Introduction
Carcinoma of the oesophagus poses a considerable global health challenge, being the 11th most prevalent cancer globally with 511,054 new diagnoses cases in 2022. This type of cancer was responsible for 445,129 fatalities, representing 4.6% of all cancer-related deaths. In India, it holds the second position in terms of incidence, with 70,637 cases and 66,410 deaths documented in 2022. Reference Bray, Laversanne, Sung, Ferlay, Siegel and Soerjomataram1 The treatment of locally advanced oesophageal cancer generally requires a multimodal strategy, which may include radical concurrent chemoradiotherapy (CRT) for cases deemed unresectable, as well as neoadjuvant CRT followed by surgical resection for those that are resectable. The tendency of oesophageal cancer to disseminate submucosally over extensive areas often necessitates the use of large radiation treatment volumes. Reference Miller2
Radiotherapy is essential in the management of oesophageal cancer, especially since over 60% of patients are diagnosed at advanced stages, making surgical intervention impractical. The intricate anatomy of the oesophagus, which is close to vital structures like the heart, lungs and spinal cord, poses considerable difficulties in formulating radiotherapy plans that deliver uniform doses to the target while adhering to the dose limitations for surrounding organs at risk (OARs).
In recent years, there have been notable improvements in the methodologies for treatment planning and delivery concerning oesophageal cancer. Although 3-dimensional conformal radiation therapy (3DCRT) has long been the standard approach, research has indicated that intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) may offer distinct benefits in specific clinical situations. Reference Deng, Wang, Shi, Jiang, Wang and Liu3–Reference Taher, Elawady and Amin7 Wu et al Reference Wu, Xie, Hu, Han, Yi and Zhou5 propose that 3D-CRT presents a more economical choice for the radiotherapy of middle thoracic oesophageal cancer when compared to VMAT and IMRT. Nevertheless, both VMAT and IMRT have demonstrated their efficacy in reducing high-dose radiation exposure to the lungs and heart, although this comes at the cost of administering lower doses to larger areas of these organs.
Comparative studies have produced varied outcomes. Dora et al. Reference Dora, Deshmukh, Chatterjee, Goel, Bose and Singh8 found that VMAT resulted in reduced heart exposure compared to 3DCRT in cases of locally advanced oesophageal cancer; however, this advantage did not lead to notable differences in survival rates when patients received high doses of chemotherapy and radiation. Ghosh et al. Reference Ghosh, Kapoor, Gupta, Khosla, Kochhar and Oinam9 showed that 3DCRT resulted in lower lung volumes exposed to 30Gy, 10Gy, and 5 Gy when compared to IMRT, although it was associated with increased average doses to the heart. In this study, Kataria et al. Reference Kataria, Govardhan, Gupta, Mohanraj, Bisht and Sambasivaselli10 demonstrated that VMAT provided a dose distribution that was either comparable to or superior to that of IMRT, leading to a significant decrease in lung doses, while the reductions in heart doses were minor and not statistically significant. This finding is further corroborated by Yin et al. Reference Yin, Chen, Xing, Dong, Liu and Lu11 in the context of cervical oesophageal tumours.
The most effective radiotherapy approach for oesophageal cancer continues to be a topic of discussion. To be considered effective, a radiotherapy technique should not only provide optimal target coverage but also minimise toxicity to surrounding tissues, allow for straightforward patient setup and potentially translate to improved clinical outcomes including survival benefits and quality of life. Hybrid methodologies that integrate 3DCRT with IMRT or VMAT have demonstrated potential across multiple cancer types, such as breast, oesophageal and lung cancers. Reference Mayo, Urie, Fitzgerald, Ding, Lo and Bogdanov12,Reference Takakusagi, Kusunoki, Kano, Anno and Tsuchida13
However, the optimal ratio of 3DCRT and VMAT for hybrid VMAT plans in oesophageal cancer remains unknown. In this dosimetric evaluation, we aim to determine the best hybrid treatment plan by comparing two different beam dose weightings, 33% and 67%, for 3D-CRT beams and 67% and 33% for VMAT plans, while minimising lung and heart doses in oesophageal cancer.
Methods and Materials
Patients and simulation
This study was conducted in the Department of Radiation Oncology, State Cancer Institute, IGIMS, Patna, Bihar. Retrospectively, 14 patients with carcinoma of the oesophagus were included between September 2021 and October 2023. This represents an initial study with a limited sample size; nonetheless, the findings provide important insights for improving treatment planning. Previously, all patients received radical treatment using coplanar VMAT (Volumetric Modulated Arc Therapy) with Rapid Arc Techniques on a True Beam SVC Linear Accelerator (Varian Medical Systems, Palo Alto, California, USA) using 6MV photon beam. Patients were positioned supine with arms raised overhead during CT simulation using the Revolution EVO model manufactured by GE Healthcare. CT images were obtained at 2.5mm slice spacing from vertebrae C2 to L4. The acquired Digital Imaging and Communications in Medicine (DICOM) images were transferred to Varian Soma Vision software (Version 16.0.14) for contouring purposes. Approval for the study was obtained from the hospital ethics committee.
Contouring of target volumes and organs at risk (OARs)
PET-CT simulation was utilised to exclude distant metastases. The gross tumour volume (GTV), clinical target volume (CTV), planning target volume (PTV), lymph nodes and OARs, including the lungs, heart and spinal cord, were delineated on the Eclipse Somavision Contouring Workstation version 16.0.14, according to Radiation Therapy Oncology Group protocol 0436. Reference Miyazaki, Ohira, Ueda, Isono, Fujiwara and Tanooka14 The GTV was identified by visible tumours or lymph nodes on CT scans, supported by fusion with PET-CT simulation images, and confirmed by a radiologist. Additional superior and inferior margins of 3–4.5 cm, along with a 1.5 cm radial margin, were added to the GTV to define the CTV. Lymph nodes were contoured with a 1 cm margin in all directions. The PTV was defined with an additional 0.5 cm margin around the CTV, considering GTV delineation.
Treatment planning
This study included four different hVMAT plans that combine 3DCRT with VMAT techniques. The configurations are: hVMAT-1, (33% (2-field) 3DCRT with 67% Arc); hVMAT-2, (33% (3-field) 3DCRT with 67% Arc); hVMAT-3, (67% (2-field) 3DCRT and 33% Arc) and hVMAT-4 (67% (3-field) 3DCRT with33% Arc).
These four treatment plans were generated for each patient using the Eclipse treatment planning system version 16.0.14, which is equipped with the Millennium 120 multi-leaf collimator (MLC). This collimator consists of 60 pairs of leaves, including 40 pairs that are 5 mm wide in the central region and 20 pairs that are 10 mm wide in the outer region, all utilised on a TrueBeam SVC linear accelerator (Varian Medical Systems, Palo Alto, CA, USA). In order to minimise the treatment delivery duration, a maximum dose rate of 600 MU/min was used, delivering a prescribed dose of 50.4 Gy in 28 fractions. The final dose calculation utilised the Analytical Anisotropic Algorithm. The primary aim in planning each hVMAT technique was to ensure uniform coverage of the Planning Target Volume (PTV), with a target of achieving a V95% of no less than 95%. Furthermore, the maximum point dose within the PTV should not exceed 107% of the prescribed dose. A secondary focus was to minimise the radiation doses to OARs for each individual patient. The dose constraints for the OARs utilised in the optimisation are presented in Table 1.
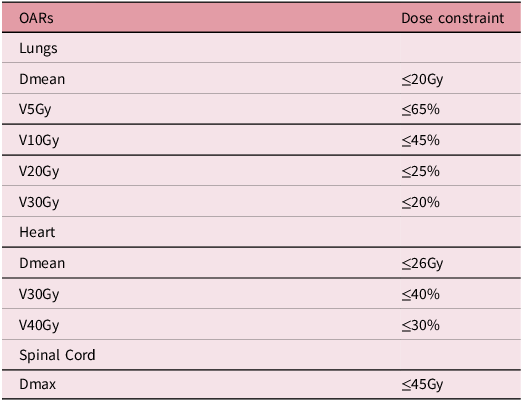
Table 1. Dose constraints for organs at risk (OARs)
Final hVMAT plan creation involves two steps.
Table 2. Planning target volume (PTV) analysis derived from dose-volume histogram (DVH) for all hybrid volumetric-modulated arc therapy (VMAT) plan
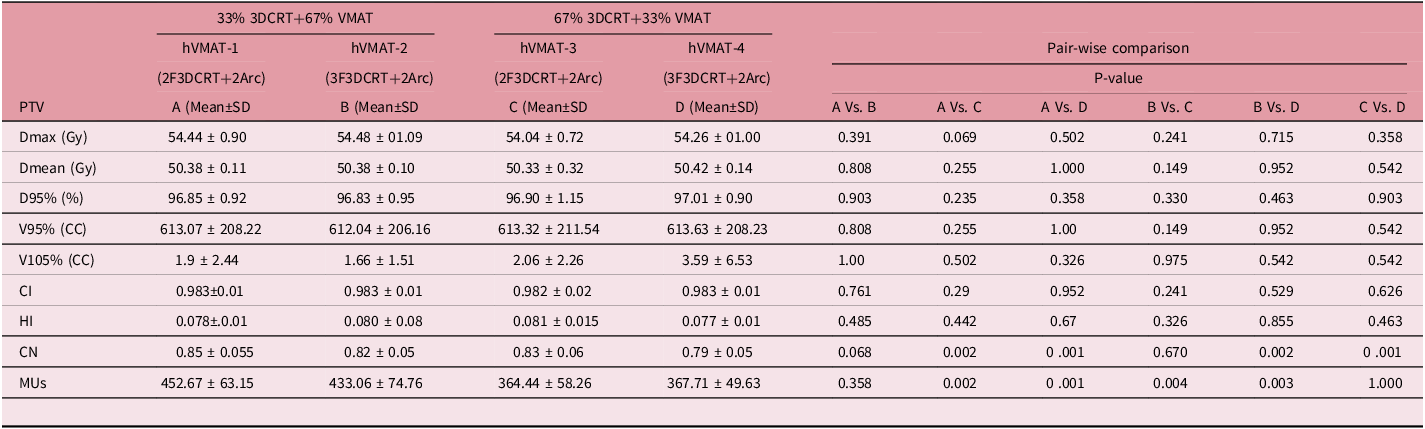
HVMAT (conformal+Arc), Dmax: Maximum Dose, Dmean: Mean Dose, D95%: Dose received by 95%, V95%: 95% dose received by volume (cc), SD: Standard Deviation, CI: Conformity Index, HI: Homogeneity Index, CN: Conformation number, Wilcoxon Signed-Rank Test for analyzing parameters. XX % dose received by % of the volume, MUs: Monitor Units.
Step 1: Creation of Hyb_3DCRT plans:
A standard beam configuration for the 3DCRT-1: 2F plan comprises an anterior beam positioned at 0° and a posterior beam at 180°. In contrast, the 3DCRT-1: 3F plan features an anterior-posterior (AP) field along with two posterior oblique fields, with gantry angles ranging from 100° to 120° and 240° to 260°, specifically chosen to protect the spinal cord. The photon beam energies utilised are 10 MV and 15 MV, with the selection of energy dependent on the thickness of the patient and the coverage of the planning target volume (PTV). MLCs are utilised, tailored to the PTV with a margin of 0.5 cm, and the collimator angle is adjusted to ensure optimal fitting of the MLCs. Each beam arrangement is designed with two different dose weightings, including 33% and 67% of the prescribed dose, leading to the creation of four different 3DCRT plans: 3DCRT-1: 2F at 33% Prescription dose (PD), 3DCRT-2: 3F at 33% PD, 3DCRT-3: 2F at 67% PD and 3DCRT-4: 3F at 67% PD.
Step 2 Hyb_arc plan:
In this study, a hybrid VMAT (hVMAT) plan was developed, featuring two complete arcs that included clockwise (from 181.0° to 179.0°) and counter-clockwise (from 179.0° to 181.0°) gantry rotations. A collimator rotation ranging from 30° to 330° was implemented to ensure comprehensive tumour coverage while minimising the tongue-and-groove effect associated with MLCs. The prescription was established based on the full planning dose. For the hVMAT plans, optimisation was conducted utilising the Photon Optimiser version 16.1, incorporating 3D conformal radiotherapy (3DCRT) base dose plans including 3DCRT-1 for hVMAT-1, 3DCRT-2 for hVMAT-2 and similarly for hVMAT-3 and hVMAT-4. In the development of the final hVMAT plan, each beam from the conformal Hyb_3DCRT plan was transferred into the hVMAT plan, initially setting the normalisation to ‘No Plan Normalization’ before recalculating the plan. The beam weightings of the conformal fields were modified to align with the monitor units (MU) from the original plan (Hyb_CRT), ensuring uniformity for subsequent optimisations. This process was facilitated by directly copying the beam weighting from the hVMAT plan to the Hyb_CRT plan. Ultimately, the normalisation was revised to 100.00% covering 50.00% of target volume.
Plan evaluation
The dose received by the target volume, as well as dosimetric parameters such as conformity index (CI), homogeneity index (HI), conformation number (CN) Reference Abotaleb, Attalah, El-Hossary and Ismaiel15 and integral dose (ID), Reference Chan, Lee, Hung, Chang, Yeung and Lee16 was assessed through the analysis of cumulative dose-volume histograms (cDVHs) for both the target volume and OARs.
Conformity index (CI) is defined as:
CI = Volume of reference isodose/ Volume of planning target volume---- (1).
Homogeneity index (HI) is defined as:
HI= (D2%–D98%)/D50%------ (2)
Where D2%, D98% and D50% are the dose received by 2%, 98% and 50% of the volume.
Conformation number (CN) is defined as:
CN= (TVRI/TV) x (TVRI/VRI) ------ (3)
Where TV, TVRI and VRI represent the treatment volume, the treatment volume at reference isodose (RI) of the prescribed dose and the total volume at RI of the prescribed dose, respectively. The RI was defined as 95% of the PTV prescribed dose.
Integral dose (ID):
ID = Dmean × Vmean × ρmean (Gy-L) ---- (4)
Where Dmean: mean organ dose, Vmean: mean organ volume, ρmean: mean organ density
For ρ = 1:
ID = Dmean × Vmean (Gy-L) ---- (5)
In addition, the MUs associated with each treatment plan were recorded for comparative analysis. The study analysed the mean doses received by the lungs and heart, as well as the maximum dose to the spinal cord. Volume-specific metrics, including V5Gy, V10Gy, V20Gy, V30Gy and V40Gy, were also documented for both the lungs and heart.
Gamma analysis
This study analysed the influence of hybrid treatment strategies on the precision of radiation therapy delivery, emphasising gamma passing rates. Dosimetric verification utilised the ArcCHECK (Sun Nuclear Corporation, Melbourne, Florida, USA), cylindrical diode array to compare the measured and calculated dose distributions. The main analysis criterion was set at 2%/2mm (2% dose difference, 2mm distance to agreement), with supplementary evaluations conducted at 3%/2mm and 3%/3mm. All analyses adhered to a 10% low-dose threshold. Treatment plans to achieve a gamma passing rate of ≥95% were considered of good quality for ensuring accurate and high-quality treatment for patients.
Statistical analysis
To analyse the dose-volume data of hybrid plans, a one-way Analysis of Variance (ANOVA) test was used to evaluate variance. Mean and standard deviation values were presented. SPSS software (version 26) was used to compare the four hybrid plans using a two-sided Wilcoxon rank-sum test for paired samples. A p-value <0.05 was considered significant.
Results
This study included 14 patients with carcinoma of the oesophagus in our department. Patients ranged in age from 41 to 83 years, with a median age of 65 years and a mean age of 63 years. Oesophageal carcinoma (EC) involved in this study included the upper-middle third and middle-lower third, middle and lower oesophagus. The long axis of the PTV varied from 14.3 cm to 25.61 cm, with an average of 19.99 cm. The average PTV volume was 613.28 cc, with a median of 615.85 cc (range 260.2 to 898.1 cc).
The dose distributions and cumulative dose volume histogram for four hybrid VMAT plans were presented for one patient in Figure 1. Table 2 demonstrates that the hVMAT plans do not exhibit significant variations in maximum dose (Dmax), mean dose (Dmean) and the dose delivered to 95% of the planning target volume (PTV) (D95%), CI and HI when comparing different combinations of 3DCRT with VMAT. However, a significant difference was observed in the conformation number (CN), where hVMAT-1(0.85 ± 0.055) displayed markedly superior conformity in comparison to hVMAT-3 (0.83 ± 0.068, p = 0.002) and hVMAT-4 (0.79±0.059, p = 0.001). Additionally, the assessment of MUs indicated significant disparities, with hVMAT-1 (452.67 ± 63.15) and hVMAT-2 (433.06 ± 74.76) necessitating a greater number of MUs than hVMAT-3 (364.44 ± 58.26, p = 0.002) and hVMAT-4 (367.71 ± 49.63, p = 0.001).
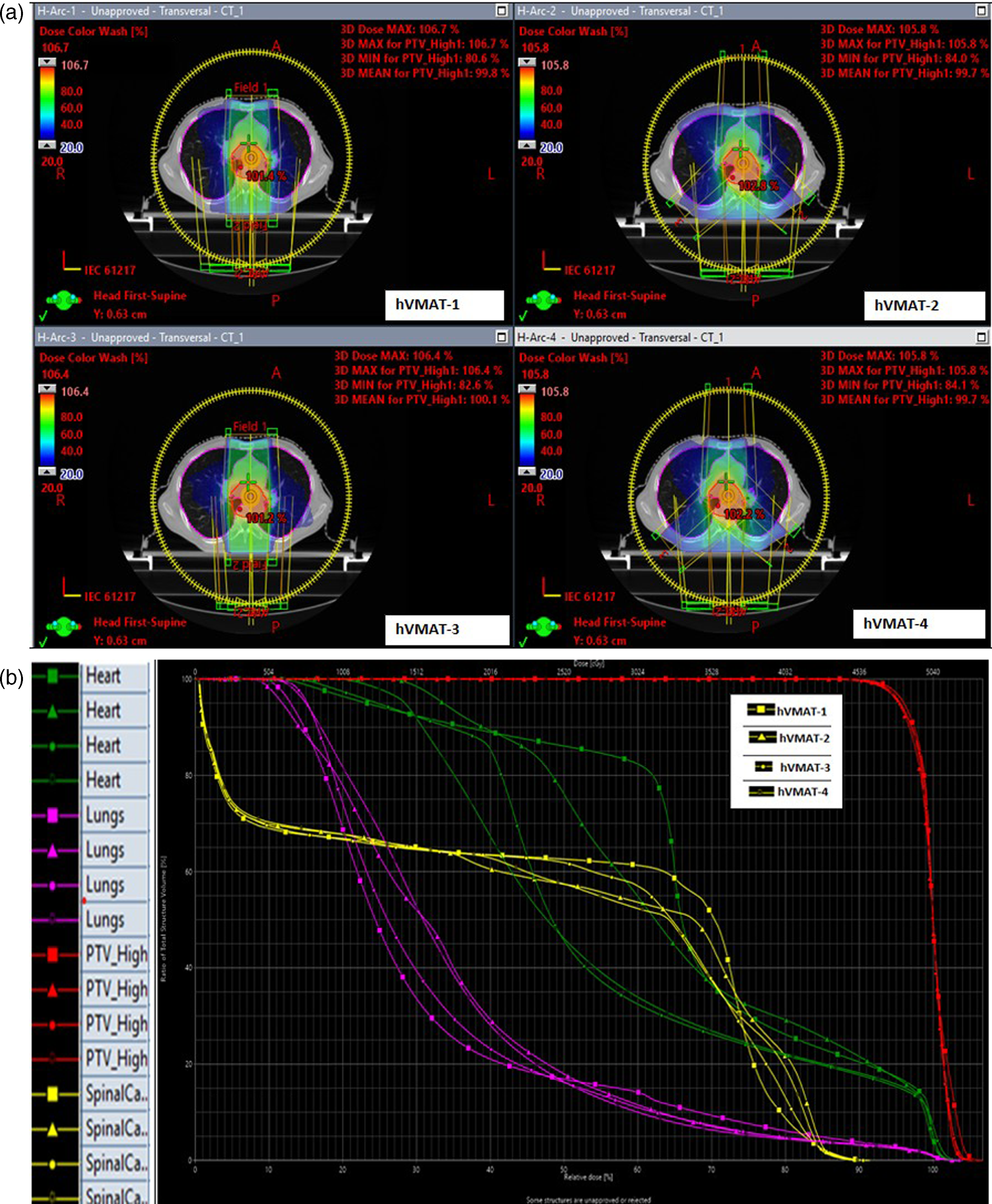
Figure 1. Dose distributions (a) and cumulative dose volume histogram (b) for a representative patient treated with four hybrid volumetric modulated arc therapy plans.
Table 3. Organ at risk values obtained from the cumulative dose-volume histograms (cDVHs) for all hybrid volumetric-modulated arc therapy (VMAT) plan
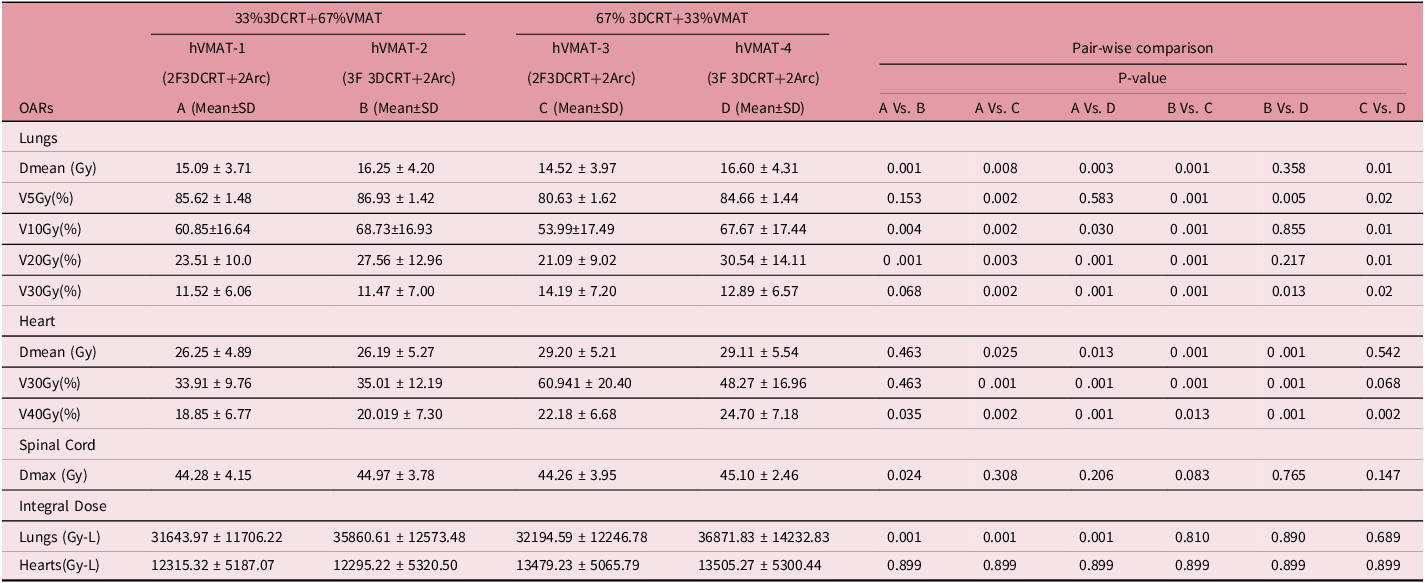
HVMAT (3DCRT +VMAT, Dmean: Mean Dose, SD: Standard Deviation, Vxx: XX % dose received by % of the volume, Wilcoxon Signed-Rank Test for analyzing parameters.
Organ at Risks Analysis
Table 3 shows the analysis of OAR values obtained from the cDVHs indicated notable discrepancies among the hybrid VMAT (hVMAT) plans.
Lung Dose Metrics: The mean dose delivered to the lungs (Dmean) exhibited considerable variation among the four hybrid VMAT configurations. hVMAT-1 provided a mean dose of 15.09 ± 3.71 Gy, which was significantly lower than that of hVMAT-2 (16.25 ± 4.20 Gy, p = 0.001) and hVMAT-4 (16.60 ± 4.31 Gy, p = 0.003). hVMAT-3 (14.52 ± 3.97 Gy) demonstrated a lower dose in comparison to hVMAT-2 and hVMAT-4; however, no significant differences were noted when compared to hVMAT-1 (p = 0.358). In the context of lung volume receiving 5Gy (V5Gy), HVMAT-1 achieved a delivery of 85.62 ± 1.48%, while hVMAT-2 reached 86.93 ± 1.42%. In contrast, hVMAT-3 demonstrated a notable decrease, delivering 80.63 ± 1.62% (p < 0.001) when compared to both hVMAT-1 and hVMAT-2. hVMAT-4 provided a delivery of 84.66 ± 1.44%, showing no significant difference when compared to the other configurations (p = 0.583 for hVMAT-1, p = 0.583 for hVMAT-2 and p = 0.02 for hVMAT-3). Significant differences were noted between hVMAT-2 and hVMAT-3 (p = 0.002), as well as between hVMAT-3 and hVMAT-4 (p = 0.005). However, no significant differences were observed between hVMAT-1 and hVMAT-3 (p = 0.153) or between hVMAT-1 and hVMAT-4 (p = 0.217). The V10Gy (%) values among the four hybrid VMAT configurations exhibited notable variations. The hVMAT-1 configuration yielded a V10Gy of 60.85 ± 16.64%, whereas hVMAT-2 recorded a higher value of 68.73 ± 16.93%. The disparity between hVMAT-1 and hVMAT-2 was statistically significant (p = 0.004). In contrast, hVMAT-3 produced a significantly lower V10Gy of 53.99 ± 17.49% when compared to hVMAT-1 (p = 0.002), while hVMAT-4 achieved a V10Gy of 67.67 ± 17.44%, which was also significantly different from hVMAT-1 (p = 0.030). However, no significant differences were found between hVMAT-2 and hVMAT-4 (p = 0.855) or between hVMAT-3 and hVMAT-4 (p = 0.01). Concerning the lung volume receiving 20Gy, the results were as follows: hVMAT-1 delivered 23.51 ± 10.0%, hVMAT-2 delivered 27.56 ± 12.96%, HVMAT-3 delivered 21.09 ± 9.02% and hVMAT-4 delivered 30.54 ± 14.11%. Notable differences were identified between hVMAT-1 and hVMAT-2 (p = 0.001), hVMAT-1 and hVMAT-3 (p = 0.003), as well as hVMAT-1 and hVMAT-4 (p = 0.001). Furthermore, hVMAT-2 exhibited significant differences when compared to hVMAT-3 (p = 0.003), whereas no significant difference was observed between hVMAT-2 and hVMAT-4 (p = 0.217). Additionally, a significant difference was found between hVMAT-3 and hVMAT-4 (p = 0.01). For the V30Gy metric, the results were as follows: hVMAT-1 produced a mean of 11.52 ± 6.06%, hVMAT-2 yielded 11.47 ± 7.00%, hVMAT-3 achieved 14.19 ± 7.20% and hVMAT-4 resulted in 12.89 ± 6.57%. Statistically significant differences were identified between hVMAT-1 and hVMAT-3 (p = 0.001), hVMAT-1 and hVMAT-4 (p = 0.001) and hVMAT-2 and hVMAT-3 (p = 0.001), as well as hVMAT-2 and hVMAT-4 (p = 0.013). Conversely, no statistically significant difference was observed between hVMAT-1 and hVMAT-2 (p = 0.068), nor between hVMAT-3 and hVMAT-4 (p = 0.02).
Heart dose metrics
In terms of heart dose, hVMAT-1 administered 26.25 ± 4.89 Gy, hVMAT-2 administered 26.19 ± 5.27 Gy, hVMAT-3 administered 29.20 ± 5.21 Gy and hVMAT-4 administered 29.11 ± 5.54 Gy. There was no statistically significant difference between hVMAT-1 and hVMAT-2 (p=0.463). However, significant differences were noted between hVMAT-1 and hVMAT-3 (p = 0.025), as well as between hVMAT-1 and hVMAT-4 (p = 0.013). Additionally, significant differences were found between hVMAT-2 and hVMAT-3 (p < 0.001), and between hVMAT-2 and hVMAT-4 (p < 0.001), while no significant difference was observed between hVMAT-3 and hVMAT-4 (p = 0.542).
For V30 Gy percentage, hVMAT-1 delivered 33.91 ± 9.76%, hVMAT-2 delivered 35.01 ± 12.19 hVMAT-3 delivered 60.94 ± 20.40% and hVMAT-4 delivered 48.27 ± 16.96%. No significant difference was detected between hVMAT-1 and hVMAT-2 (p = 0.463), but significant differences were identified between hVMAT-1and hVMAT-3 (p < 0.001), hVMAT-1and hVMAT-4 (p < 0.001) and between hVMAT-2 and hVMAT-3 (p < 0.001). There was no significant difference between hVMAT-3 and hVMAT-4 (p = 0.068).
For V40Gy, the delivery percentages for hVMAT-1, hVMAT-2, hVMAT-3 and hVMAT-4 were 18.85 ± 6.77%, 20.01 ± 7.30%, 22.18 ± 6.68% and 24.70 ± 7.18%, respectively. Statistically significant differences were identified between hVMAT-1 and hVMAT-2 (p = 0.035), hVMAT-1 and hVMAT-3 (p = 0.002), hVMAT-1 and hVMAT-4 (p < 0.001) and hVMAT-2 and hVMAT-3 (p = 0.013), as well as hVMAT-2 and hVMAT-4 (p < 0.001). However, no significant difference was noted between hVMAT-3 and hVMAT-4 (p = 0.068).
Spinal cord dose metric
hVMAT-1 values recorded were 44.28 ± 4.15 Gy, 44.97 ± 3.78 Gy for hVMAT-2, 44.26 ± 3.95 Gy for hVMAT-3 and 45.10 ± 2.46 Gy for hVMAT-4. A significant difference was found between hVMAT-1 and hVMAT-2 (p = 0.024). No significant differences were observed between hVMAT-1 and hVMAT-3 (p = 0.308), hVMAT-1 and hVMAT-4 (p = 0.206), hVMAT-2 and hVMAT-3 (p = 0.083), hVMAT-2 and hVMAT-4 (P = 0.765) or between hVMAT-3 and hVMAT-4 (p = 0.147). In terms of spinal cord dose, hVMAT-4 (45.10±2.46 Gy) exhibited a greater maximum dose (Dmax) than the other hVMAT treatment plans.
Integral dose
The integral dose to the lungs (Gy-L) exhibited considerable variation among the four hybrid VMAT configurations. Specifically, hVMAT-1 administered a significantly lower dose of 31,643.97 ± 11,706.22 Gy-L, in contrast to hVMAT-2, which delivered 35,860.61 ± 12,573.48 Gy-L, hVMAT-3 at 32,194.59 ± 12,246.78 Gy-L and hVMAT-4 at 36,871.83 ± 14,232.83 Gy-L (p = 0.001 for all comparisons). Nevertheless, no significant differences were found between hVMAT-2 and hVMAT-3 (p = 0.810), hVMAT-2 and hVMAT-4 (p = 0.890) or between hVMAT-3 and hVMAT-4 (p = 0.689).
The integral dose to the heart (Gy-L) across the four hybrid VMAT configurations exhibited minimal variation. The hVMAT-1 configuration administered a dose of 12,315.32 ± 5,187.07 Gy-L, whereas hVMAT-2 provided a dose of 12,295.22 ± 5,320.50 Gy-L. Both hVMAT-3 and hVMAT-4 delivered comparable doses, measuring 13,479.23 ± 5,065.79 Gy-L and 13,505.27 ± 5,300.44 Gy-L, respectively. Statistical analysis indicated that there were no significant differences among any of the configurations, with a p= 0.899 for all comparisons.
Gamma analysis
Table 4 and Figure 5 provide detailed analysis of the gamma passing rates for different hybrid plans and criteria. The result of analysis reveals that the hVMAT-1 and hVMAT-3 plans do not differ significantly, which exhibited the highest gamma passing rates: 97.94±3.0 and 97.41 ± 5.64 (2%/2mm,p = 0.289), 98 ± 2.57 and 98.47 ± 4.65 (3%/2mm,p = 0.396) and 99.78 ± 0.51 and 98.88 ± 3.99 (3%/3mm,p = 0.260). On the other hand, the minimum gamma passing rates were consistently found with hVMAT-4, with values of 90.08±8.99 (2%/2mm), 93.25 ± 8.37 (3%/2mm) and 94.42 ± 8.12 (3%/3mm). Notably, hVMAT-2 and hVMAT-4 plans are statistically different (2%/2mm,p = 0.030, 3%/2mm,p = 0.031 and 3%/3mm,p = 0.017).
Table 4. The gamma analysis results using various dose differences or distance-to-agreement (DTA) criteria with a 10% dose threshold for four hybrid volumetric-modulated arc therapy (VMAT) plan
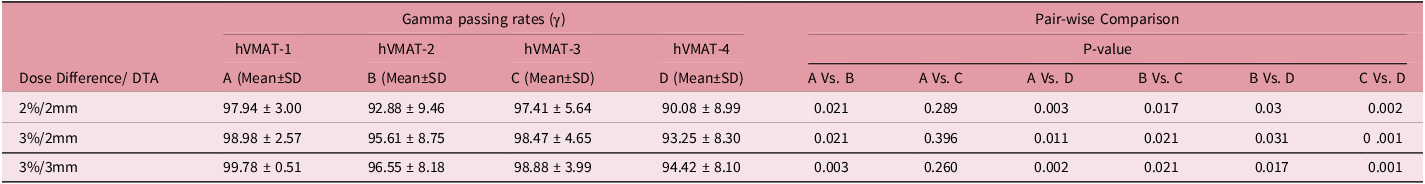
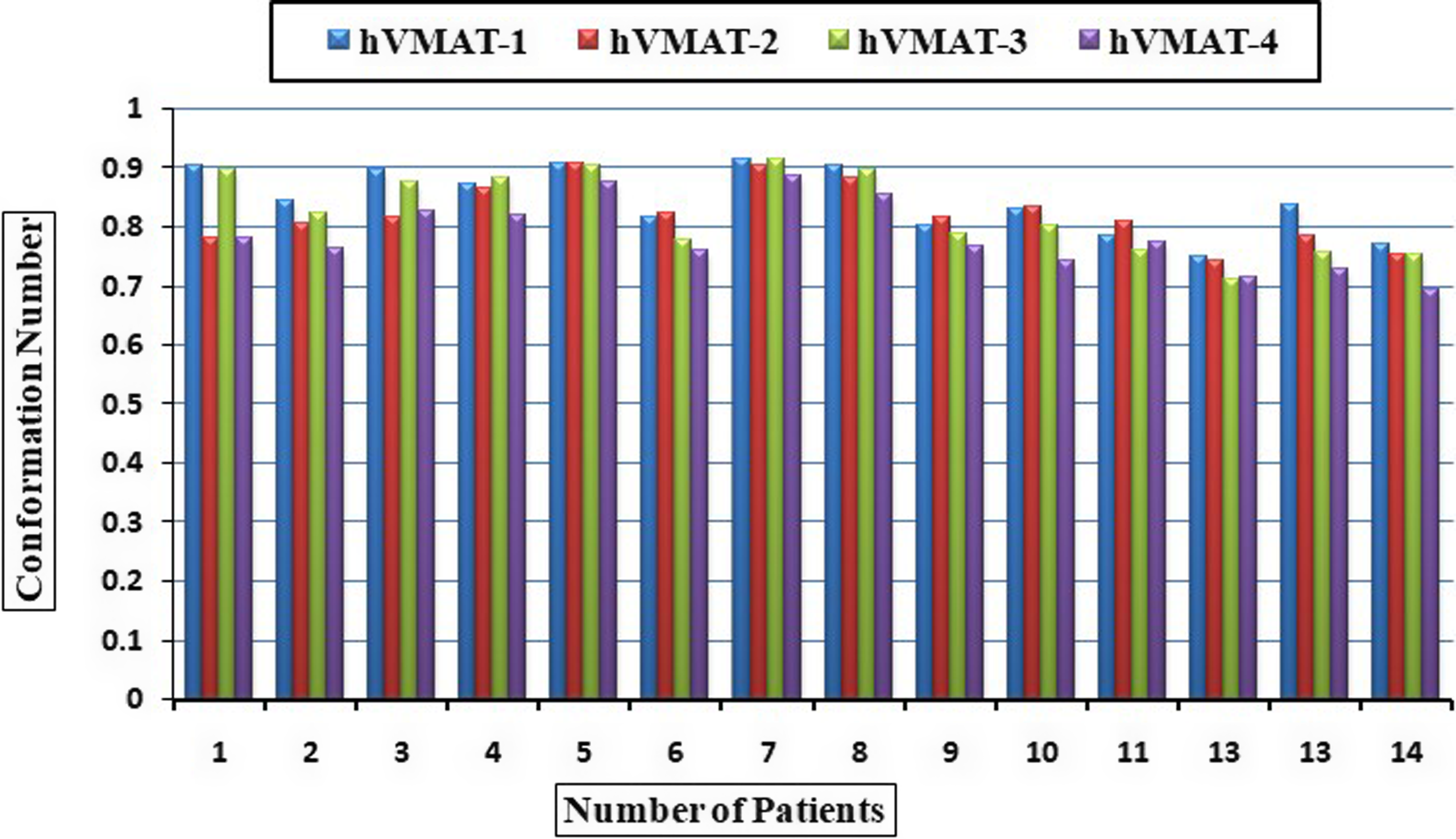
Figure 2. Variation of the conformation number across the four hybrid volumetric modulated arc therapy plan.
Discussion
The study conducted a comparative analysis of four hybrid VMAT (hVMAT) planning techniques for the treatment of oesophageal cancer, which combined 3D-conformal radiation therapy (3DCRT) with VMAT approaches. We evaluated two distinct 3DCRT strategies (AP-PA and AP-RPO-LPO) in conjunction with two different beam weight distributions (33%/67% and 67%/33% for 3DCRT/VMAT).
The analysis of the CN indicated that hVMAT-1 (0.85 ± 0.055) exhibited better performance than hVMAT-3 (0.83 ± 0.068) and hVMAT-4 (0.79 ± 0.059) as shown in Figure 2. This finding implies that the integration of AP-PA fields with a more substantial VMAT component may improve dose conformity, thereby potentially reducing complications in surrounding normal tissues. Our findings align with our recently published work (Zope et al.), Reference Zope, Patil and Saroj17 which demonstrated significant improvements in dosimetric parameters for hVMAT plans compared to both coplanar and non-coplanar techniques in the treatment of oesophageal cancer. This earlier published research involved the same group of patients as the present study. The study showed that hybrid plans enhanced conformity and homogeneity indices while reducing mean doses to critical organs such as the lungs and heart, emphasising the advantages of hybrid techniques in clinical practice.
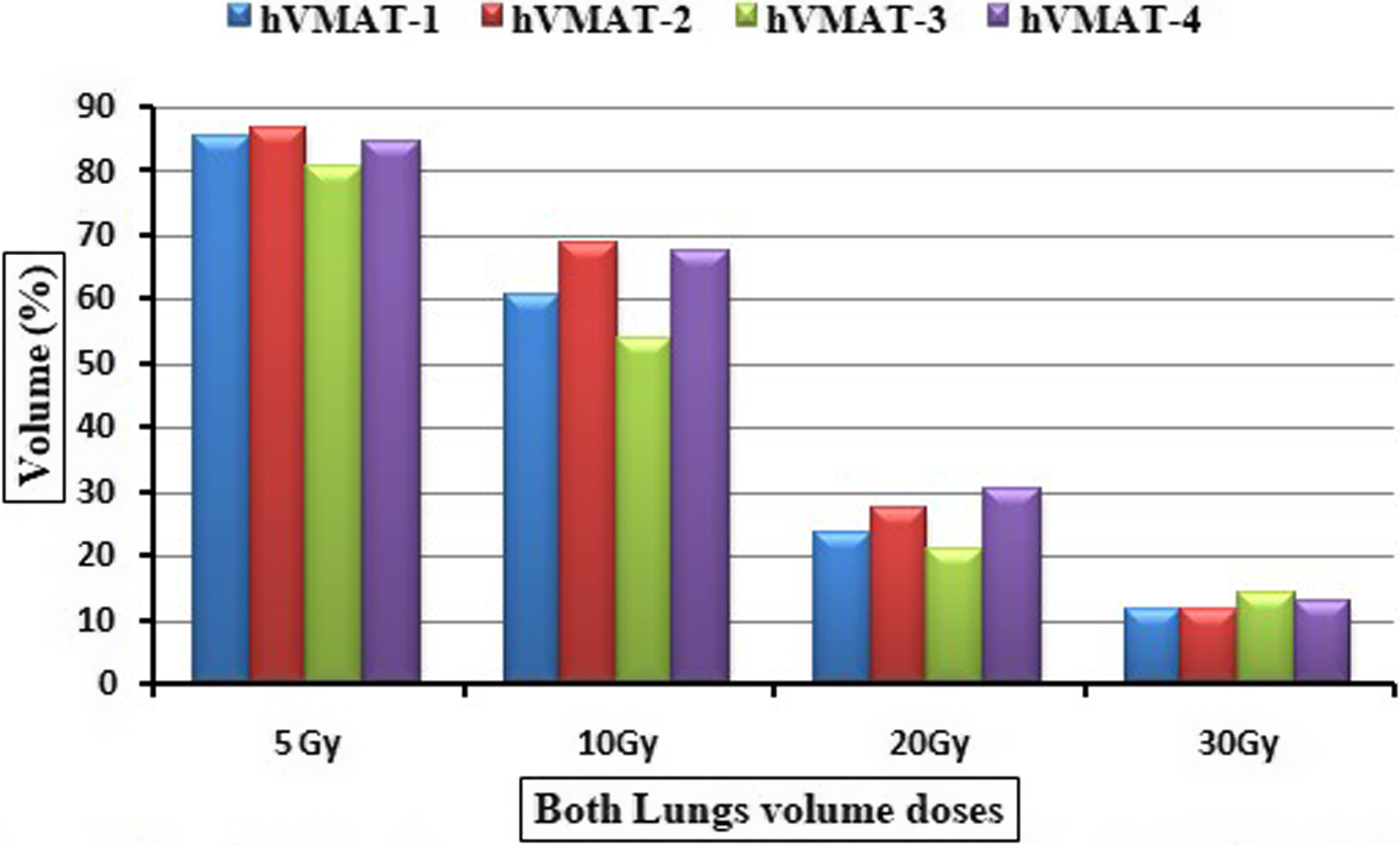
Figure 3. Heart dose variation across four hybrid volumetric modulated arc therapy plan.
Previous study by Münch, S et al., Reference Münch, Aichmeier, Hapfelmeier, Duma, Oechsner and Feith18 suggests that VMAT allows for higher radiation doses or the integration of 3DCRT and VMAT without damaging normal tissues. This advantage arises from VMAT’s precise targeting of the treatment area while sparing surrounding normal tissues. Takakusagi et al. Reference Takakusagi, Kusunoki, Kano, Anno and Tsuchida13 conducted a study comparing 3DCRT, hVMAT and VMAT techniques for patients with cT1bN0M0 oesophageal cancer. Their findings indicated that raising the VMAT component in hVMAT plans to between 50% and 70% led to a reduction in the mean heart dose and V30/V40 values, although this was accompanied by an increase in V5, V10, V20 and the mean lung dose (MLD). Our findings are consistent with those of Takakusagi et al., especially in relation to H-Arc-1 and H-Arc-2. The 67% VMAT component demonstrated a significant 15% decrease in the average heart dose, all while keeping lung V20 levels under the clinically acceptable limit of 25%.
Our study builds on and expands the existing literature in this area. Miyazaki et al. Reference Miyazaki, Ohira, Ueda, Isono, Fujiwara and Tanooka14 examined hVMAT plans that utilised a combination of 50% AP-PA beam and 50% VMAT in a cohort of 11 patients with oesophageal cancer. Their findings indicated that modifying the ratio of AP-PA beam to VMAT could lead to a reduction in lung doses. Additionally, Gong et al. Reference Chan, Lee, Hung, Chang, Yeung and Lee16 found that hVMAT plans enhanced conformity and decreased low-dose volumes for V5, V13, V20, V30 and MLD, thereby minimising the radiation exposure to healthy lung tissue, except V5. Our research not only supports the conclusions of earlier studies but also introduces significant advancements. In the cases of H-Arc-1 (33% 2F 3DCRT/67% RA) and H-Arc-2 (33% 3F 3DCRT/67% RA), we noted similar enhancements in dose conformity and protection of OARs. Additionally, our study presents new insights by exploring a wider range of hybrid configurations and their related dosimetric impacts.
Heart dose analysis and its clinical significance
Several studies have validated the risk of cardiac damage due to radiation exposure, especially at doses greater than 40 Gy. Reference Chun, Hu, Choy, Komaki, Timmerman and Schild19 In this study, we found that the hVMAT-1 and hVMAT-2 treatment plans yielded heart V40Gy values of 18.85% and 20.19%, respectively, both of which fall within acceptable thresholds. These results are particularly significant considering the findings by Pao et al., Reference Pao, Chang, Chiang, Lin, Lai and Tseng20 who established notable correlations between cardiac effusion and heart V30 >33%, as well as Dmean >20 Gy in IMRT for oesophageal cancer.
Our research enhances the growing knowledge of cardiac dose optimisation in radiotherapy for oesophageal cancer, expanding on the foundational studies conducted by Wei et al.. Reference Wei, Liu, Tucker, Wang, Mohan and Cox21 Their study highlighted a notable difference in the incidence of cardiac effusion, with rates of 13% when V30 is below 46% and 73% when V30 exceeds 46%. They also identified an average heart dose above 26.1 Gy as a potential threshold for cardiac complications.
In this study, hVMAT-1 and hVMAT-2 plans achieved significantly low heart V30Gy values of 33.91% and 35.01%, respectively, while keeping mean heart doses within the clinically acceptable limit of 26 Gy. This represents advancement over traditional methods and adheres to established cardiac dose limits. Although hVMAT-3 and hVMAT-4 achieved elevated values of 60.94% and 48.27%, respectively, they exceeded the average heart dose threshold by approximately 41.49% and 18.74%, respectively. Figure 4 illustrates the variation in heart volume doses among the four hVMAT techniques. The clear advantage of hVMAT-1 and hVMAT-2 in cardiac sparing compared to historical benchmarks and other hybrid techniques offers a strong basis for treatment planning. By demonstrating the capacity of specific hVMAT approaches to markedly reduce both V30Gy and mean heart dose, our study establishes a strong foundation for potentially reducing cardiac toxicity in radiotherapy for oesophageal cancer, thereby improving the overall therapeutic ratio.
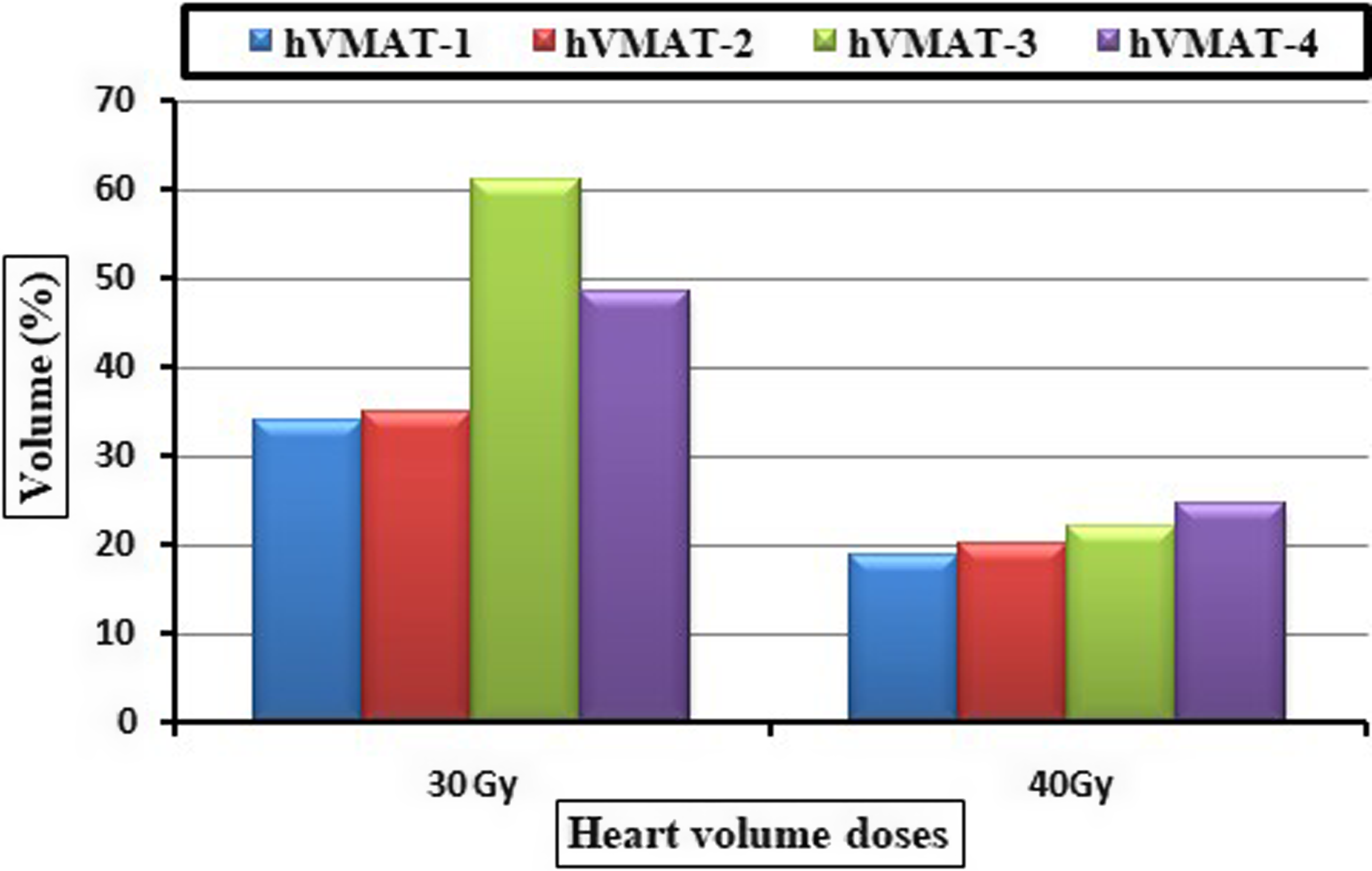
Figure 4. Variation in dose to both lungs across the four hybrid volumetric modulated arc therapy plan.
Lung dose assessment and its clinical significance:
Radiation-induced lung toxicities are influenced by the volume of lung tissue exposed, and minimising the irradiated lung volume can help reduce the likelihood of complications. Reference Williams and Newhauser22 Graham et al. Reference Graham, Purdy, Emami, Harms, Bosch and Lockett23 identified a significant relationship between pneumonitis and lung V20. In the context of radiotherapy for lung cancer, it is advisable to keep V20 below 30%–35% to prevent severe pneumonitis. Reference Marks, Bentzen, Deasy, Kong, Bradley and Vogelius24 Mayo et al. Reference Mayo, Urie, Fitzgerald, Ding, Lo and Bogdanov25 indicated that a total lung V20Gy of less than 25% corresponds to a low risk of pneumonitis, whereas Asakura et al. Reference Asakura, Hashimoto, Zenda, Harada, Hirakawa and Mizumoto26 reported that a V20 exceeding 37% increases the risk of radiation pneumonitis in patients undergoing treatment for EC. Furthermore, it was noted that pneumonitis is also linked to Dmean in the lungs, with suggested thresholds ranging from 20 to 23 Gy. Reference Chun, Hu, Choy, Komaki, Timmerman and Schild19
In our research, both V20 and the MLD in all hVMAT plans were maintained below clinically significant levels (25% and 17 Gy, respectively). Nonetheless, we noted an increase in low-dose regions and MLD with higher VMAT ratios. Jo et al. Reference Jo, Kay, Kim, Son, Kang and Jung27 proposed that a V5Gy greater than 65% signifies a considerable risk of pneumonitis. In our findings, hVMAT-2 had the highest V5Gy at 86.93%, followed by hVMAT-1 at 85.62%, hVMAT-4 at 84.66% and hVMAT-3 at 80.63%. Figure 3 illustrates the variation in both lung volume doses among the four hVMAT techniques. These results underscore the necessity of achieving a balance between high-dose and low-dose constraints when determining the most effective treatment strategy. Although hVMAT configurations with elevated VMAT components (hVMAT-1 and hVMAT-2) provided improved conformity and high-dose sparing, they also resulted in a greater distribution of low doses, which may adversely affect pulmonary function in patients with pre-existing compromised lung capacity.
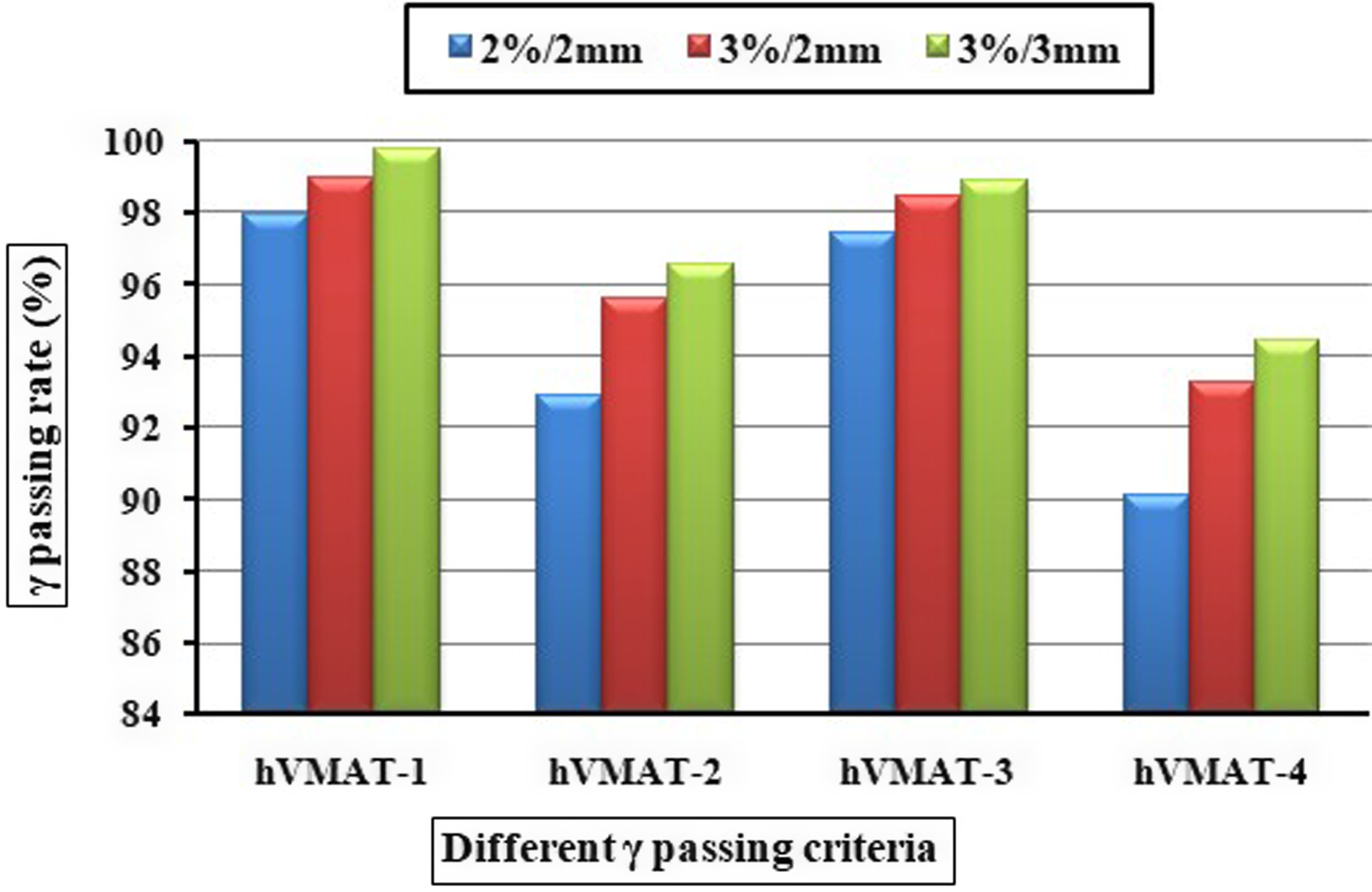
Figure 5. The variation in gamma (γ) passing rates (%) across four hybrid volumetric modulated arc therapy plan.
Spinal cord analysis:
Preserving the spinal cord is essential in the treatment of EC, particularly due to the potential for radiation-induced myelopathy when doses surpass 50 Gy. by Kirkpatrick et al. Reference Kirkpatrick, van der Kogel and Schultheiss28 reported myelopathy rates of 0.2%, 6%, and 50% for spinal cord doses of 50 Gy, 60 Gy, and 69 Gy, respectively. Our findings align with recent studies Reference Takakusagi, Kusunoki, Kano, Anno and Tsuchida13,Reference Miyazaki, Ohira, Ueda, Isono, Fujiwara and Tanooka14 that indicate hVMAT can significantly lower spinal cord exposure during EC treatment.
Integral dose analysis
Box plot analysis as shown in Figure 6 shows the interquartile range for integral dose is maximum for hVMAT-4 treatment plan for combined lungs and hearts. ID for lungs shows that the hVMAT-2 plans received the lowest ID score than its rival’s treatment plans. hVMAT-3 and hVMAT-4 give 9.4% and 9.6% more integral doses to the hearts compared to the hVMAT-2. ID analysis of combined lungs shows that hVMAT-1 achieved significantly lowest ID value compared to other HVMAT treatment plans. hVMAT-1 plans to deliver 13.3% and 16.6% less IDs compared to hVMAT-2 and hVMAT-4 respectively, while the hVMAT-3 plan delivers somewhat like hVMAT-1.
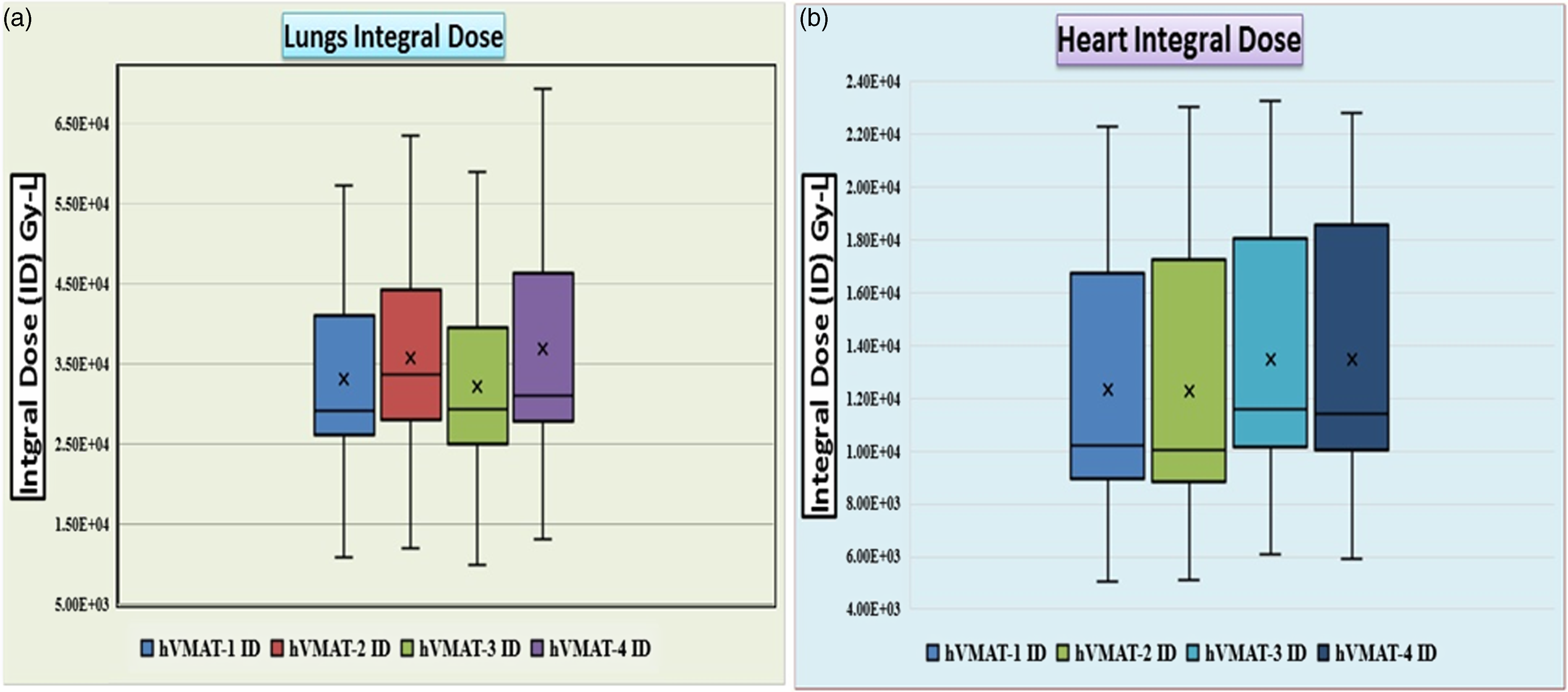
Figure 6. Shows the box plot of integral dose for both lungs (left) and heart (right).
Considerations for clinical implementation
From a practical perspective in radiotherapy, the hVMAT -1 technique offers several advantages that could improve its clinical use. Although our study is constrained by a small sample size (n = 14), the results indicate that this approach may enhance workflow efficiency by requiring fewer MUs compared to traditional VMAT techniques, potentially resulting in reduced treatment delivery times. Additionally, the simple beam configuration facilitates easier patient setup verification and quality assurance processes, which is especially advantageous in busy radiotherapy department. These practical factors are crucial for integrating this technique into standard radiotherapy practice, as they may enhance departmental efficiency while maintaining treatment quality.
The increased dose sparing to critical organs observed with hVMAT -1 and hVMAT -2 may enhance treatment tolerance and possibly decrease therapy interruptions, which are known to impact treatment results. While our pilot study primarily emphasises dosimetric outcomes, the demonstrated sparing of cardiac and pulmonary doses could have implications for minimising long-term toxicity, a major concern in radiotherapy for carcinoma of the oesophagus. The relationship between improved dosimetry and patient survival necessitates further exploration through larger clinical trials with extended follow-up durations. Radiotherapy departments contemplating the adoption of hybrid techniques should consider these potential advantages alongside the added complexity in planning that such techniques entail.
Considerations for clinical application
This study indicates several significant implications for the practice of radiotherapy in the treatment of carcinoma of the oesophagus. The hVMAT-1 and hVMAT-2 configurations, which integrate 33% 3DCRT with 67% VMAT, seem to provide benefits due to their improved dose conformity and lower toxicity levels for the heart and lungs. For facilities currently utilising either 3DCRT or VMAT exclusively, transitioning to this hybrid method could enhance the protection of critical organs while ensuring effective tumour coverage. This is particularly important considering the established link between radiation exposure to the heart and lungs and the associated treatment-related complications. When choosing between the hVMAT configurations, treatment planners must take into account individual patient factors, especially those related to cardiac and pulmonary risks, as these can significantly affect the suitability of each technique. Facilities adopting these hybrid techniques would benefit from developing standardised quality assurance protocols specifically designed for hybrid planning, as our gamma analysis indicated variability among the different hVMAT configurations.
Limitations
A key limitation of this study is that actual organ densities were not used in calculating the integral dose, and the small sample size may affect the generalizability of the findings. While the results show statistical significance, increasing the sample size would provide more robust and reliable outcomes. This study should be viewed as a pilot or preliminary exploration, highlighting the need for larger, more comprehensive studies to further validate these findings.
Conclusion
This pilot study serves as an initial investigation into the use of hybrid VMAT techniques for treating oesophageal cancer within a small group of patients. The findings suggest a promising opportunity to enhance radiation delivery while minimising exposure to critical organs. The hVMAT-1 and hVMAT-2 configurations demonstrated encouraging preliminary dosimetric outcomes, including improved dose conformity, decreased cardiac exposure and acceptable lung doses when compared to traditional methods. These initial results imply that a treatment strategy comprising 33% 3DCRT and 67% VMAT may effectively balance target coverage with the protection of OARs, although our current analysis has notable limitations.
Future research should focus on addressing the primary limitations identified in this study by assessing these initial dosimetric results in larger and more varied patient groups, while also correlating them with clinical outcomes, including treatment-related side effects, quality of life and survival rates. This approach would enhance the evidence supporting the incorporation of hybrid techniques into standard clinical practice for radiotherapy in carcinoma of the oesophagus.
Acknowledgements
Not applicable.
Competing interests
No.












