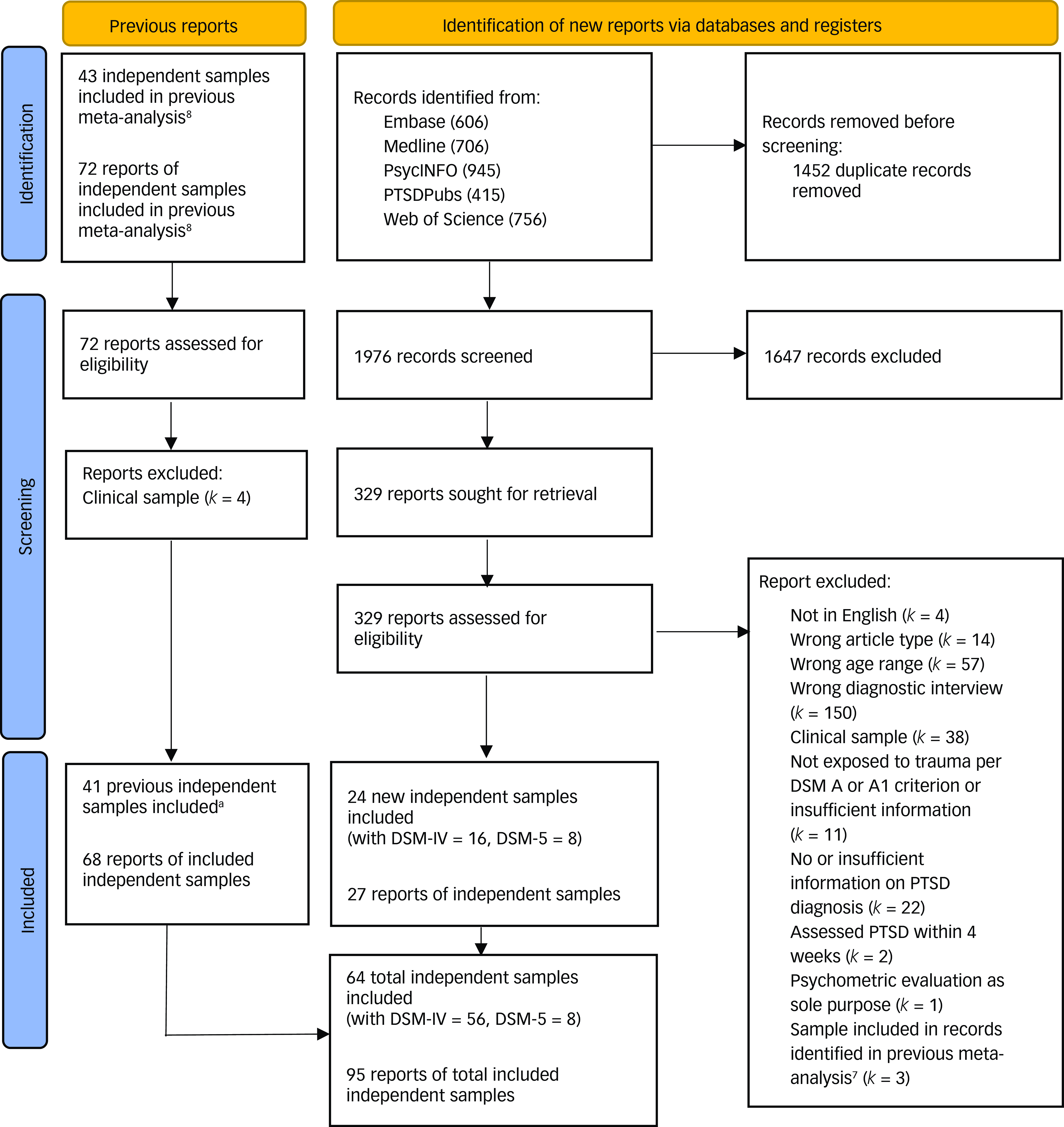
Fig. 1 Flowchart of selection process. PTSD, post-traumatic stress disorder.
a. In Alisic et al’s article,Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 one report was considered to consist of two independent samples. However, we treated and thus counted these two samples as one, because of our multilevel meta-analytic approach.
Data extraction
For each study previously identified by Alisic et al Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 and for those identified in our latest search, we extracted data on sample characteristics, trauma exposure, PTSD assessment method and PTSD assessment results (the complete coding manual is available from the author I.V.). We maintained separate files for data from studies applying the DSM-IV criteria and those applying the DSM-5 criteria. Data extraction was conducted on 5 April 2024. In terms of sample characteristics, we recorded the country of data collection, sample size, mean age of the sample (s.d. and age range), percentage of boys in the sample and exclusion criteria applied by the primary study authors, such as cognitive impairments, insufficient language skills and current medication use. As for trauma exposure, we first coded details of the traumatic event. Next, we classified the trauma exposures into three categories: ‘interpersonal trauma’, ‘non-interpersonal trauma’ or ‘varied types’. We also recorded the time since trauma exposure in mean number of weeks (and week range), and created a discrete variable with the categories ‘3 months or less since exposure’ and ‘more than 3 months since exposure’. This categorisation was based on research on both adults and children that suggests a decrease in prevalence 3 months post-trauma. Reference Diamond, Airdrie, Hiller, Fraser, Hiscox and Hamilton-Giachritsis19,Reference Hiller, Meiser-Stedman, Fearon, Lobo, MacKinnon and Fraser20 Regarding the PTSD assessment, we recorded the informant type and the type of diagnostic interview used. Finally, we recorded the proportion of individuals who satisfied the criteria for a PTSD diagnosis. If the study authors had provided prevalence data for boys and girls separately, both were extracted.
In case of missing information, we contacted the study authors, whereby most but not all responded. All data extraction was carried out by two members of the research team (I.V. and H.D.). There was a full consensus on all coding. The characteristics of all included studies are presented in Supplementary Tables S1 and S2.
Table 1 Results of moderator analyses for DSM-IV meta-analysis

Number of studies refers to the number of studies with independent samples; level-2 residual variance refers to residual variance in effect sizes within studies; level-3 residual variance refers to residual variance in effect sizes between studies. PTSD, post-traumatic stress disorder; CAPS-CA, Clinician-Administered PTSD Scale for Children and Adolescents; ADIS, Anxiety Disorder Interview Schedule; DICA, Diagnostic Interview for Children and Adolescents; K-SADS, Kiddie Schedule for Affective Disorders and Schizophrenia; CPTSDI, Children’s PTSD Inventory.
a Omnibus test of all regression coefficients in the model.
b P-value of the omnibus test.
c The Diagnostic Infant and Preschool Assessment was not included in the moderation analyses because its discrete category included fewer than five effect sizes.
*P < 0.05, **P < 0.001.
Statistical analysis
We used two separate, three-level random-effects models to estimate two overall prevalence rates (separately for DSM-IV and for DSM-5 data), and used test variables as moderators of each overall rate. As this approach enabled the modelling of effect size dependency, multiple relevant effect sizes could be extracted from individual primary studies (for example, for each type of trauma exposure), if these were reported. Effect size dependency was modelled by assigning a random effect to studies at level 3 of the model and to effect sizes within studies at level 2 of the model, enabling three sources of variance to be considered: (a) sampling error of the observed effect sizes, (b) variance in effect sizes within studies and (c) variance in effect sizes between studies. These three-level meta-analyses were performed in R version 4.2.3 for Windows (R Core Team, Vienna, Austria; www.R-project.org), using the metafor package Reference Viechtbauer25 and following the syntax defined by Assink and Wibbelink. Reference Assink and Wibbelink26
In the event of heterogeneity in effect sizes – which was determined by conducting two separate log-likelihood ratio tests that assessed the significance of the within-study and between-study variance components – we then conducted moderator analyses to evaluate whether (a) gender, (b) type of traumatic event, (c) time since trauma exposure, (d) informant of the assessment or (e) type of diagnostic interview could explain the variance in effect sizes. The results of our moderation analyses were obtained by extending a three-level intercept-only model with potential moderating variables as covariates. Each extracted prevalence was transformed to a t-value, using the double arcsine method as described by Barendregt et al. Reference Barendregt, Doi, Lee, Norman and Vos27 After analyses, the t-values were transformed back into prevalence proportions by using the inverse of the transformation. Reference Barendregt, Doi, Lee, Norman and Vos27 Further, to examine whether and how the results might have been affected by publication bias, we performed an Egger’s regression test Reference Egger, Davey Smith, Schneider and Minder28 that was adapted for three-level meta-analysis, followed by an adapted trim-and-fill procedure. Reference Fernandez-Castilla, Declercq, Jamshidi, Beretvas, Onghena and Van den Noortgate29 We also visually examined a funnel plot that displays effect sizes against the standard error surrounding an estimated summary effect.
Results
In total, we extracted data from k = 95 primary studies, which reported on 64 independent samples and yielded u = 104 effect sizes. Overall characteristics of all included studies can be found in the Supplementary Material (Supplementary Tables 1 and 2).
Study characteristics
For the DSM-IV meta-analysis, we included 56 independent samples (sample sizes ranging from 16 to 435), of which 16 were identified in the current search and 40 were drawn from the previous meta-analysis. These samples were examined in k = 87 primary studies that produced u = 94 effect sizes. These studies reported on 6745 children and adolescents that underwent PTSD assessments. The study samples comprised 48% girls, with four studies that included boys or girls exclusively. The sample ages ranged from 2 to 18 years. The independent samples predominantly originated from North America (n = 24), followed by Europe (n = 20), Oceania (n = 5), the Middle East (n = 3), Asia (n = 2), Africa (n = 1) and South America (n = 1). Children and adolescents in the included samples had been exposed to various types of trauma, such as abuse, accidental injury, wartime experiences or the sudden loss of a parent. Participants in 22 samples (39%) had experienced one or more non-interpersonal traumas; in 20 samples (36%), they had experienced one or more interpersonal traumas; and in 14 samples, participants had experienced either or both types (25%). In 13 samples (23%), all participants had undergone their most recent trauma exposure in the 3 months before the PTSD assessment; in 21 samples (38%), more than 3 months had elapsed; and in 22 samples (39%), the timing was unclear. In the majority of independent samples, PTSD assessment interviews were held with the children and adolescents directly (n = 36; 64%). The most frequently used diagnostic interview was the CAPS-CA (n = 21; 36%). Reported PTSD prevalence estimates varied from 0 to 89%.
For the DSM-5 meta-analysis, we included eight independent samples (sample sizes ranging from 79 to 11 877) examined in k = 8 studies that produced u =10 effect sizes. These studies examined 12 644 children and adolescents that had undergone PTSD assessments, 49% of whom were girls. The ages of the participants ranged from 1 to 18 years. The independent samples predominantly originated from Europe (n = 4), followed by North America (n = 3) and the Middle East (n = 1). The sampled children and adolescents had been exposed to various types of trauma, such as abuse, accidental injury, wartime experiences or parental loss. In four samples (50%), participants had experienced non-interpersonal trauma; in two samples (25%), participants had undergone interpersonal trauma; and two other samples (25%) reported varied types. In one sample (13%), the most recent trauma exposure had been in the 3 months before to the PTSD assessment; in three samples (38%), more than 3 months had elapsed; and in four samples (50%), the timing was unclear. In the majority of independent samples, PTSD assessment interviews were held directly with the parent (n = 3; 38%) or with parent and child together (n = 3; 38%). The K-SADS was most often used as the diagnostic interview (n = 5; 63%). Prevalence estimates for reported PTSD ranged from 3 to 51%.
Overall PTSD prevalence
Where DSM-IV criteria were applied, the estimated PTSD prevalence rate among trauma-exposed children and adolescents was 20.3% (95% CI 14.9–26.2), with 56 independent samples and 94 effect sizes. For inspection of the forest plot, see Figure S1 in the Supplementary Material. We found significant within-study variance (level 2, χ 2(2) = 87.83, P < 0.001) and between-study variance (level 3, χ²(2) = 21.02, P < 0.001), based on log-likelihood ratio tests, thus indicating effect size heterogeneity. Of the total amount of effect size variance, 30.62% could be attributed to within-study differences in effect sizes (level 2; differences relating to assessment informant and interview schedules for example), 65.22% to between-study differences (level 3) and 4.16% to sampling variance (level 1). Given this heterogeneity, it was deemed justified to proceed with bivariate moderator analyses to identify variables that might explain effect size variability.
Where DSM-5 criteria were applied, the estimated PTSD prevalence rate was 12.0% (95% CI 3.7–24.2), with eight independent samples and ten effect sizes. For inspection of the forest plot, see Figure S2 in the Supplementary Material. Of the total amount of effect size variance, 0% could be attributed to within-study effect size differences (level 2), 96.16% to between-study differences (level 3) and 3.84% to sampling variance (level 1). We found no significant heterogeneity either for within-study variance (level 2, χ²(2) = 0, P > 0.999) or for between-study variance (level 3, χ²(2) = 3.40, P = 0.065), using log-likelihood ratio tests. Moreover, given the small number of included studies, most categories of the coded discrete variables were based on fewer than five effect sizes. As estimations would have likely been unreliable from analysing such a minimal amount of information per category, moderator analyses were not performed for the DSM-5 meta-analysis.
Moderator analyses
We conducted moderator analyses with the DSM-IV data to investigate the potential influence of gender, type of trauma, time since trauma exposure, type of informant and type of diagnostic interview on the overall estimated PTSD prevalence. Table 1 summarises the results of those analyses.
We found significant moderating effects for gender (F(1, 83) = 8.44, P = 0.005), type of trauma (F(2, 88) = 5.30, P = 0.007) and type of diagnostic interview (F(4, 86) = 8.22, P < 0.001). Specifically, there was a significant moderating effect for gender in the sense that primary studies reported lower PTSD prevalence rates as the percentage of boys in the samples increased. Further, in testing discrete variables as moderators, we compared each category against a reference category to test for differences in PTSD prevalence rates. As for trauma type, the PTSD prevalence rate was significantly lower for non-interpersonal trauma (11.8%) than for interpersonal trauma (32.1%), but it did not differ significantly between children with interpersonal trauma and samples in which both types (21.9%) were represented. We also found a significant effect for the type of diagnostic interview, whereby only the CPTSDI (62.3%) yielded a significantly higher PTSD prevalence than the CAPS-CA (15.8%). Neither time since trauma exposure nor type of informant showed a significant moderating effect.
Outlier and bias assessment
In the DSM-IV data, no outliers were detected in a boxplot, nor on the basis of the z-scores of the effect sizes, which did not exceed −3.29 or +3.29. Reference Tabachnick and Fidell30 Egger’s regression test to account for effect size dependency was significant (b 0 = 0.64, s.e. = 0.15, t(92) = 4.29, 95% CI 0.34–0.94, P < 0.001), suggesting potential publication bias. However, when we ran adapted multilevel trim-and-fill analyses, Reference Fernandez-Castilla, Declercq, Jamshidi, Beretvas, Onghena and Van den Noortgate29 estimators yielded values below the threshold indicative of publication bias, Reference Fernandez-Castilla, Declercq, Jamshidi, Beretvas, Onghena and Van den Noortgate29,Reference Kromrey and Rendina-Gobioff31 with R 0 = 3 and L 0 = 0. Visual inspection of the funnel plot (Fig. 2) indicates symmetry. Our bias analyses thus provided conflicting evidence on the presence of publication bias.
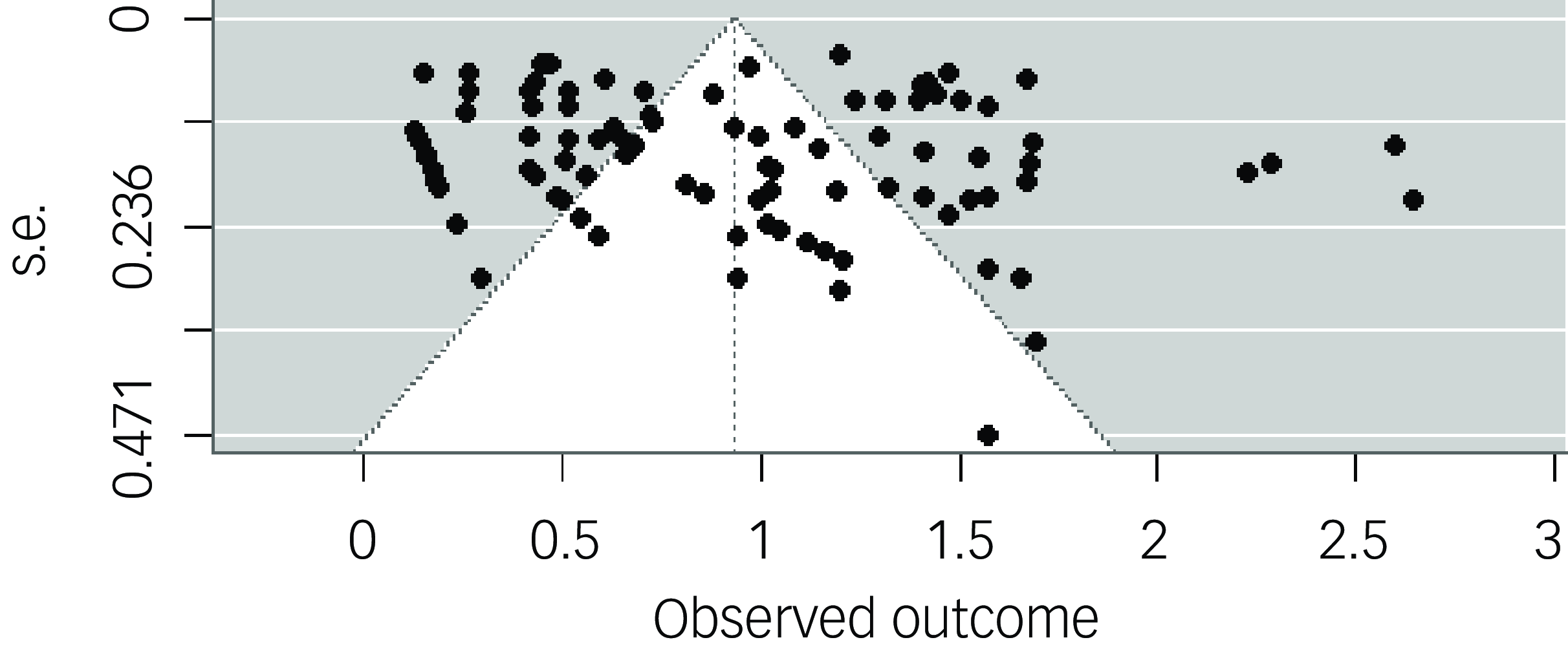
Fig. 2 Funnel plot for DSM-IV meta-analysis. Funnel plot displaying DSM-IV transformed prevalence rates plotted against their s.e., to assess publication bias.
In the DSM-5 data, one outlier was detected from examination of a boxplot. However, as none of the z-scores for the effect sizes exceeded the threshold values of −3.29 or +3.29, Reference Tabachnick and Fidell30 we retained the outlier in all our analyses and ran separate sensitivity analyses excluding the outlier (see sensitivity analyses and Supplementary Figs S3 and S4 in the Supplementary Material). No significant result was obtained in an adapted Egger’s test to account for effect size dependency (b 0 = 0.71, s.e. = 0.34, t(8) = 2.13, 95% CI −0.06–1.50, P = 0.066). Multilevel trim-and-fill analysis estimators were both below their respective threshold values, Reference Fernandez-Castilla, Declercq, Jamshidi, Beretvas, Onghena and Van den Noortgate29,Reference Kromrey and Rendina-Gobioff31 with R 0 = 0 and L 0 = 0. However, visual inspection of the funnel plot (Fig. 3) indicates no clear symmetry. Our bias analyses thus did not conclusively demonstrate the absence of publication bias.
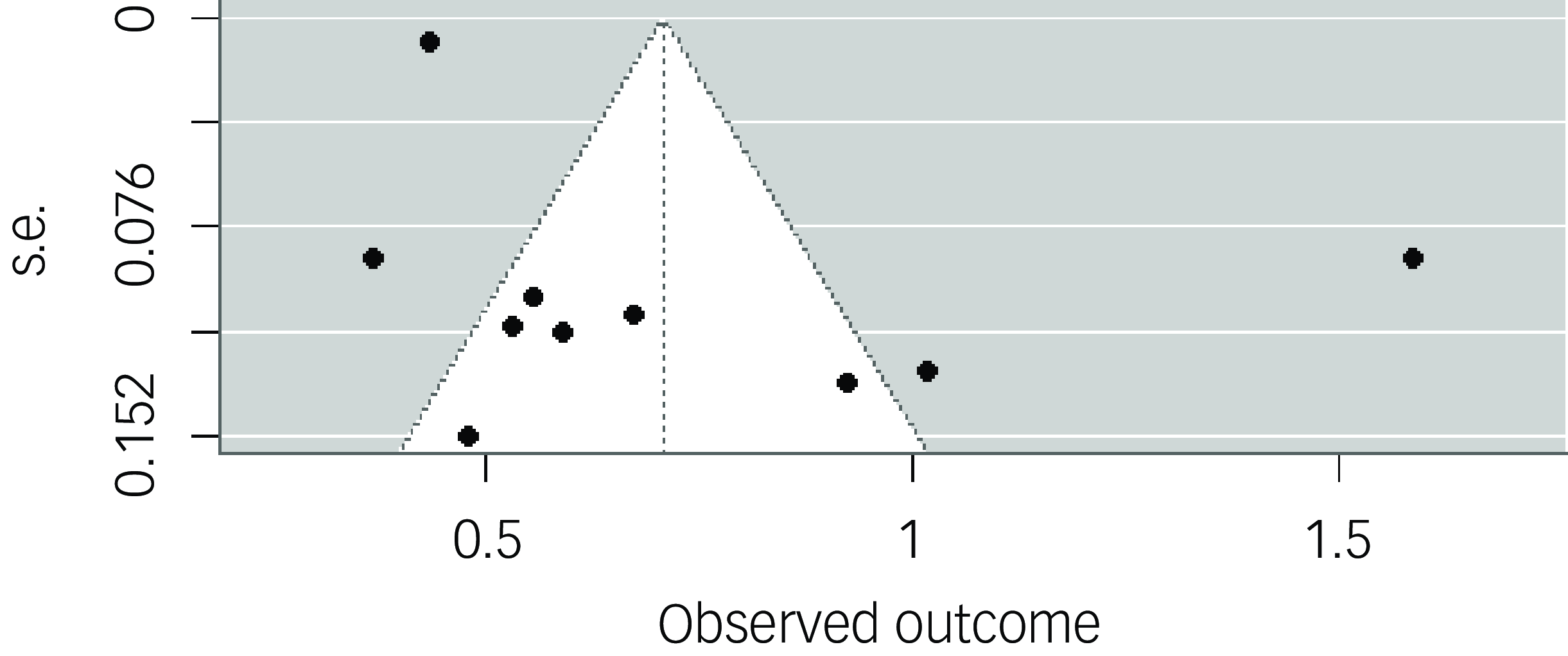
Fig. 3 Funnel plot for DSM-5 meta-analysis. Funnel plot displaying DSM-5 transformed prevalence rates plotted against their s.e., to assess publication bias.
Discussion
In the past decade, no meta-analytic estimates have been made, to our knowledge, of the prevalence of PTSD among children and adolescents, despite numerous new prevalence studies and the revised diagnostic criteria in the DSM-5. In the current study, we sought to update the most recent meta-analysis by Alisic and colleagues, Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 by incorporating new studies published since 2012. Using a total of 64 independent samples, from which we extracted 104 effect sizes, we meta-analytically estimated PTSD prevalence rates for trauma-exposed children and adolescents according to both DSM-IV and DSM-5 diagnostic criteria.
PTSD prevalence estimates
After analysis of all primary studies that applied DSM-IV diagnostic criteria, our estimation revealed a PTSD prevalence rate of about 20% (range 15–26%), indicating that approximately one in five trauma-exposed children and adolescents develop PTSD. This prevalence is slightly higher than the 16% (range 8–33%) rate found by Alisic et al, Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 but remains within a comparable range. This reaffirms that, although most children do not develop PTSD after experiencing potentially traumatic life events, a significant subgroup of young people remains that do face substantial burdens. These findings thus emphasise the importance of trauma-related screening and diagnostics after an event has been experienced, followed by watchful waiting and prevention of further events, as early identification of PTSD has been linked to improve treatment outcomes and long-term prognosis. Reference Burback, Brult-Phillips, Nijdam, McFarlane and Vermetten32
In studies using DSM-5 diagnostic criteria, our analysis determined an estimated PTSD prevalence rate of approximately 12% (range 3–24%). That rate was lower than our estimate for the DSM-IV criteria (20%, range 15–26%), although the ranges overlap. In literature on children and adolescents, it has been suggested that the new PTSD diagnostic criteria in DSM-5, with their improved developmental sensitivity, could actually generate higher prevalence findings for children. Reference De Young and Landolt11 Although it is true that a direct comparison between eight studies and 56 studies may not be entirely robust, the fact that the eight DSM-5 studies included 12 644 children, compared with the 6745 children in the 56 DSM-IV studies, should also be considered. It therefore seems reasonable to argue that prevalence rates obtained under DSM-5 criteria are most likely to be significantly lower than those under DSM-IV criteria.
Interestingly, reported PTSD prevalence estimates varied widely between studies, ranging from 0 to 89%. Such variations are likely attributable to several factors, including sample size and the type of traumatic events experienced. Notably, Ostrowski et al Reference Ostrowski, Ciesla, Lee, Irish, Christopher and Delahanty33 observed a prevalence of 0% in their study, with a modest sample size (N = 99) and a focus on relatively mild traumatic experiences limited to non-abusive events and emergency department stays not exceeding 8 h. In contrast, Wechsler-Zemring et al Reference Wechsler-Zimring and Kearney34 observed a prevalence of 89% in their study that was similarly constrained by sample size (N = 84), but focused on youth who experienced neglect as well as physical or sexual maltreatment.
Moderator effects
In the DSM-IV prevalence data, several sample characteristics were examined to determine whether the PTSD prevalence estimate would show any variability. First, we found that gender moderated the prevalence rate, with primary studies reporting lower PTSD prevalence rates as the percentage of boys in samples increased. This finding aligns with the previous meta-analysis by Alisic et al. Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 Biological, psychological and sociocultural factors may contribute to this difference. For instance, girls are generally found to have higher oestrogen levels and a more sensitised hypothalamus–pituitary–adrenal axis. Reference Garza and Jovanovic35,Reference Singh and Wendt36 Additionally, coping strategies differ by gender Reference Tamres, Janicki and Helgeson37 and these may affect PTSD risk. Reference Pineles, Hall and Rasmusson38 Furthermore, girls are more likely to be exposed to interpersonal trauma types that carry higher PTSD risks, such as sexual violence and domestic abuse. Reference Tolin and Foa39 At the same time, girls tend to have stronger social support networks, and these may, depending on the context, either alleviate or exacerbate PTSD symptoms. Reference Wang, Chung, Wang, Yu and Kenardy40 Given these varying interpretations, our findings primarily underline the need for better research into the causal mechanisms that produce gender-specific differences.
Second, we observed that the type of trauma experienced also moderated the overall prevalence rate of PTSD, with interpersonal trauma associated with a higher rate than non-interpersonal trauma, also in samples where both interpersonal and non-interpersonal trauma were represented. The findings support the notion that children and adolescents who have experienced violence, abuse or other significant boundary breaches within their relationships are at an increased risk of developing PTSD as compared with children who have experienced non-interpersonal trauma only. Associated factors such as shame, guilt and feelings of betrayal play a role in this increased risk. Reference DeCou, Lynch, Weber, Richner, Mozafari and Huggins41–Reference Kletter, Weems and Carrion43 Furthermore, existing research indicates that interpersonal trauma increases not only the risk of PTSD, but also the likelihood of other forms of psychopathology and physical health problems. Reference Fischer, Dölitzsch, Schmeck, Fegert and Schmid44,Reference Lopez-Martinez, Serrano-Ibanez, Ruiz-Parraga, Gomez-Perez, Ramirez-Maestre and Esteve45
Third, the type of diagnostic interview employed showed an ostensibly moderating effect on the PTSD prevalence rate, with the CPTSDI yielding a significantly higher rate than the CAPS-CA, which we used as a reference category. However, it seems unlikely that the observed difference can be attributed to the type of diagnostic interview. Notably, in four of the five studies in our analysis that utilised the CPTSDI, the sample consisted of individuals who had experienced interpersonal trauma. Consequently, the observed difference might sooner be ascribed to the limited number of included studies, combined with small sample sizes, and the target population in which the interviews were administered.
No moderating effect was found for the type of informant interviewed (that is, the child, parent or a combination), which is in line with the findings of Alisic et al. Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 Nor did a significant moderating effect emerge from the time elapsed since trauma exposure, categorised as less than or more than 3 months post-trauma. This contrasts with previous research on adults and on children, which suggested a decrease in prevalence after 3 months post-trauma. Reference Rezayat, Sahebdel, Jafari, Kabirian, Rahnejat and Farahani17,Reference Diamond, Airdrie, Hiller, Fraser, Hiscox and Hamilton-Giachritsis19 However, as previously noted by Alisic et al, Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 many included studies reported wide variability in the timing of PTSD assessment or provided no timing information, thus resulting in substantial missing data for our moderation analyses.
Strengths
We believe our study has several important strengths. To begin with, it offers a comprehensive overview of PTSD prevalence rates among trauma-exposed children and adolescents, assessed on the basis of both DSM-IV and DSM-5 diagnostic criteria. It does so by meta-analytically combining a wide array of studies published between 1994 and 2024. Second, the different studies included in our meta-analyses featured samples with varying types of trauma. That enabled us to base our estimations on a large group of children and adolescents who had experienced a wide range of potentially traumatic events – from single events to chronic situations, and from interpersonal to non-interpersonal events. In addition, by employing a multi-level approach in our meta-analyses, we were able to include as much data as possible from single studies, as we were not restricted to one effect size per study, because of potential effect size dependency.
Limitations
A number of limitations also need to be considered. First, we did not test for age differences in PTSD prevalence rates. Previous research suggests that age significantly affects PTSD prevalence rates, with varying rates observed across different age groups. Reference De Young and Landolt11,Reference Mikolajewski, Scheeringa and Weems12 That effect has not yet been examined meta-analytically. Many of our included studies used samples with broad age ranges, and that prevented us from differentiating PTSD prevalence rates for younger or older children or adolescents. Second, although recent evidence suggests an effect of trauma load on PTSD prevalence rates, Reference Knipschild, Hein, Pieters, Lindauer, Bicanic and Staal46 we were unable to examine this variable in our moderator analyses. This was primarily because of the absence of sufficient individual-level data on cumulative trauma, as many of the included studies did not report this level of granularity. Third, we applied similar inclusion and exclusion criteria to those used by Alisic and colleagues, Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad and Hassanpour8 to match their work as closely as possible. However, this approach does not eliminate the risk of bias and confounding in our estimated prevalence rates. As similarly noted by those authors, many children with higher vulnerability, such as those with cognitive limitations or current medication use, were not included in the studies we analysed. The absence of such children could result in underestimation of the true prevalence rates. Fourth, a lack of statistical power precluded the conduct of interaction moderation analyses for our discrete variables, thus restricting us in disentangling significant effects and yielding more nuanced insights.
Implications
The findings of our meta-analyses have several important implications for clinical practice and policy making. These show that the majority of children do not typically meet the criteria for PTSD in the aftermath of potentially traumatic events. Yet some 12% of children and adolescents do exhibit PTSD, with symptoms including traumatic re-experiencing, pervasive negative perceptions and heightened vigilance. Such symptoms can inflict profound distress and interfere with children’s developmental trajectories across various domains of life. Clinically, given the significant impact of post-traumatic stress symptoms, it is imperative to implement evidence-based screening and diagnostic measures, along with targeted trauma interventions for the individuals affected. Early identification is crucial, as untreated PTSD can evolve into more complex, comorbid mental health conditions. Reference Meiser-Stedman, Smith, Yule, Glucksman and Dalgleish6,Reference Norton, Barrera, Mathew, Chamberlain, Szafranski and Reddy7 From a policy perspective, our findings highlight the need for comprehensive trauma prevention and response programmes in educational and community settings. These would aim both to reduce the incidence of potentially traumatic events and to provide robust support systems for traumatised children. Preventive efforts should prioritise reducing exposure to traumatic events through initiatives targeting family violence, bullying and community safety – factors that are consistently associated with increased PTSD risk. Reference Dai, Liu, Kaminga, Deng, Lai and Wen14,Reference Fowler, Tompsett, Braciszewski, Jacques-Tiura and Baltes47,Reference Nielsen, Tangen, Idsoe, Matthiesen and Magerøy48 Evidence underscores that fostering safe and supportive environments can mitigate the psychological impact of trauma and bolster resilience. Reference McLaughlin and Lambert49 The differences in PTSD prevalence that we observed with respect to the DSM-IV and DSM-5 diagnostic criteria also indicate that future epidemiological studies should consistently apply updated diagnostic frameworks, to enhance comparability and accuracy. This is particularly pertinent, given the lower PTSD prevalence rate we identified when using the DSM-5 criteria. It may reflect more stringent diagnostic thresholds or improved developmental sensitivity in the DSM-5. As research on PTSD in children evolves, it will be critical to consider these factors so as to better understand the true prevalence of PTSD.
Supplementary material
The supplementary material is available online at https://doi.org/10.1192/bjp.2025.30
Data availability
Data availability is not applicable to this article as no new data were created or analysed in this study. The analytic code and research materials associated with the manuscript are available from the corresponding author, I.V., upon reasonable request.
Acknowledgements
The authors thank Michael Dallas, BA, of Amsterdam for providing language editorial support, which was funded by Amsterdam UMC.
Author contributions
I.V., M.v.d.M., R.K., I.H., W.S. and R.J.L.L. conceptualised and designed the study. J.S. performed the literature search, and I.V. and H.D. selected and coded the qualifying studies. I.V. conducted the analyses, and M.A. and N.v.D. supervised the analyses. I.V., M.v.d.M., R.K. and R.J.L.L. wrote the first draft of the manuscript. All authors contributed to the interpretation of the data, reviewed and revised the manuscript and approved the final manuscript as submitted.
Funding
This study was part of the DREAMS Trauma Research Project. DREAMS is funded by the Association of Netherlands Municipalities through structurally allocated government funding. The funder had no role in the design of the study, in the collection, analyses or interpretation of data; the writing of the manuscript or the decision to publish the results. All views expressed are those of the authors and not necessarily those of the funders.
Declaration of interest
None.







eLetters
No eLetters have been published for this article.