An estimated 4% of the world’s population experiences psychosis Reference Moreno-Küstner, Martín and Pastor1 – mental health symptoms characterised by loss of contact with reality that may manifest as delusions, hallucinations or disorganised thoughts or behaviours. 2 Psychotic disorders pose significant challenges to individuals, their families and society because they are associated with productivity losses, morbidity and mortality, including suicidality. Reference Starzer, Hansen, Hjorthøj, Speyer, Albert and Nordentoft3,Reference Bai, Liu, Jiang, Zhang, Rao and Cheung4 Effective treatment of psychosis necessitates engagement with the formal healthcare system for pharmacological and psychosocial interventions. However, patients experiencing psychosis are often deterred from seeking care due to stigma, religious/cultural beliefs or financial constraints. Reference James, Thomas, Seb-Akahomen, Igbinomwanhia, Inogbo and Thornicroft5 In Ghana, psychotic disorders are the mental disorders most diagnosed, probably due to the disruptive nature of severe psychotic symptoms, and account for most psychiatric in-patients. 6 These patients probably represent a small proportion of cases with the most severe symptoms, because many individuals experiencing psychosis in Ghana do not engage with the formal health system. 7 This situation is exacerbated by inadequate mental healthcare investment, a shortage of skilled professionals and the influence of religious and cultural beliefs that contribute to delays in seeking care. 7
Disengagement from care
The systemic issues not only hinder initial access to mental health services but also contribute to ongoing patient disengagement. Even after accessing mental health services, patients often disengage due to cost, lack of support, poor insight or stigma. Reference Hailemariam, Fekadu, Prince and Hanlon8 Disengagement from care worsens symptoms and disrupts the lives of patients and their families. Engaging patients in the early stages of psychosis is critical to minimising its impact and improving outcomes. Reference Correll, Galling, Pawar, Krivko, Bonetto and Ruggeri9
Impact of antipsychotics on cardiovascular outcomes
Individuals with psychosis have a reduced life expectancy of 10–15 years, Reference Hjorthøj, Stürup, McGrath and Nordentoft10 with cardiovascular disease being a major contributor to this excess mortality. Reference Correll, Solmi, Croatto, Schneider, Rohani-Montez and Fairley11 Metabolic syndrome, which is exacerbated by clinically significant weight gain (CSWG) (≥7% of baseline weight), Reference Dai, Li, Yang, Xu, Jia and Yang12,Reference Bares, Wu, Tassiopoulos, Lake, Koletar and Kalayjian13 increases the risk of cardiovascular disease and mortality. Reference Li, Zhai, Zhao, He, Li and Liu14 Unfortunately, antipsychotics, although necessary for treating psychosis, contribute to weight gain and metabolic issues through multiple mechanisms. Reference Cuerda, Velasco, Merchán-Naranjo, García-Peris and Arango15 This risk is highest in the early stages of treatment. Reference Dayabandara, Hanwella, Ratnatunga, Seneviratne, Suraweera and de Silva16 Recent systematic reviews and meta-analyses have shown that most antipsychotics cause weight gain; Reference Campforts, Drukker, Crins, van Amelsvoort and Bak17,Reference Wu, Siafis, Hamza, Schneider-Thoma, Davis and Salanti18 the difference, however, lies in the magnitude of the weight gain and the proportion of patients who experience this outcome. This suggests that there are really no ‘safe antipsychotics’ in regard to weight gain.
Special monitoring of cardiovascular disease risk factors is therefore vital for extending the lifespan of patients with psychosis. Guidelines from both Europe and the USA recommend frequent monitoring of fasting blood sugar and lipid profiles, especially during the initial months of antipsychotic treatment. Reference Azfr Ali, Jalal and Paudyal19 Given that the treatment options available may not significantly reverse antipsychotic-induced weight gain and metabolic abnormalities, Reference Speyer, Westergaard, Albert, Karlsen, Stürup and Nordentoft20 prevention through lifestyle modifications and early detection via regular testing are crucial. There are no equivalent protocols for cardiometabolic monitoring for people with psychosis in Ghana.
Current situation in Ghana and Sub-Sahara Africa
Accra Psychiatric Hospital is the oldest psychiatric hospital in Ghana and one of the oldest in West Africa, serving as the primary training centre for mental healthcare in that country. It is the main centre for training of psychiatrists under both the Ghana and West Africa Colleges of physicians in Ghana. In addition, many medical schools and allied health programmes in Ghana receive mental health training from the Accra Psychiatric Hospital. The hospital has a capacity of 300 beds, with acute and chronic wards and a residential drug rehabilitation centre. It also has a medical laboratory, clinical psychology, occupational therapy, social welfare and community psychiatry units. It attends to over 600 new cases of non-affective psychosis annually.
One study in Nigeria found that the mean body mass index (BMI, kg/m2) of patients prescribed second-generation antipsychotics increased from 23.7 at baseline to 31 after 3 months. Reference Chukwujekwu and Olose21 Luckhoff et al Reference Luckhoff, Phahladira, Scheffler, Asmal, du Plessis and Chiliza22 also found that BMI change scores inversely correlated with Positive and Negative Syndrome Scale scores in a South African population. However, these studies did not estimate the proportion of patients who became overweight or obese over time. There is a gap in the knowledge regarding the effects of antipsychotics on the weight and BMI of patients taking antipsychotics in Ghana. Additionally, there is little information regarding the characteristics of psychotic patients in Ghana that predispose them to antipsychotic-induced weight gain. The absence of both guidelines on the prescription of antipsychotics and monitoring for cardiovascular disease lead to delay in detecting patients that require treatment.
Current study
We aimed to address this gap in knowledge at Accra Psychiatric Hospital, by reviewing patients’ attendance patterns and cardiovascular risk (trends in weight and BMI) among patients newly diagnosed with psychosis for the first 6 months following initial engagement in care. We also examined some correlates of cardiovascular disease risk factors. Overall, we aim to evaluate disengagement in care and cardiovascular disease risk outcomes among newly diagnosed psychotic patients at Accra Psychiatric Hospital.
Method
Sample and setting
This is a retrospective cohort study conducted by reviewing the anonymised electronic medical records of patients at Accra Psychiatric Hospital in Ghana. The inclusion criteria were all patients newly diagnosed with non-affective psychotic disorder according to the ICD-10 23 criteria (F20–29) during the study period (1 June 2022 to 31 May 2023) and who had received antipsychotic medication. We included both voluntary and involuntary patients. Patients under the age of 18 years were excluded in the analysis of weight and BMI changes but were included in the analysis of disengagement and medication prescription patterns at first visit. All patients were followed for a maximum of 6 months, with assessments at baseline, 3 months and 6 months. The 6-month cut-off point was used because, beyond that time point, the disengagement rate was close to 100%. Ethical approval was obtained from Accra Psychiatric Hospital’s Research and Ethics Committee (no. APH-ERC 00012/23). Six research assistants performed data abstraction after receiving training on the protocol and data abstraction tool. The principal investigator audited the work to ensure compliance with the protocol.
Outcome measures
Outcome variables collected included medication choice, dropout status in the first 6 months, evidence of cardiovascular disease monitoring and weight changes. We also collected demographic information (age, sex, occupation) and anthropometric data (weight [kg] and BMI/ [weight/height]), 2 which were used as covariates in our analysis. The data were clustered at baseline, 3 ± 1 months and 6 ± 1 months. Where there were multiple visits, the last before the particular time point was used. All weights were recorded using the same weighing scale at the hospital outpatient department.
Statistical analysis
Statistical analysis was performed using R version 4. Descriptive statistics, including frequencies (percentages) and means (±s.d.) were used to analyse categorical and continuous baseline data, respectively. The prescription pattern and factors influencing the choice of medication were also analysed, using multinomial logistic regression. We further analysed the pattern and risk factors for weight change using a linear mixed-effects model. The fixed effects in this model were patients’ age, baseline weight, sex, time and medication. In comparing weight change based on medication choice, olanzapine was set as the reference medication because it was the medication prescribed most often. Medications with frequency below ten (chlorpromazine, clozapine, paliperidone and quetiapine) were excluded from the analysis. Results from the models include 95% CIs to provide estimates of precision. Missing data were omitted during the analysis.
Results
Baseline characteristics and prescribed medication
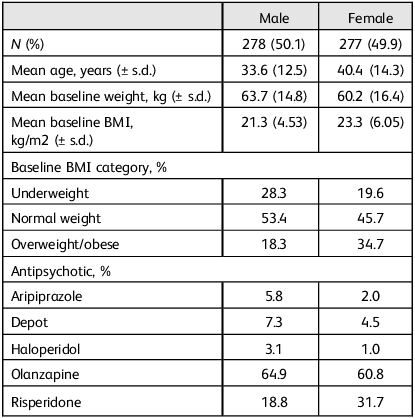
Table 1 shows the mean age, weight, BMI and prescribed antipsychotic of patients at their first visit to the study site.
Table 1 Baseline characteristics and prescribed medication

Hospital attendance
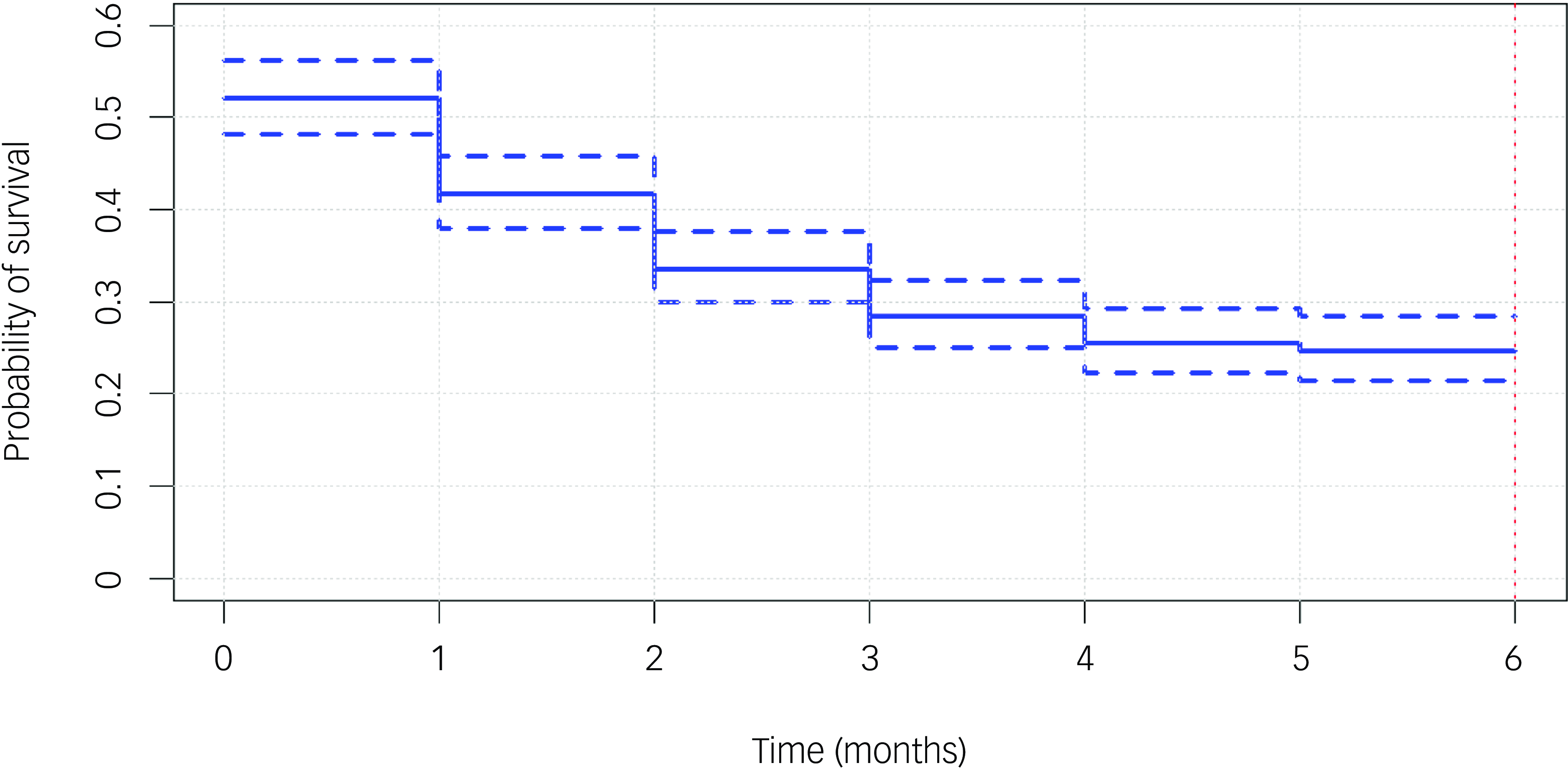
The majority of patients (75.5%) stopped attending reviews within the first 6 months. More than half (53.1%) of patients did not engage with the service for up to 1 month; they either never attended again after their first visit or were seen within 1 month of their first visit and then became lost to follow-up. Most patients (39%) did not return for review following their first visit, while only 24% and 14% attended a total of one and two additional reviews, respectively, after the first visit. Figure 1 shows the probability of disengagement at various time points within the first 6 months of care.

Fig. 1 Probability of disengagement within the first 6 months. Survival curve showing the probability of patients dropping out at various time points (months) within the first 6 months.
Cardiometabolic monitoring
From our analysis, olanzapine was the antipsychotic most prescribed (62.8%) and aripiprazole the least (3.6%). Despite the high rate of prescribing olanzapine, less than half of the patients at their first visit had their blood sugar (43%) or lipid profile (26%) requested/recorded before initiating antipsychotic treatment. This pattern did not improve over time, with under 5% having had their blood sugar or lipid profile tested at each subsequent visit. Furthermore, 13% of patients did not have records of their weight at first visit. A multinomial logistic regression using patients’ age, sex and baseline weight as predictors indicated that patients with higher baseline weight were more likely to receive aripiprazole (odds ratio 1.07, 95% CI 1.04, 1.10, P < 0.001), haloperidol (odds ratio 1.05, 95% CI 1.01, 1.09, P = 0.03) or risperidone (odds ratio 1.04, 95% CI 0.07, 1.05, P < 0.001) in comparison with olanzapine.
Weight change over time
At 3 months, 40% of patients experienced clinically significant weight gain (≥7% of baseline weight), and this increased to 58% at 6 months.
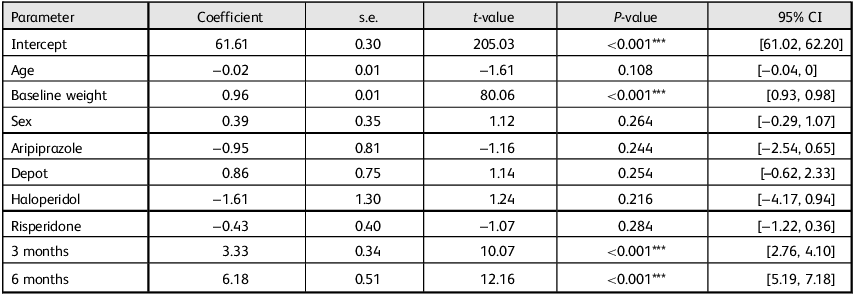
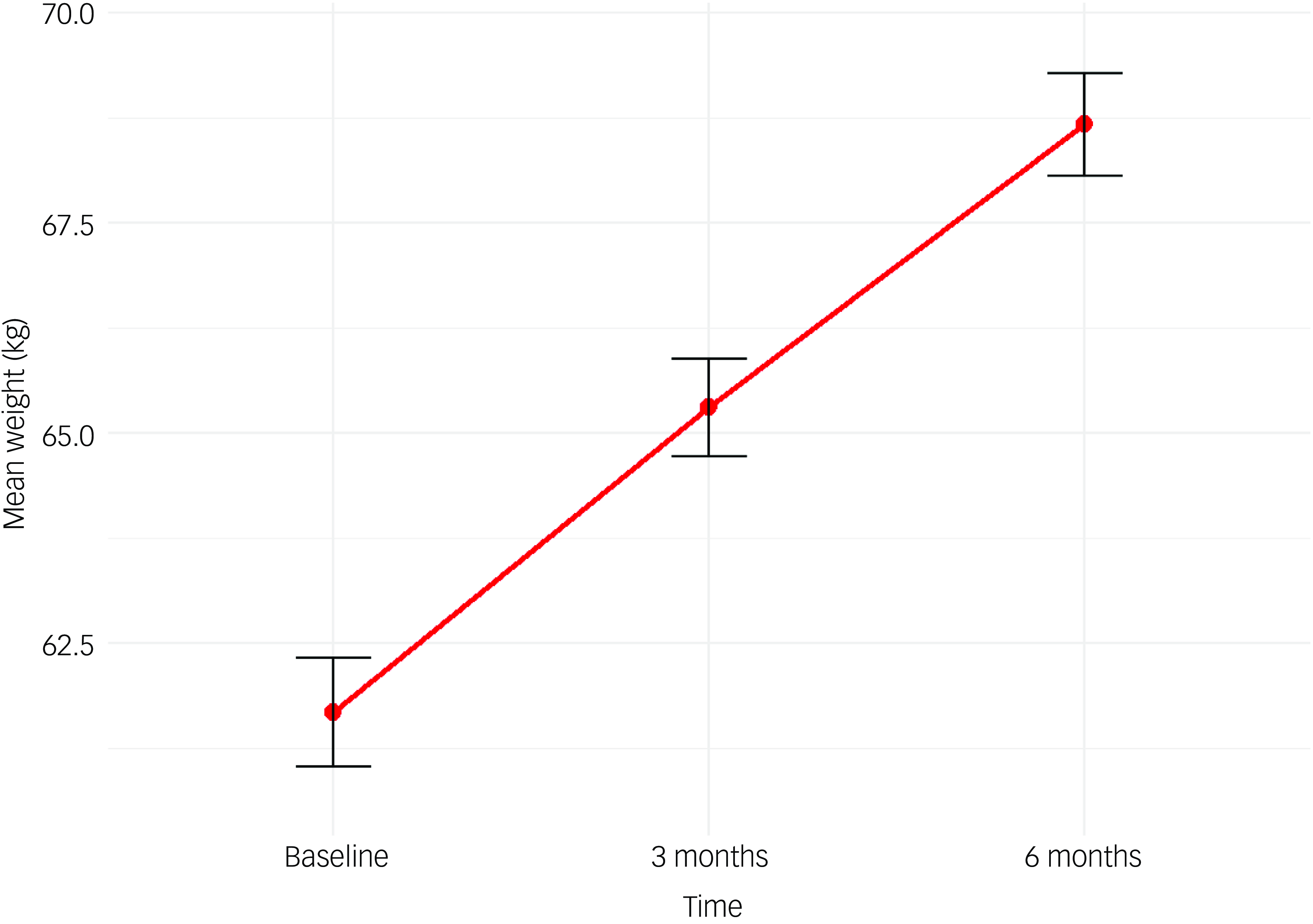
We fitted a linear mixed-effects model to examine the effects of selected covariates on weight change, incorporating age, sex, baseline weight, medication type and time, with a random effect for individual subjects. The results (Table 2) indicated that higher baseline weight was associated with significantly greater weight over time (β = 0.96, P < 0.001). Additionally, weight increased significantly over the 6-month follow-up period, with notable weight gains of 8.6% above baseline weight at 3 months (β = 3.33, P < 0.001) and increasing to 12.2% at 6 months (β = 6.16, P < 0.001), as illustrated in Fig. 2. None of the medication types, when compared with olanzapine, showed statistically significant different effects on weight change. Additionally, sex was not a significant predictor of weight change (β = 0.39, P = 0.264).
Table 2 Effects of various covariates on weight change

*** P < 0.01.

Fig. 2 Weight change in the first 6 months. Line chart showing the mean weight trajectory of patients in the first 6 months of starting antipsychotics.
Change in BMI
Patients’ BMI was dichotomised as either not overweight (BMI <25) or overweight (BMI ≥25) and was followed over time. BMI values generally increased over time in a way similar to weight. At baseline, about one quarter of patients (25.9%) had BMI ≥25 and, at 6 months, half of those with records available (52%) were overweight.
Discussion
This study used the medical records of patients at Accra Psychiatric Hospital in Ghana to analyse the pattern of attendance, antipsychotic prescription practices and weight and BMI changes over the first 6 months of treatment. Our results demonstrate a significant service disengagement rate, poor cardiometabolic risk monitoring and significant changes in weight and BMI over the first 6 months.
Baseline characteristics
The average age of our study population (37.4 years) is generally higher than findings from other countries in Africa and the UK. Reference Mishra, Patil, Sathe and Reshamvala24,Reference Gureje, Appiah-Poku, Bello, Kola, Araya and Chisholm25 This higher age of presentation probably reflects the prolonged duration of untreated psychosis in low- and middle-income countries, and the multiple pathways to care in Ghana. Reference Appiah-Poku, Laugharne, Mensah, Osei and Burns26 Additionally, because Accra Psychiatric Hospital is a referral centre, there may be delays between the onset of psychosis and hospital presentation.
The mean BMI of 22.2 kg/m2, with 25.9% of patients being either overweight or obese, is comparable to the general Ghanaian population mean BMI of 24.7 kg/m2. Reference Titi, Id, Morrison and Annan27
Disengagement from service
Psychotic disorders generally follow a chronic course, usually requiring prolonged treatment. It is recommended that a first-episode psychosis be treated until symptoms have been in remission for a minimum of 1 year, to prevent exacerbations. Reference Üçok28 Our finding that over half (53.1%) of patients with non-affective psychosis disengaged within 1 month, and 75.5% by 6 months, is alarming. This rate is significantly higher compared with other regions, Reference O’Brien, Fahmy and Singh29 highlighting a particular issue in Ghana.
Several factors may have contributed to this high disengagement rate. Patients may transfer to community mental health services due to proximity, although this is unlikely to account for most cases because standard practice requires that patients be clinically stable before transfer to community care. Another factor is resorting to religious and faith healers, especially prayer camps, which is common and widely practised in Ghana. Reference Gyimah, Ofori-Atta, Asafo and Curry30 During the period under this review, patients and their caregivers had to bear the cost of care for mental health services, and this is another possible explanation for the high rates of disengagement. Additionally, some patients may have achieved full recovery and returned to baseline functioning, reducing their perceived need to continue to engage with mental health services, with some evidence suggesting that patients with early psychosis show good treatment response. Reference Kang, Piao, Li, Kim, Kim and Lee31 Furthermore, our review included all patients diagnosed with a non-affective disorder, and this includes patients with acute and transient psychotic disorders. These disorders are known to resolve quickly, usually within 1 month, 2 and these patients are unlikely to feel the need to return for review, especially considering the stigma associated with a psychiatric diagnosis. It is now a priority to understand the reasons for patient disengagement, to help to develop strategies aimed at improving retention and treatment outcomes.
Cardiometabolic considerations
Despite growing evidence concerning the metabolic consequences of olanzapine, Reference Pillinger, McCutcheon, Vano, Mizuno, Arumuham and Hindley32 63% of patients in our review received this medicatiion during their first visit. Clinicians probably prefer olanzapine due to its perceived superior efficacy in resolving psychotic symptoms, Reference Davis and Chen33 prioritising immediate clinical response over the risk of long-term metabolic dysregulation. Other countries recommend that olanzapine not be used as a first-line treatment for psychosis because of its metabolic profile. Reference Crlenjak, Curtis, Fraser, Fraser, Hughes and Mcgorry34 The low levels of use of long-acting injectable (LAI) antipsychotics (depot) in our study population could represent a cost issue. While second-generation antipsychotics are the preferred first-line treatment, LAIs are expensive and many patients cannot afford them. Clinicians might opt against first-generation LAIs due to their extrapyramidal side-effects.
Proactive prevention of cardiovascular-related mortality requires regular monitoring of cardiometabolic risk factors. The Royal College of Psychiatrists recommends cardiometabolic tests to monitor physical health in the early stages of antipsychotic treatment, including weight, BMI, blood pressure, plasma glucose and lipid profiles. Reference Perry, Holt, Chew-Graham, Tiffin, French and Pratt35 Our study’s finding of low levels of cardiometabolic monitoring, even among those receiving olanzapine, means that these standards are not being met, exposing patients to risk. Under half of patients had their blood sugar levels recorded before initiating antipsychotics, and this proportion did not improve significantly over time. Similarly, lipid profile monitoring was insufficient. The absence of established local protocols for cardiometabolic monitoring probably contributes to this issue, as well as the cost of laboratory investigations, which are borne by the patient or their caregiver. However, this cannot explain the failure to record patients’ weight during initial consultation.
Weight and BMI changes over time
Patients demonstrated progressive weight and BMI increases over the course of this review, consistent with findings from other studies in patients with first-episode psychosis. Reference Tek, Kucukgoncu, Guloksuz, Woods, Srihari and Annamalai36 People with higher baseline weight continued to record further increases.
Our analysis revealed that weight change associated with the other medications was not different from that of olanzapine. This finding of insignificant difference in the contribution of medication type to weight changes conflicts with the existing literature, which typically shows olanzapine to be associated with the greatest weight gain. Reference Tek, Kucukgoncu, Guloksuz, Woods, Srihari and Annamalai36,Reference Bernardo, Rico-Villademoros, García-Rizo, Rojo and Gómez-Huelgas37 The lack of randomisation in our study may have introduced selection bias based on clinician preferences, influencing the observed effects on weight changes. Olanzapine was preferentially prescribed for patients with lower baseline weight and, because lower baseline weight is associated with less weight gain in our population, people on other medications are likely to have differentially gained more weight, potentially masking the effects of olanzapine on weight. This would be plausible given that almost all antipsychotics are known to cause weight gain. Reference Campforts, Drukker, Crins, van Amelsvoort and Bak17,Reference Wu, Siafis, Hamza, Schneider-Thoma, Davis and Salanti18,Reference Bak, Fransen, Janssen, van Os and Drukker38 However, this could also be a type II error, with a lack of power to detect differences between medications. Our finding that 40% of patients experienced CSWG at 3 months and 58% at 6 months is higher than those of a recent meta-analysis on the association between antipsychotics and CSWG. Reference Campforts, Drukker, Crins, van Amelsvoort and Bak17 At baseline, one in four patients was either overweight or obese and, by 6 months, this proportion had increased to one in two. Research has pointed to racial differences in the experience of antipsychotic-induced weight gain with people of black ancestry recording higher weight gains than their caucasian counterparts. Reference Jerome, Pulley, Sathe, Krishnaswami, Dickerson and Worley39 Genetic variability in the expression of antipsychotic target genes and antipsychotic metabolism has been proposed as a reason for these observed racial disparities, Reference Zhang, Lencz, Zhang, Nitta, Maayan and John40,Reference Pardiñas, Kappel, Roberts, Tipple, Shitomi-Jones and King41 and this could be the reason why our study population, which is entirely African, recorded higher rates of weight increase. This calls for early, proactive efforts when initiating antipsychotics to prevent weight gain, identify those gaining weight and initiate measures to mitigate the impact on their physical health. Because there are no established guidelines for dealing with antipsychotic-induced weight gain, implementation of mitigation measures is at the discretion of the clinician. Having guidelines allows the hospital to plan and make resources for lifestyle or pharmacological interventions available for all patients.
Future research directions
This study highlights significant patient disengagement and lapses in both cardiometabolic risk monitoring and weight management in patients with psychosis at Accra Psychiatric Hospital. Even though feedback has been provided to the hospital, addressing these challenges requires robust monitoring protocols to ensure that patients’ cardiovascular risks are routinely evaluated, especially in the first few months of initiating antipsychotic treatment. Evidence-based interventions should be recommended to mitigate the cardiovascular risks associated with exposure to antipsychotics, and these should be timely, adopting both preventive and therapeutic approaches. There is also a need for ongoing research to understand the factors contributing to the high disengagement rate, and to develop interventions to address this problem. While these findings are restricted to the study site, the contributory factors are common to most low- and middle-income countries and these findings are likely to be replicated in similar settings.
Study limitations
This study utilised real-world clinical data, with significant missing data, which is a limitation to its interpretation. Additionally, the absence of randomisation potentially introduces bias in the allocation of medications, thus affecting the interpretation of the relationship between antipsychotic type and weight/BMI changes. Furthermore, there are probably unmeasured confounding variables such as genetic, lifestyle and dietary factors that could potentially account for a significant proportion of the variation noted in weight and BMI. Finally, because our study was a retrospective review, we were unable to obtain comprehensive follow-up data to ascertain the cause of some findings, such as the high disengagement rate.
Data availability
The data that support the findings of this study are available from the corresponding author, J.A., upon reasonable request.
Acknowledgements
We are grateful to Africa Oxford Initiative (AfOx) for supporting this project, and to the management of Accra Psychiatric Hospital for facilitating the necessary processes to enhance our work.
Author contribution
J.A. and B.L. conceptualised the research, developed the research questions and designed the study. All authors participated in the implementation of the programme and contributed to writing the manuscript. J.A. analysed the data. B.L. supervised the work.
Funding
This work was supported by an AfOx catalyst grant (no. AfOx-238). The funders had no role in the design and implementation of the study.
Declaration of interest
None.
Ethics statement
This work was approved by the Research and Ethics Committee of Accra Psychiatric Hospital.



eLetters
No eLetters have been published for this article.