Introduction
Anxiety disorders (ADs) are the most prevalent psychiatric condition worldwide, with approximately 301 million people living with an anxiety-related problem (Our World in Data, 2019). Between 6.57% and 13.54% of new fathers have an AD (Leiferman et al., Reference Leiferman, Farewell, Jewell, Lacy, Walls, Harnke and Paulson2021), a considerably higher prevalence than of ADs in men generally, estimated to range between 2.2 and 3.8% (World Health Organization, 2017), suggesting that the transition to fatherhood may represent a risk factor for anxiety (Leiferman et al., Reference Leiferman, Farewell, Jewell, Lacy, Walls, Harnke and Paulson2021).
Perinatally, mental health problem onset or exacerbation is common in both fathers and mothers (Challacombe et al., Reference Challacombe, Pietikäinen, Kiviruusu, Saarenpää-Heikkilä, Paunio and Paavonen2023). Furthermore, maternal and paternal mental health are linked. For example, meta-analytic evidence shows that maternal depression increases the likelihood of paternal postnatal anxiety (odds ratio [OR] = 3.86, 95%CI [2.54–5.89]; Chhabra et al., Reference Chhabra, McDermott and Li2020).
Children’s mental health is affected by their parents’ mental health (Uher et al., Reference Uher, Pavlova, Radua, Provenzani, Najafi, Fortea, Ortuño, Nazarova, Perroud, Palaniyappan, Domschke, Cortese, Arnold, Austin, Vanyukov, Weissman, Young, Hillegers, Danese and Fusar‐Poli2023). Particularly, a substantial body of evidence indicates that children whose parents have ADs, compared to children whose parents do not, have a significantly higher risk of mental health problems (Ahmadzadeh et al., Reference Ahmadzadeh, Schoeler, Han, Pingault, Creswell and McAdams2021; Lawrence et al., Reference Lawrence, Murayama and Creswell2019; Uher et al., Reference Uher, Pavlova, Radua, Provenzani, Najafi, Fortea, Ortuño, Nazarova, Perroud, Palaniyappan, Domschke, Cortese, Arnold, Austin, Vanyukov, Weissman, Young, Hillegers, Danese and Fusar‐Poli2023; Zecchinato et al., Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024). Developmental theories suggest that the rearing environment provided by parents pre- and postnatally, including parental traits and behaviors, and parenting styles, has a key impact on offspring emotional development and social competence, for instance via parental emotion socialisation (Eisenberg et al., Reference Eisenberg, Cumberland and Spinrad1998; Eisenberg, Reference Eisenberg2020) and social learning processes (Bandura & Walters, Reference Bandura and Walters1977; Grusec, Reference Grusec1994; Olsson & Phelps, Reference Olsson and Phelps2007; Patterson, Reference Patterson2002). According to these models, the ways in which parents respond to their children’s emotional expressions, the extent and type of emotional expressions by parents, and the frequency with which parents engage in (dys)functional discussions and communications about emotions serve as a model for children, shaping their understanding, regulation, and expression of emotions, as well as their social behaviors and the cognitive-affective representations of the self and others (Eisenberg et al., Reference Eisenberg, Cumberland and Spinrad1998; Eisenberg, Reference Eisenberg2020; Grusec, Reference Grusec1994). Moreover, as a child shares 50% of their genes with each biological parent and considering that many traits, including mental health issues, are heritable, any parent-offspring association could be, at least partly, due to shared genes, reflecting a genetic transmission pathway (Jami et al., Reference Jami, Hammerschlag, Bartels and Middeldorp2021). Crucially, conceptual models of intergenerational transmission of mental illness recognize the complex interplay between experientially and genetically mediated risk transmission as biological parents provide both – they pass on their genes and create the rearing environments for their children (e.g., Jami et al., Reference Jami, Hammerschlag, Bartels and Middeldorp2021; Rutter et al., Reference Rutter, Moffitt and Caspi2006).
Father-specific contributions to children’s mental health difficulties have been under-investigated, especially compared to maternal-specific contributions (Bögels & Phares, Reference Bögels and Phares2008). Further, the risk posed by paternal anxiety, particularly perinatally, for offspring mental health difficulties is unclear (Bögels & Phares, Reference Bögels and Phares2008; Zecchinato et al., Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024). However, a growing body of research supports the crucial importance of shedding light on the role of fathers in their children’s development (Connell & Goodman, Reference Connell and Goodman2002; Sweeney & MacBeth, Reference Sweeney and MacBeth2016; Trepiak et al., Reference Trepiak, Trepiak, Guérin-Marion, Kristen and Deneault2022; Zecchinato et al., Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024). In a recent meta-analysis examining the associations between fathers’ anxiety and offspring adverse outcomes, Zecchinato et al. (Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024) found significant, positive associations between paternal anxiety and offspring emotional and behavioral problems overall (r = .16, 95%CI [.13, .19], N = 54,998), as well as behavioral (r = .19, 95%CI [.13, .24], n = 10,958), emotional (r = .15, 95%CI [.12, .18], n = 52,327), anxiety (r = .13, 95%CI [.11, .16], n = 47,113), and depression outcomes (r = .13, 95%CI [.03, .23], n = 4,502). Nevertheless, only a relatively small number of studies have examined the association between paternal anxiety and offspring behavioral outcomes. Moreover, the risk posed by indirect and direct exposure to paternal anxiety perinatally, specifically for child emotional and behavioral development, is also poorly understood (Challacombe et al., Reference Challacombe, Pietikäinen, Kiviruusu, Saarenpää-Heikkilä, Paunio and Paavonen2023). Although Zecchinato et al. (Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024) found no significant moderating effect of the associations between paternal anxiety and offspring mental health by time-lag between paternal and offspring assessments or by offspring age in their meta-analysis, suggesting that paternal anxiety may represent a risk factor for offspring across the lifespan, it is well established that during a lifespan there are sensitive periods when risk and protective factors could increase or decrease vulnerability to mental illness and have long-lasting consequences (Arango et al., Reference Arango, Díaz-Caneja, McGorry, Rapoport, Sommer, Vorstman, McDaid, Marín, Serrano-Drozdowskyj, Freedman and Carpenter2018; Michael et al., Reference Michael, Gard, Tillem, Hardi, Dunn, Smith, McLoyd, Brooks-Gunn, Mitchell, Monk and Hyde2024; Nelson et al., Reference Nelson, Sullivan and Engelstad2024). The perinatal period specifically represents a window of major developmental brain changes and is crucial for the development of secure attachment, basic schemas related to self, others, and the world, the regulation of physiological and behavioral responses, and the adult personality (Arango et al., Reference Arango, Díaz-Caneja, McGorry, Rapoport, Sommer, Vorstman, McDaid, Marín, Serrano-Drozdowskyj, Freedman and Carpenter2018; Nelson et al., Reference Nelson, Sullivan and Engelstad2024). Moreover, research on early interactions shows that anxious caregivers tend to be over-responsive to their children, displaying over-controlling or intrusive behaviors, and this interaction style can lead to atypical attachment patterns (Beebe et al., Reference Beebe, Steele, Jaffe, Buck, Chen, Cohen, Kaitz, Markese, Andrews, Margolis and Feldstein2011; Feldman, Reference Feldman2007; Smith et al., Reference Smith, Kievit and Astle2023). Considering that the perinatal period is a time of heightened parental anxiety (Challacombe et al., Reference Challacombe, Pietikäinen, Kiviruusu, Saarenpää-Heikkilä, Paunio and Paavonen2023; Leiferman et al., Reference Leiferman, Farewell, Jewell, Lacy, Walls, Harnke and Paulson2021), that early infancy represents a sensitive window for development (Nelson et al., Reference Nelson, Sullivan and Engelstad2024), and that the prevention of child mental illness is a recognized priority (Doyle et al., Reference Doyle, Harmon, Heckman and Tremblay2009; McGorry et al., Reference McGorry, Mei, Dalal, Alvarez-Jimenez, Blakemore, Browne, Dooley, Hickie, Jones, McDaid, Mihalopoulos, Wood, El Azzouzi, Fazio, Gow, Hanjabam, Hayes, Morris, Pang and Killackey2024), it is crucial to better understand the specific impact of exposure to paternal perinatal anxiety on later child outcomes. Such insights would inform the development of timely, targeted preventive interventions and guide broader prevention efforts.
Further, prior examinations of risk transmission from fathers’ anxiety have omitted to account for factors that can be important in the intergenerational transmission of risk of psychopathology, as suggested by theoretical models for the transmission of risk from mothers (Goodman & Gotlib, Reference Goodman and Gotlib1999) and fathers (Ramchandani & Psychogiou, Reference Ramchandani and Psychogiou2009) to their children, including maternal and paternal current and past mental health, child temperament, and sociodemographic variables such as parent education, race/ethnicity, age, and social class.
Additional support for the importance of investigating the father-specific contribution to offspring development comes from theoretical and empirical evidence suggesting that fathers and mothers are likely to have different impacts on their children’s behavioral and emotional outcomes (Bögels & Phares, Reference Bögels and Phares2008; Fisher et al., Reference Fisher, Cobo, Figueiredo, Fletcher, Garfield, Hanley, Ramchandani and Singley2021; Natsuaki et al., Reference Natsuaki, Shaw, Neiderhiser, Ganiban, Harold, Reiss and Leve2014; Ramchandani & Psychogiou, Reference Ramchandani and Psychogiou2009). Specifically, it is proposed that their evolutionary-based prominent role in the socialisation and encouragement of their children’s autonomy may make fathers particularly central for children’s resilience and socioemotional development (Feldman, Reference Feldman2023). In turn, this unique role is likely to be negatively impacted by paternal psychopathology, including anxiety, thus increasing the risk of the development of emotional problems in their children (Bögels & Phares, Reference Bögels and Phares2008; Bögels & Perotti, Reference Bögels and Perotti2011; Majdandžić et al., Reference Majdandžić, Möller, de Vente, Bögels and van den Boom2014; Ramchandani & Psychogiou, Reference Ramchandani and Psychogiou2009; Winnicott, Reference Winnicott1964). Finally, it is important to account for the societal changes that have characterized parenthood in the last few decades, which are generally leading to an increasing involvement of fathers in childcare roles and a simultaneous growing participation of mothers in the workforce (e.g., Cabrera et al., Reference Cabrera, Tamis-LeMonda, Bradley, Hofferth and Lamb2000; Feldman, Reference Feldman2023). An increased presence of fathers in their children’s lives may lead to a stronger influence of paternal mental health on their offspring developmental outcomes, underscoring the need of studying fathers’ contribution to child mental health.
Crucially, the mechanisms of intergenerational transmission of psychopathology in the context of paternal anxiety remain poorly understood. The degree to which psychosocial risks operate directly through psychosocial mechanisms is a central theoretical question in developmental psychopathology. Different timings of parental mental illness (including offspring exposure pre- and/or postnatally) may be linked to specific pathways in relation to child outcomes (Rajyaguru et al., Reference Rajyaguru, Kwong, Braithwaite and Pearson2021; Stein et al., Reference Stein, Pearson, Goodman, Rapa, Rahman, McCallum, Howard and Pariante2014). Substantial evidence supports the key importance of environmental mechanisms (e.g., parental context, altered parenting behaviors), even when accounting for genetic predisposition (Ahmadzadeh et al., Reference Ahmadzadeh, Eley, Leve, Shaw, Natsuaki, Reiss, Neiderhiser and McAdams2019; Eley et al., Reference Eley, McAdams, Rijsdijk, Lichtenstein, Narusyte, Reiss, Spotts, Ganiban and Neiderhiser2015; Jami et al., Reference Jami, Hammerschlag, Bartels and Middeldorp2021; Murray et al., Reference Murray, Creswell and Cooper2009; Purves et al., Reference Purves, Coleman, Meier, Rayner, Davis, Cheesman, Bækvad-Hansen, Børglum, Wan Cho, Jürgen Deckert, Gaspar, Bybjerg-Grauholm, Hettema, Hotopf, Hougaard, Hübel, Kan, McIntosh and Eley2020). Nevertheless, when studying the intergenerational transmission of psychopathology and the nature of risk mechanisms, it is key to distinguish between prenatal and postnatal parental psychopathology and compare direct with indirect exposure (Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008), as existing evidence is inconsistent. Some suggest sufficiency of prenatal (indirect) exposure to psychosocial risks (e.g., parental mental ill-health) alone for poor child psychological adjustment (Barker et al., Reference Barker, Jaffee, Uher and Maughan2011). For instance, fathers might influence child development prenatally exerting an impact on maternal mental health, and thus affecting the foetus during pregnancy (e.g., Psouni & Eichbichler, Reference Psouni and Eichbichler2020; Ramchandani & Psychogiou, Reference Ramchandani and Psychogiou2009; Sethna et al., Reference Sethna, Murray, Netsi, Psychogiou and Ramchandani2015), in line with the biological programing hypothesis (Van den Bergh et al., Reference Van den Bergh, Mulder, Mennes and Glover2005). Some suggest that direct postnatal exposure to parent mental ill-health alone is sufficient to observe adverse offspring outcomes (Ahmadzadeh et al., Reference Ahmadzadeh, Schoeler, Han, Pingault, Creswell and McAdams2021). We propose that postnatal exposure alone, compared to prenatal exposure alone, might be associated with greater adversity in children as it would reflect risk transmitted via environmental means, including altered parenting behavior, in addition to potential underlying genetic risk. Furthermore, the postnatal period represents a richer and more dynamic environment for parent-child interactions compared to the prenatal period. During this time, children engage in multimodal interactions with their caregivers, involving visual, auditory, tactile, and olfactory stimuli, which are critical for early emotional and behavioral development (Dunn, Reference Dunn2004; Göksun et al., Reference Göksun, Aktan-Erciyes, Karadöller and Demir-Lira2024; Tanaka et al., Reference Tanaka, Fukushima, Okanoya and Myowa-Yamakoshi2014). This increased range of modes for parental input postnatally means that parental behaviors have more ways to shape their children, so the influence of parental mental health is amplified (Bronfenbrenner, Reference Bronfenbrenner1979; Dunn, Reference Dunn2004). While mechanisms were not the primary focus here, this study’s approach to differential timings of exposure effects may provide fundamental insights into potential pathways of intergenerational risk transmission, opening avenues for future research.
To specifically examine the differential effects of paternal prenatal-only and postnatal-only depression for children’s subsequent emotional and behavioral functioning, Ramchandani et al. (Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008) used the data from a large cohort study and conducted a natural experimental design, comparing only prenatal to only postnatal (and to both prenatal and postnatal) exposure to paternal depression. Children whose fathers were depressed both pre- and postnatally, compared to children whose fathers were not depressed, had the highest risks of emotional and behavioral problems at 3 years, 6 months (OR = 3.55, 95%CI [2.07, 6.08]) and psychiatric diagnosis at 7 years, 7 months (OR = 2.54, 95%CI [1.19, 5.41]) (Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008), highlighting the cumulative risk of adverse outcomes posed by prolonged exposure to paternal depression across both prenatal and postnatal periods. Moreover, when compared to fathers who were not depressed, male offspring whose fathers had postnatal depression only had higher rates of conduct problems at 3 years, 6 months, whereas male offspring of the prenatal only group did not, underscoring the particular relevance of direct exposure to paternal depression during the postnatal period for certain developmental outcomes, particularly in boys (Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008). However, no studies have been conducted to disentangle the impact of timing of paternal perinatal anxiety on child mental health.
Study aims
We aimed to elucidate fathers’ contribution to the intergenerational transmission of psychopathology and test different timings of paternal perinatal anxiety (prenatal-only, postnatal-only, and paternal anxiety both pre- and postnatally) in relation to children’s subsequent psychological functioning. Building on existing theoretical frameworks on risk transmission from depressed mothers to children (Goodman & Gotlib, Reference Goodman and Gotlib1999) and from fathers to children (Ramchandani & Psychogiou, Reference Ramchandani and Psychogiou2009) and empirical evidence (Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008; Sandstrom et al., Reference Sandstrom, Uher and Pavlova2020; Zecchinato et al., Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024) highlighting the importance of the familial context (sociodemographic characteristics, paternal and maternal current and past mental health) and child temperament in intergenerational risk transmission, we also controlled for these variables when analyzing the relationship between paternal anxiety and child outcomes. This approach allowed us to account for potential confounding relationships, although we do not refer to these variables as confounders to avoid making untested assumptions about their causal associations with both the exposure and the outcome, particularly given the possibility of their involvement in the causal pathway (Hernán & Robins, Reference Hernán and Robins2010; VanderWeele, Reference VanderWeele2015). Following the study design by Ramchandani et al. (Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008) and using the data from the ALSPAC cohort, we employed a prospective study design to compare child outcomes (also specifying between behavioral and emotional difficulties) at 3 years, 6 months and at 7 years, 7 months in four mutually exclusive groups: 1) children whose fathers were anxious neither prenatally nor postnatally (non-anxious group); 2) children whose fathers were anxious prenatally only (prenatal-only group); 3) children whose fathers were anxious postnatally only (postnatal-only group); and 4) children whose fathers were anxious both prenatally and postnatally (anxious-at-both-times group). The unique research design presented here allowed us to explore patterns of data that could indicate different mechanisms by which the intergenerational transmission of risk from fathers to their offspring may occur, although the underlying mechanisms were not directly tested in this study.
We hypothesized that:
-
a. paternal anxiety would represent a risk factor for child outcomes at both 3 years, 6 months and 7 years, 7 months; hence, we predicted a difference between the non-anxious group (1) and all three anxious groups (groups 2, 3 and 4), with worse emotional and/or behavioral outcomes in 2, 3, and 4, compared to 1;
-
b. direct psychological exposure (group 3) would predict more severe child emotional/behavioral outcomes than indirect exposure alone (group 2), considering that the postnatal period represents a more complex and dynamic environment for parent-child interactions compared to the prenatal period and that it would reflect risk transmitted via environmental means, including altered parenting behavior, in addition to potential underlying genetic risk; hence, we expected that children with fathers in the postnatal-only group (3) would show worse outcomes than children in the prenatal-only group (2);
-
c. the group of children exposed to paternal anxiety at both times (4), compared to groups 1, 2 and 3, would be at greater, cumulative risk of adverse behavioral/emotional outcomes.
Figure 1 provides a visual representation of the study hypotheses.
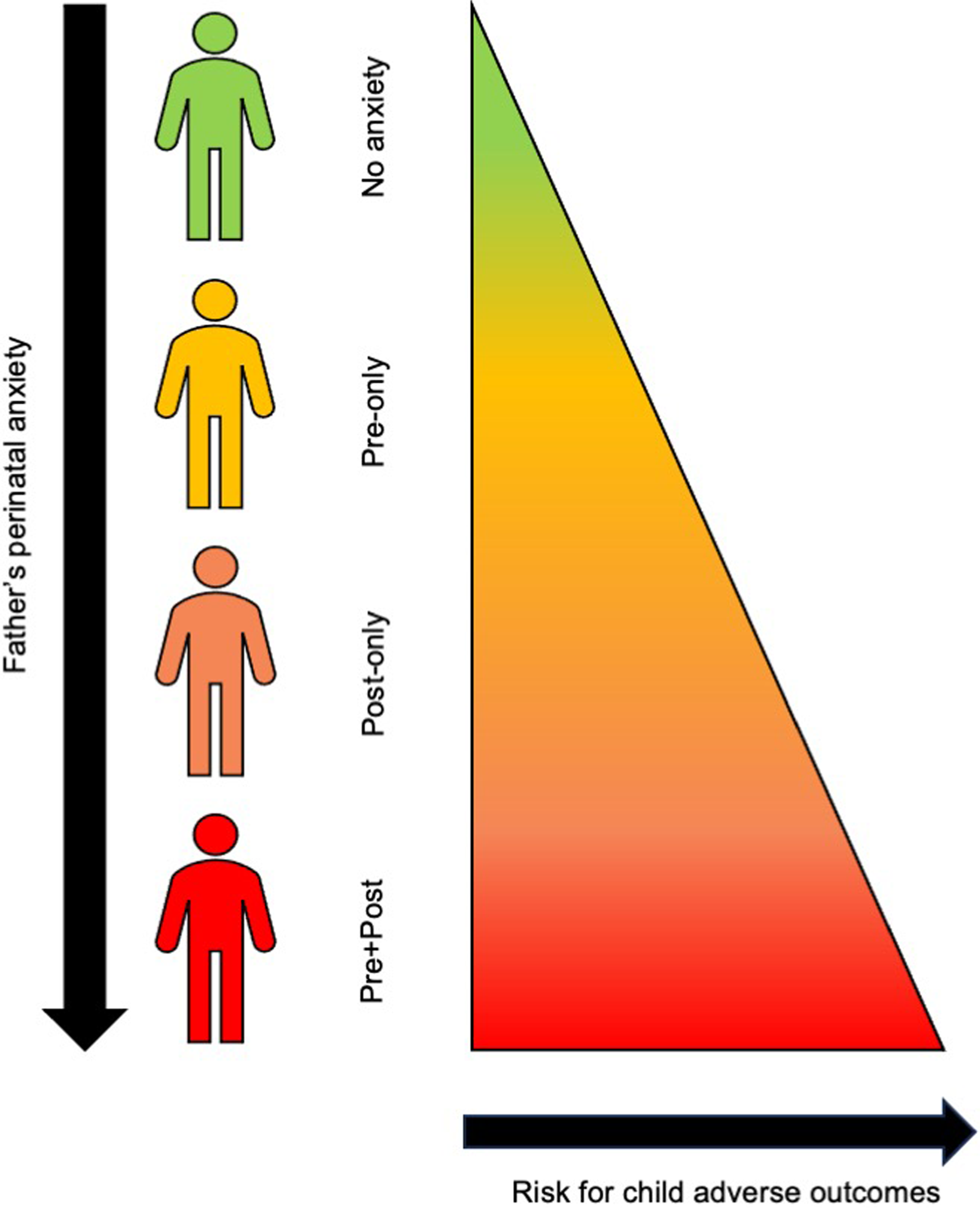
Figure 1. Visual representation of the study hypotheses. Note. No anxiety = fathers who were anxious neither prenatally nor postnatally; pre-only = fathers who were anxious only prenatally (18-week gestation assessment); post-only = fathers who were anxious only postnatally (8-week postnatal assessment); pre+post = fathers who were anxious both pre- and postnatally (18-week gestation assessment and 8-week postnatal assessment).
Methods
The sample comprised participants from the Avon Longitudinal Study of Parents and Children (ALSPAC; Golding et al., Reference Golding2001), a large, population-based birth cohort. Pregnant women resident in Avon, UK with expected delivery dates between 1st April 1991 and 31st December 1992 were invited to participate; the initial number of pregnancies enrolled was 14,541, and 13,988 had children who were alive at 1 year of age. 14,203 unique mothers were initially enrolled in the study. Partners were invited to complete questionnaires by the mothers at the start of the study and they were not formally enrolled at that time; 12,113 unique partners have been in contact with the study by providing data and/or formally enrolling when this started in 2010, and 3,807 partners are currently enrolled. We included the subsample of participants with complete exposure (i.e., paternal prenatal and postnatal anxiety) and offspring outcome (at 3 years, 6 months and 7 years, 7 months) data. Figure 2 gives an overview of the study sample derivation. As a note, because it was the participating mother who nominated the person who completed the partner questionnaires, those participants could be the biological father of the index child, the mother’s current partner, or a father-figure in the child’s life. To control for this, we conducted sensitivity analyses including only the subgroup of participants where the biological father was living with the family at the 3-year assessment.
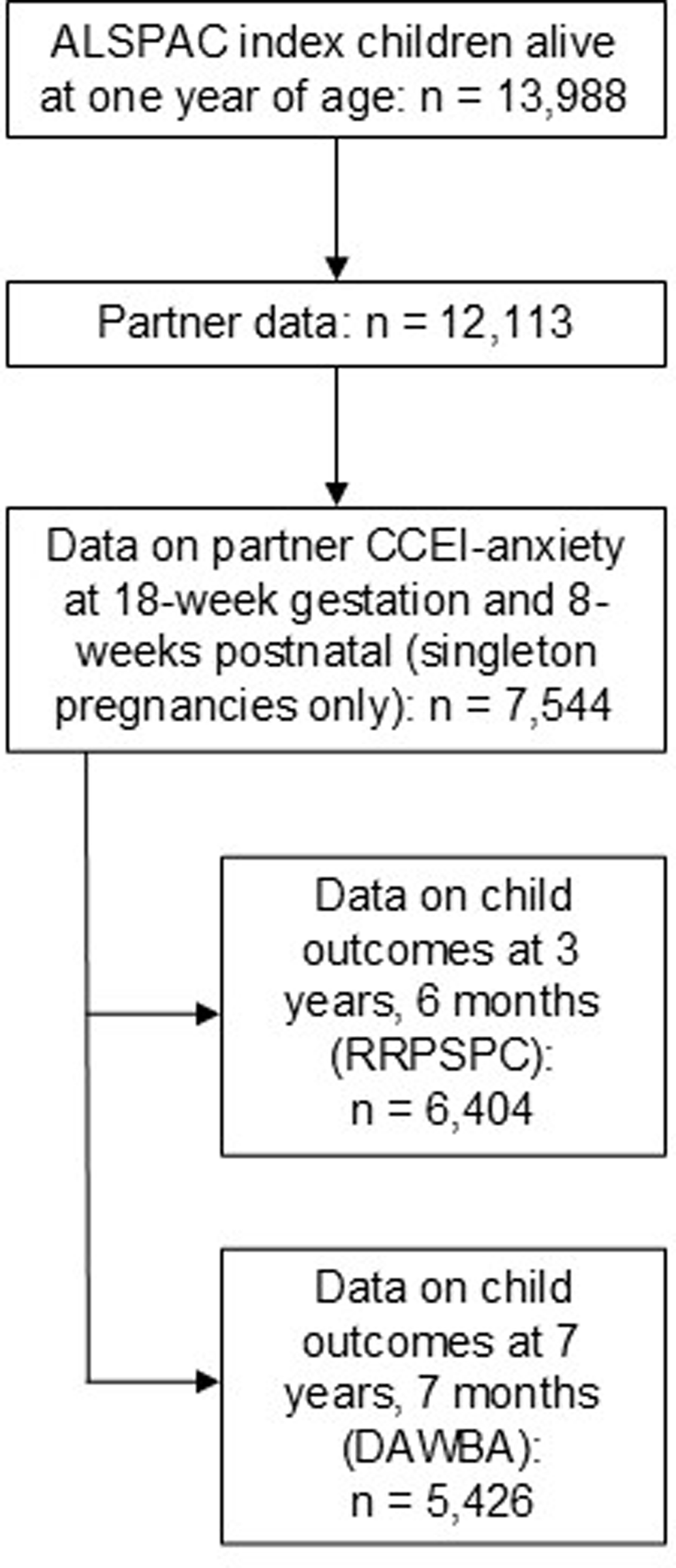
Figure 2. Overview of the study sample derivation. Note. ALSPAC = Avon Longitudinal Study of Parents and Children; CCEI = Crown-Crisp Experiential Index; RRPSPC = Revised Rutter Parent Scale for Preschool Children; DAWBA = Development and Wellbeing Assessment - Parent Questionnaire.
To maximize analytical power to examine magnitude of risk and confounding effects, we used all available data from exposures and outcomes. All missing data from the covariates were imputed via multiple imputation before conducting the adjusted logistic regressions (White et al., Reference White, Royston and Wood2011). Given that there is substantial information on sociodemographic variables in ALSPAC that predict missingness, missing information can be assumed dependent on observed data. Thus, we employed a fully conditional specification using the mice() function from the MICE package (which stands for stands for multivariate imputation by chained equations; Van Buuren & Groothuis-Oudshoorn, Reference Van Buuren and Groothuis-Oudshoorn2011) in R. For each variable included in our adjusted models, we used the default imputation method in the mice() function, which is predictive mean matching for continuous variables and logistic regression for binary variables. Two distinct imputed datasets were created, one for the analyses looking at the child outcomes at 3 years, 6 months and one for the analyses looking at the child outcomes at 7 years, 7 months. Analyses for the adjusted models were conducted post-imputation. Full details of the imputation method are in Appendix S1, available online.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. Ethical approval and informed consent were obtained for all procedures involving human participants from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees (http://www.bristol.ac.uk/alspac/researchers/research-ethics/) and from the University of Southampton Research Governance and Ethics Committee (ERGO ID: 88,927). Information about ALSPAC is available at www.bristol.ac.uk/alspac/, including a fully searchable data dictionary and variable search tool (http://www.bris.ac.uk/alspac/researchers/our-data/). Further details on the cohort profile, representativeness and phases of recruitment are described in three cohort-profile papers (Boyd et al., Reference Boyd, Golding, Macleod, Lawlor, Fraser, Henderson, Molloy, Ness, Ring and Davey Smith2013; Fraser et al., Reference Fraser, Macdonald-Wallis, Tilling, Boyd, Golding, Davey Smith, Henderson, Macleod, Molloy, Ness, Ring, Nelson and Lawlor2013; Northstone et al., Reference Northstone, Shlomo, Teyhan, Hill, Groom, Mumme, Timpson and Golding2023).
Study design
We used the available ALSPAC data to create four mutually exclusive groups for comparison: non-anxious (1), prenatal-only (2), postnatal-only (3), anxious-at-both-times (4). This study design allowed us to disaggregate direct (i.e., postnatal) from indirect (i.e., prenatal) exposure as mechanisms of risk transmission. Hence, we could test whether direct exposure, compared to indirect exposure, to paternal anxiety predicts greater risk of offspring emotional and behavioral outcomes. The logic and key comparisons of the design are as follows:
-
a. if paternal anxiety carries no risk for the child (via any risk mechanism), then there should be no difference between the non-anxious (1) and any of the three anxious groups (2, 3 and 4). This is the initial null hypothesis, representing an important baseline.
-
b. The second comparison was between the non-anxious group (1) and the prenatal-only (2) and postnatal-only (3) groups. If direct exposure to paternal anxiety is sufficient for adverse outcomes in offspring, then the children with fathers in the postnatal-only group (3) would show worse outcomes than children in the non-anxious (1) and prenatal-only (2) groups.
-
c. The third comparison of interest was between the prenatal-only group (2) and both the postnatal-only (3) and the anxious-at-both-times (4) groups, which provided an additional test of the exposure effect (i.e., anxious-at-both-times and postnatal-only > prenatal-only), as well as of severity (i.e., non-anxious < prenatal only < postnatal only < anxious-at-both-times), where children in the group with fathers anxious at both times (4) might be expected to experience higher rates of behavioral/emotional difficulties than seen in groups 1, 2 or 3.
Measures
Paternal anxiety
Paternal anxiety was measured at 18-weeks’ gestation and at 8-weeks postnatally using the 8-item anxiety subscale of the Crown-Crisp Experiential Index (CCEI; Crown & Crisp, Reference Crown and Crisp1970), a validated self-rating inventory that assesses the frequency in which the respondent experiences a range of anxiety symptoms at the present time from ‘never’ to ‘very often’ (e.g., “Do you feel uneasy and restless?”; “Do you worry a lot?”). We used the ALSPAC pro-rated scores (i.e., for missing items, scores were pro-rated using individual’s mode, unless all items were missing) and considered a cut-off of the top 15% of scorers to define high anxiety levels (Capron et al., Reference Capron, Glover, Pearson, Evans, O’Connor, Stein, Murphy and Ramchandani2015).
Offspring outcomes
Our primary outcomes were any child mental health problems at 3 years, 6 months and at 7 years, 7 months.
Offspring emotional and behavioral outcomes at 3 years, 6 months were assessed with the Revised Rutter Parent Scale for Preschool Children (RRPSPC; Elander & Rutter, Reference Elander and Rutter1996), maternal report. Items combine to form three problem scales (emotional problems, conduct problems and hyperactivity), and a prosocial behaviors scale. All problem scales combine to give a total problems scale. We used a cut-off of the top 10% of scorers to define high-scorers (Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008). The RRPSPC has no subscale specifically for behavioral difficulties, thus children were considered ‘high’ in behavioral problems if they scored in the top 10% in either the conduct or hyperactivity scales (or both).
Offspring emotional and behavioral outcomes at 7 years, 7 months were assessed with the Development and Wellbeing Assessment-Parent Questionnaire (DAWBA; Goodman et al., Reference Goodman, Ford, Richards, Gatward and Meltzer2000), maternal and teacher report for attention deficit hyperactivity disorder, oppositional defiant disorder and conduct disorder, and maternal report only for the other disorders. The questionnaire assesses the presence of psychiatric symptoms and their impact on children’s functioning, generating probable DSM-IV psychiatric diagnoses (DSM-IV-TR., 2000), confirmed by experienced clinical raters.
Paternal and maternal mental health
We included information on paternal and maternal self-reported current and past mental ill-health, specifically: history of severe depression and other psychiatric problems – self-reported (yes/no response) at 12-weeks’ gestation for mothers and fathers; anxiety measured via the CCEI at 18-weeks’ gestation and 8-weeks postnatally for mothers, and at 73-months for both parents; depression via the Edinburgh Postnatal Depression Scale (10-item; EPDS; Cox et al., Reference Cox, Holden and Sagovsky1987) at 18-weeks’ gestation, 8-weeks postnatally, and 73-months for mothers and fathers (using a cut-off score of >12 to identify high depression; Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008).
Sociodemographic variables
We included fathers’ age and the number of other children in the family at the time of index children’s birth (6-month assessment); and paternal: education (18-weeks’ gestation assessment); racial identity (32-weeks’ gestation assessment, maternal report); social class (32-weeks’ gestation assessment, maternal report, measured as the number of partners in professional or managerial and technical occupations); and marital status (12-weeks’ gestation assessment).
Child temperament
We included information on child temperament, assessed with the Carey Infant Temperament Scale (Carey & McDevitt, Reference Carey and McDevitt1978), mother-report at 24-months, including 88-items and nine separate subscales (i.e., activity, rhythmicity, approach, adaptability, intensity, mood, persistence, distractibility, and threshold scale).
Subgroups
We included information about the index child’s sex assigned at birth and whether their biological father was living with them at the 3-year assessment, and conducted subgroup analyses on female and male offspring separately and, in order to exclude stepfather confounds, on the subgroup of participants where the biological father was living with the family at the 3-year assessment.
Statistical analyses
We took the steps below for the data at 3 years, 6 months:
-
1. Participants with complete data on the paternal pre- and postnatal CCEI anxiety measures and on the RRPSPC scales at 3 years, 6 months were included in the analyses. We created four paternal anxiety status groups (measured using the CCEI): no anxiety at any time point, prenatal anxiety only (prenatal-only), postnatal anxiety only (postnatal-only), and anxiety at both prenatal and postnatal times (anxious-at-both-times). The groups were then compared on a range of sociodemographic variables that might have affected the associations between paternal anxiety and child outcomes.
-
2. Using binary logistic regression models, we conducted a series of planned contrasts to test differential effects of direct vs indirect exposure to paternal anxiety on children. The outcome in this first series of contrasts was high levels of emotional and behavioral symptoms in children at 3 years, 6 months measured using the RRPSPC. We contrasted risk in the three anxiety groups (prenatal-only, postnatal-only, and anxious-at-both-times) using the non-anxious group as the reference (baseline) group, and then undertook planned analyses directly comparing the anxious groups.
-
3. We repeated these analyses accounting for the potential effect effects of: child temperament, maternal only, and parental mental health (i.e., maternal anxiety and depression in the pre- and postnatal periods and paternal depression in the pre- and postnatal periods, history of severe depression and other psychiatric problems in parents), and for any other sociodemographic covariates that differed significantly between the anxious and non-anxious groups.
-
4. These analyses for RRPSPC scores were repeated for male and female offspring separately.
-
5. These analyses were repeated excluding those families where the biological father was no longer living with the family, to exclude stepfather confounds.
Steps 1 to 5 were repeated using psychiatric status of the children at 7 years, 7 months (DAWBA) as the outcome, to examine the persistence and developmental importance of any association. Only participants with complete data on the paternal pre- and postnatal CCEI anxiety measures and on DAWBA outcomes at 7 years, 7 months were included in the analyses. For consistency with the outcomes at 3 years, 6 months, we grouped the diagnostic outcomes in: any behavioral disorder (i.e., oppositional defiant, conduct, or attention deficit hyperactivity disorder), any emotional disorder (i.e., anxiety, obsessive compulsive, posttraumatic stress, depression disorder), and any disorder. We also reported on any anxiety disorder in offspring, to test whether there was an association between paternal and offspring anxiety specifically. In addition to the covariates mentioned above (3), we also accounted for the potential effect of paternal and maternal anxiety and depression at 73 months.
Finally, we undertook the analyses for outcomes at both 3 years, 6 months and 7 years, 7 months using continuous CCEI anxiety scores in fathers at prenatal and postnatal times as predictors, to address the potential artifacts that may derive from the use of cut-off scores.
Considering the theoretical and empirical interrelatedness of the variables examined, we chose not to apply corrections for multiple testing. Such corrections, particularly under assumptions of test independence, could increase the risk of Type II errors, thereby obscuring meaningful associations (Bender & Lange, Reference Bender and Lange2001; Ranganathan et al., Reference Ranganathan, Pramesh and Buyse2016). Instead, we emphasized the interpretation of results based on effect sizes and their associated confidence intervals, offering a more nuanced understanding of the data (Rothman, Reference Rothman1990).
Results
Outcomes at 3 years, 6 months
-
1. Data on paternal pre- and postnatal anxiety and on child outcomes at 3 years, 6 months were available for 6,404 participants. Fathers’ mean age was 31.20 years (SD = 5.55) and 98% identified their race as White. Of these, 303 (4.73%) were anxious only prenatally (prenatal-only group), 394 (6.15%) were anxious only postnatally (postnatal-only group), and 336 (5.25%) were anxious at both times (anxious-at-both-times group); 5,371 (83.87%) were anxious at neither time (non-anxious group). Table 1 provides the means and SD obtained by participants on the CCEI-anxiety pre- and postnatally. The four groups differed significantly in terms of: number of other children in the family, fathers’ marital status, fathers’ social class, and maternal and paternal mental health variables (see Table 1, where descriptive variables with missing values have been imputed. Table S1, available online, provides non-imputed data). The variables that were significantly different across the four groups were accounted for in the adjusted models.
-
2. The results of the unadjusted and adjusted models are presented in Table 2. For the total problems scale of the RRPSPC, children of anxious fathers had higher rates than children whose fathers had not been anxious perinatally; specifically, the non-anxious group differed significantly from the prenatal-only group (unadjOR = 1.82, 95%CI [1.28, 2.53], p = .001) and anxious-at-both-times group (unadjOR = 1.66, 95%CI [1.17, 2.30], p = .003). No significant differences emerged between the non-anxious and postnatal-only groups, nor when the anxiety groups were directly compared. The prenatal-only group was significantly more likely to have emotional problems than the non-anxious group (unadjOR = 2.37, 95%CI [1.63, 3.40], p < .001), but not behavioral problems (unadjOR = 1.40, 95%CI [0.99, 2.30], p = .049). For emotional problems, the prenatal-only and postnatal-only groups differed significantly from each other, with children with fathers anxious only postnatally half as likely to have emotional difficulties at 3 years, 6 months (unadjOR = 0.49, 95%CI [0.29, 0.83], p = .008).
-
3. When we controlled for the effects of sociodemographic variables (adjusted Model 1), child temperament (adjusted Model 2), maternal mental health (adjusted Model 3), and maternal and paternal mental health (adjusted Model 4), we found consistent, but attenuated, patterns of associations (see Table 2).
-
4. When we examined outcomes for male and female offspring separately, we found similar patterns of difference for the effects of paternal anxiety as to those we found for the entire sample (see Tables S2 and S3, available online). Specifically, when examining female offspring only, the prenatal-only and anxious-at-both-times groups had higher rates of high total problems scores than the non-anxious group, similar to the findings in the entire sample. Moreover, the prenatal-only group was significantly more likely to show emotional problems than all the other groups. Associations remained significant in some of the adjusted models. For male offspring, we found significantly increased rates of total problems in all three anxious groups, compared to the non-anxious group. Unlike in the analyses for the entire sample, compared to the non-anxious group, the postnatal-only group had higher rates of behavioral problems. In contrast, the prenatal-only and anxious-at-both-times groups had higher scores on the emotional problems scale (similar to the findings in the entire sample), suggesting that the direct exposure hypothesis may be relevant for behavioral problems in boys, but not for total and emotional problems. No significant differences emerged when the anxious groups were directly compared. For total problems, the associations remained significant in adjusted Model 1 and 2 when comparing the non-anxious group with the prenatal-only and postnatal-only groups, and in Model 1 when comparing the non-anxious group with the anxious-at-both-times group. No significant associations emerged in the adjusted models looking at behavioral outcomes, while for emotional problems the difference remained significant between the non-anxious and prenatal-only groups in Models 1, 2 and 3, and between the non-anxious and anxious-at-both-times groups in Model 1.
-
5. When we repeated the analyses only in those families where the biological father was still living with the family at the 3-year assessment, the patterns of significance remained consistent, with some small differences in the size and significance of the effects (see Table S4, available online).
Table 1. Descriptive characteristics of the sample used in the analyses looking at outcomes at 3 years, 6 months (n = 6,404; missing values have been imputed via multiple imputation)
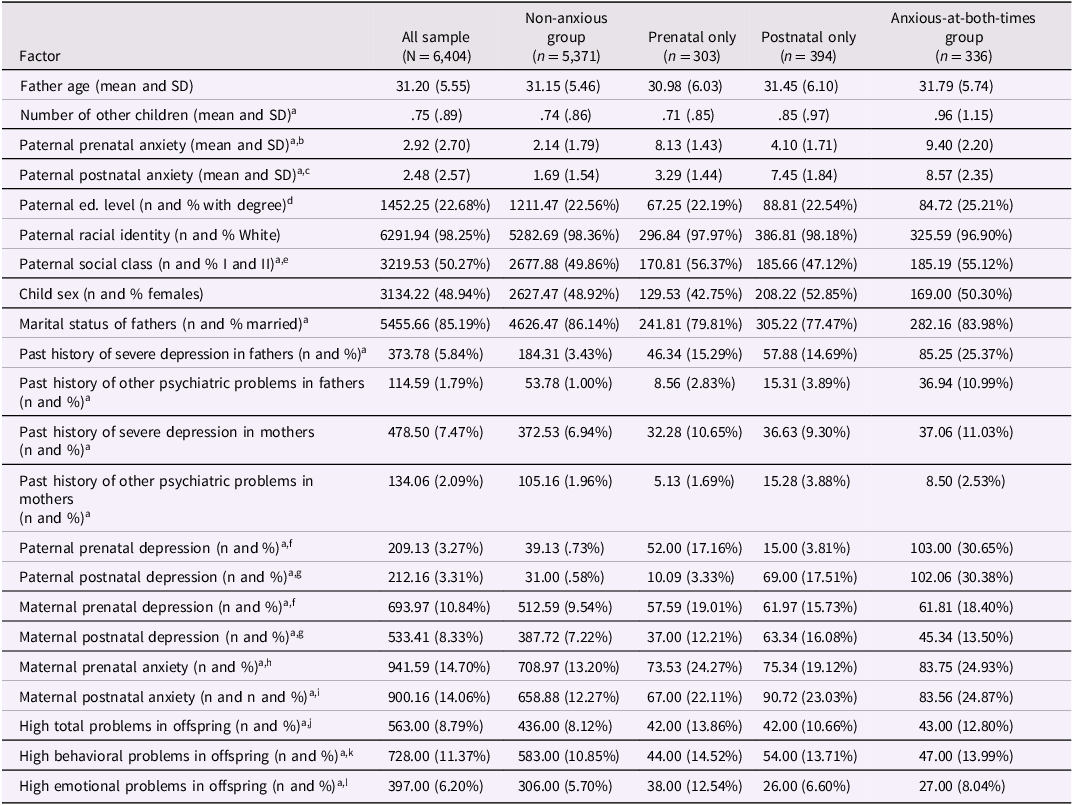
a Significant difference between the four groups (F value or Pearson’s Chi-squared test, p < .05).
b Continuous score in the Crown-Crisp Experiential Index at the 18-week gestation assessment.
c Continuous score in the Crown-Crisp Experiential Index at the 8-week postnatal assessment.
d Education level was analyzed in 5 categories of attainment, although only the percentage gaining a degree is presented here for ease of reading.
e I = professional occupations; II = managerial and technical occupations.
f Score>12 in the Edinburgh Postnatal Depression Scale at the 18-week gestation assessment.
g Score>12 in the Edinburgh Postnatal Depression Scale at the 8-week postnatal assessment.
h Score in the top 15% in the Crown-Crisp Experiential Index at the 18-week gestation assessment.
i Score in the top 15% in the Crown-Crisp Experiential Index at the 8-week postnatal assessment.
j Score in the top 10% in the total problems scale of the Revised Rutter Parent Scale for Preschool Children at 3 years, 6 months.
k Score in the top 10% in either the conduct or hyperactivity (or both) scales of the Revised Rutter Parent Scale for Preschool Children at 3 years, 6 months.
l Score in the top 10% in the emotional problems scale of the Revised Rutter Parent Scale for Preschool Children at 3 years, 6 months.
Table 2. Paternal anxiety and child high (top 10%) emotional and behavioral problems at 3 years, 6 months, unadjusted and adjusted models, with odds ratios and 95% confidence intervals
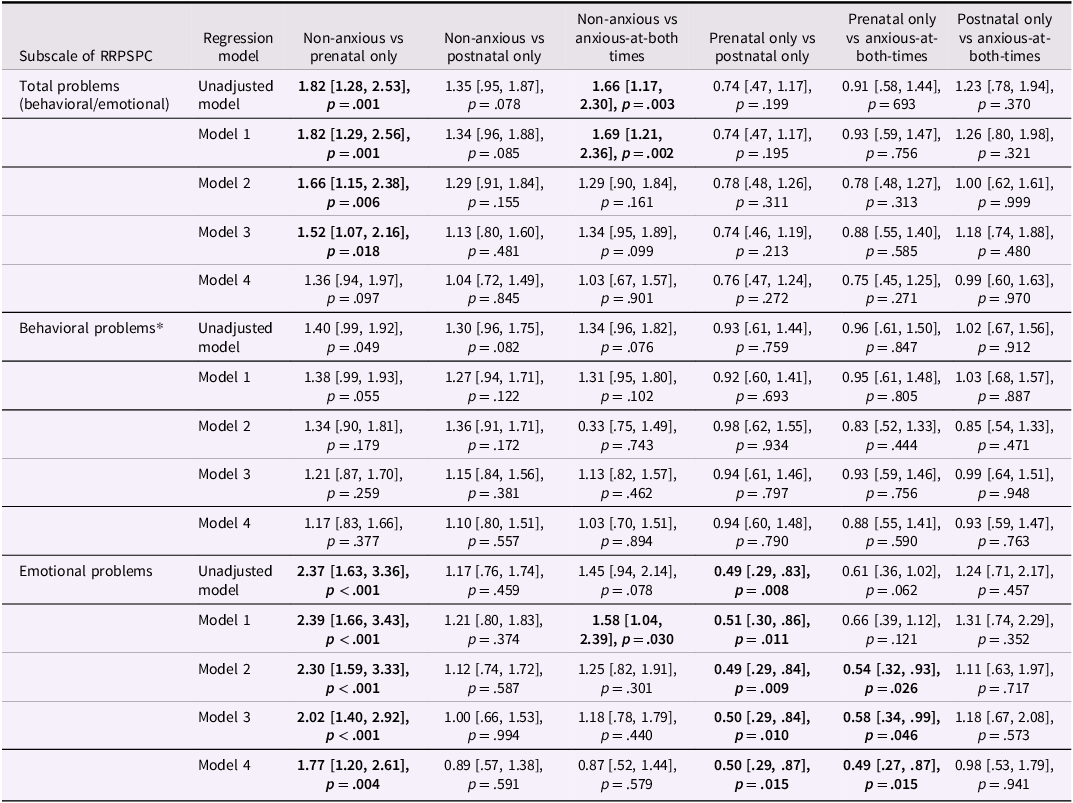
Note. The first group in each contrast was the reference group in the analyses. p-values have not been corrected for multiple-hypothesis testing.
Model 1 was adjusted for sociodemographic variables that were significantly different between the groups of comparison (i.e., number of other children, father social class, father marital status).
Model 2 was adjusted for child temperament (assessed via the Carey Infant Temperament Scale).
Model 3 was adjusted for maternal current and past mental health (maternal anxiety in the Crown-Crisp Experiential Index at 18-week prenatal and 8-week postnatal, maternal depression in the Edinburgh Postnatal Depression Scale at 18-week prenatal and 8-week postnatal, maternal history of severe depression and other psychiatric problems).
Model 4 was adjusted for maternal and paternal current and past mental health (maternal anxiety in the Crown-Crisp Experiential Index at 18-week prenatal and 8-week postnatal, maternal and paternal depression in the Edinburgh Postnatal Depression Scale at 18-week prenatal and 8-week postnatal, maternal and paternal history of severe depression and other psychiatric problems). In the adjusted models, missing values in covariates are imputed via multiple imputation. Significant results are in bold (p < .05). *Scale created by the authors, considering those who scored in the top 10% in the conduct and/or hyperactivity scales. RRPSPC = Revised Rutter Parent Scale for Preschool Children.
Outcomes at 7 years, 7 months
-
1. Data on paternal pre- and postnatal anxiety and on child outcomes at 7 years, 7 months were available for 5,426 participants. Fathers’ mean age was 31.47 years (SD = 5.46) and 98% identified as White. Detailed information on the sample at 7 years, 7 months is reported in Table 3 (with missing values imputed via multiple imputation; Table S5, available online, provides non-imputed data). The four groups differed significantly in: number of other children in the family, paternal marital status, and maternal and paternal mental health variables. These variables were accounted for in the adjusted models.
-
2. The results of the unadjusted and adjusted models are presented in Table 4. The anxious-at-both-times group, compared to the non-anxious group, had significantly higher rates of any psychiatric diagnosis (unadjOR = 2.35, 95%CI [1.60, 3.37], p < .001), any behavioral disorder diagnosis (unadjOR = 2.54, 95%CI [1.62, 3.84], p < .001), and any anxiety disorder diagnosis (unadjOR = 1.89, 95%CI [1.00, 3.40], p = .035). Rates of any psychiatric disorder and any behavioral disorder in the anxious-at-both-times group were also significantly higher than in the postnatal-only group. For behavioral disorders, rates were higher in the anxious-at-both-times than prenatal-only group.
-
3. When we controlled for the effects of sociodemographic variables (adjusted Model 1), child temperament (adjusted Model 2), maternal mental health (adjusted Model 3), and maternal and paternal mental health (adjusted Model 4), the patterns of the associations remained consistent, although were generally attenuated and some became statistically non-significant (see Table 4).
-
4. When we examined outcomes for male and female offspring separately, for males, similar patterns of difference to those at steps (2) and (3) emerged, but fewer significant associations were found for females (see Tables S6 and S7, available online). Specifically, in female offspring, the anxious-at-both-times group, compared to the non-anxious group, had higher rates of any psychiatric diagnosis and any anxiety disorder. For both outcomes, the associations remained significant in adjusted Model 1. No other significant differences emerged. In male offspring, similarly to the results for the entire sample, we found significantly higher rates of any psychiatric diagnosis and behavioral disorders in the anxious-at-both-times group, compared to the non-anxious group. These associations remained significant in all four adjusted models. Behavioral disorders were more common in the anxious-at-both-times, than in the prenatal-only group, and the associations remained significant in the adjusted Models 1, 3 and 4. Only for the adjusted Model 3, the anxious-at-both-times group had significantly higher rates of any diagnosis than postnatal-only group and, for the adjusted Models 3 and 4, the anxious-at-both-times group had significantly higher rates of behavioral disorders than postnatal-only group. No significant associations were found for emotional and anxiety disorders.
-
5. When we repeated the analyses in the subgroup of families where the biological father was still living with the family at the 3-year assessment, the patterns of significance remained consistent, with some small differences in the size and significance of the effects (see Table S8, available online).
Table 3. Descriptive characteristics of the sample used in the analyses looking at outcomes at 7 years, 7 months (n = 5,426; missing values have been imputed via multiple imputation)

a Significant difference between the four groups (F value or Pearson’s Chi-squared test, p < .05).
b Continuous score in the Crown-Crisp Experiential Index at the 18-week gestation assessment.
c Continuous score in the Crown-Crisp Experiential Index at the 8-week postnatal assessment.
d Education level was analyzed in 5 categories of attainment, although only the percentage gaining a degree is presented here for ease of reading.
e I = professional occupations; II = managerial and technical occupations.
f Score>12 in the Edinburgh Postnatal Depression Scale at the 18-week gestation assessment.
g Score>12 in the Edinburgh Postnatal Depression Scale at the 8-week postnatal assessment.
h Score>12 in the Edinburgh Postnatal Depression Scale at the 73-month assessment.
i Score in the top 15% in the Crown-Crisp Experiential Index at the 18-week gestation assessment.
j Score in the top 15% in the Crown-Crisp Experiential Index at the 8-week postnatal assessment.
k Score in the top 15% in the Crown-Crisp Experiential Index at the 73-month assessment.
l Assessed via the Development and Wellbeing Assessment - Parent Questionnaire at the assessment at 7 years, 7 months.
Table 4. Paternal anxiety and child psychiatric diagnoses at 7 years, 7 months, unadjusted and adjusted models, with odds ratios and 95% confidence intervals (n = 5,426)
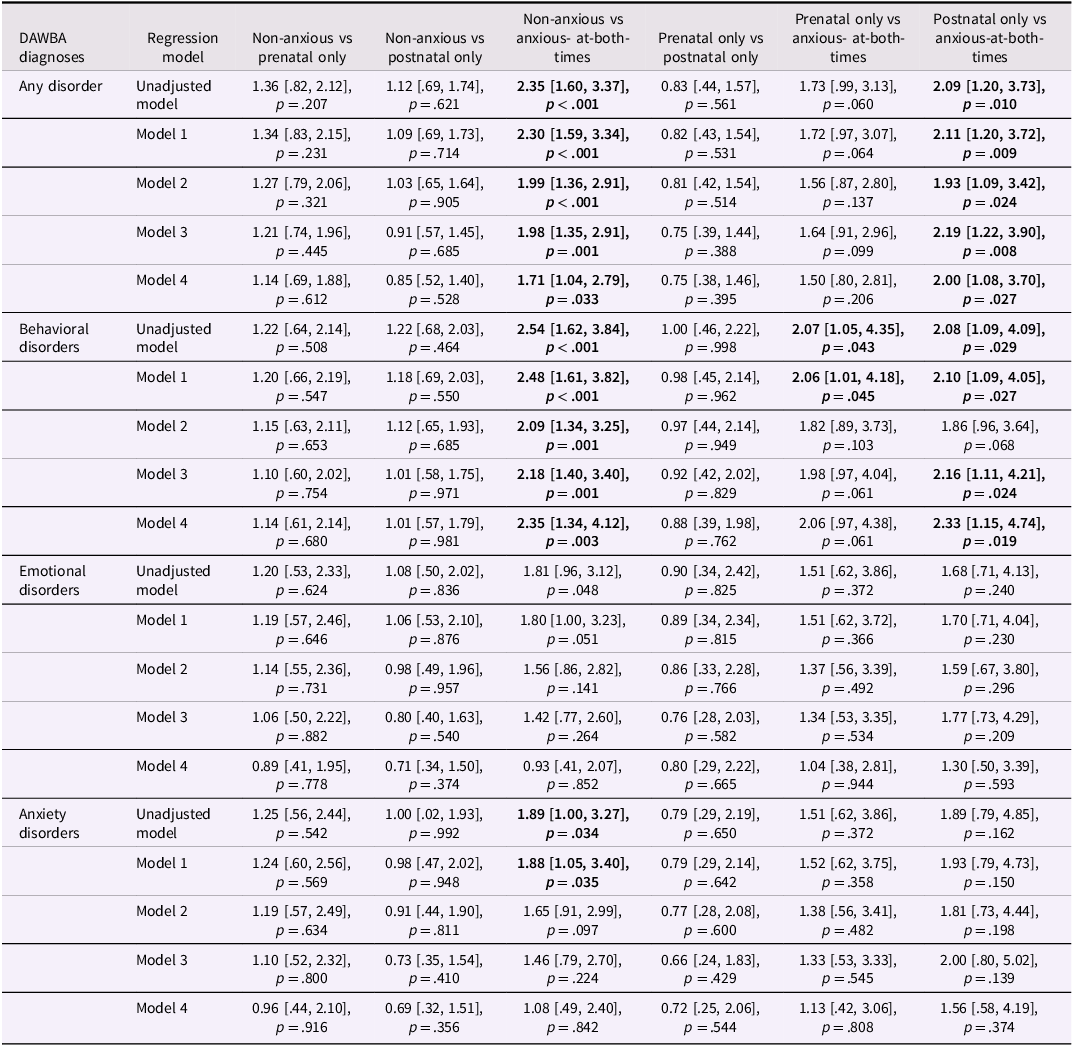
Note. The first group in each contrast was the reference group in the analyses. p-values have not been corrected for multiple-hypothesis testing.
Model 1 was adjusted for sociodemographic variables that were significantly different between the groups of comparison (i.e., number of other children, father marital status).
Model 2 was adjusted for child temperament (assessed via the Carey Infant Temperament Scale).
Model 3 was adjusted for maternal current and past mental health (maternal anxiety in the Crown-Crisp Experiential Index at 18-week prenatal, 8-week postnatal and 73 months, maternal depression in the Edinburgh Postnatal Depression Scale at 18-week prenatal, 8-week postnatal and 73 months, maternal history of severe depression and other psychiatric problems).
Model 4 was adjusted for maternal and paternal current and past mental health (maternal anxiety in the Crown-Crisp Experiential Index at 18-week prenatal, 8-week postnatal and 73 months, paternal anxiety in the Crown-Crisp Experiential Index at 73 months, maternal and paternal depression in the Edinburgh Postnatal Depression Scale at 18-week prenatal, 8-week postnatal and 73 months, maternal and paternal history of severe depression and other psychiatric problems). In the adjusted models, missing values in covariates are imputed via multiple imputation. Significant results are in bold (p < .05). DAWBA = Development and Wellbeing Assessment - Parent Questionnaire.
Continuous anxiety scores as predictors
When we conducted regression analyses using continuous anxiety scores in fathers at prenatal and postnatal time points as predictors, we found that higher paternal anxiety scores were significantly associated with an increased likelihood of adverse child outcomes at both 3 years, 6 months and 7 years, 7 months. Table S9 (available online) provides the unadjusted and adjusted ORs, showing that greater paternal anxiety both prenatally and postnatally was associated with higher odds of total, behavioral, emotional (and anxiety, for the assessment at 7 years, 7 months) problems in children.
Discussion
We believe that this is the first study to examine the role of different timings of paternal perinatal anxiety (prenatal-only, postnatal-only, and anxiety both pre- and postnatally) in relation to pre-schoolers’ or children’s mental health. Overall, our results indicate that paternal perinatal anxiety confers a risk for children’s subsequent mental health, in line with our hypothesis and with the emerging body of evidence highlighting the importance of paternal mental health for child development (Barker et al., Reference Barker, Iles and Ramchandani2017; Challacombe et al., Reference Challacombe, Pietikäinen, Kiviruusu, Saarenpää-Heikkilä, Paunio and Paavonen2023; Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008; Trepiak et al., Reference Trepiak, Trepiak, Guérin-Marion, Kristen and Deneault2022; Zecchinato et al., Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024).
The risk pattern at 3 years, 6 months was driven mainly by indirect (i.e., prenatal) exposure to paternal anxiety, in contrast with our hypothesis that direct exposure (i.e., postnatal anxiety only) is a greater risk than indirect exposure (Ramchandani et al., Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008). Specifically, compared to children with non-anxious fathers during the perinatal period, children with fathers anxious only prenatally were significantly more likely to present total and emotional difficulties. This suggests that, at 3 years, 6 months, paternal prenatal anxiety only, compared to no exposure to paternal anxiety, is sufficient and might be necessary to convey risk to children, while postnatal exposure alone, compared to no exposure, might be unnecessary and insufficient for children to manifest mental health difficulties at that age. These results could reflect the unmediated (e.g., genetic and epigenetic processes) and mediated (e.g., couple relationships, including foetal programing via an impact on maternal prenatal mental health; Van den Bergh et al., Reference Van den Bergh, Mulder, Mennes and Glover2005) pathways through which expectant fathers can shape child development during the prenatal period (Cardenas et al., Reference Cardenas, Morris, Marshall, Aviv, Martínez García, Sellery and Saxbe2022). Crucially, the magnitude of the effect sizes and pattern of associations remained consistent after accounting for sociodemographic variables, child temperament, maternal mental health (and paternal mental health, only for child emotional difficulties), highlighting the key relevance of paternal mental health, and anxiety specifically, independent from maternal mental health. The risk patterns remained generally consistent when male and female offspring were analyzed separately.
The analyses looking at the impact of timing of paternal anxiety on child psychiatric diagnoses at 7 years, 7 months resulted in different patterns compared to outcomes at 3 years, 6 months. Indeed, compared to children of non-anxious fathers, rates of offspring psychiatric disorder were only higher in children exposed both prenatally and postnatally. Specifically, children with fathers anxious at both times (pre- and postnatally) appeared to be at particular high risk of any psychiatric disorder and behavioral disorders, even after accounting for sociodemographic variables, child temperament, maternal mental health, and paternal mental health. This suggests that neither direct nor indirect exposure to paternal anxiety alone, compared to no exposure, is sufficient to convey risk through to 7 years, 7 months, but that cumulative exposure across both periods (i.e., direct and indirect risk exposure), compared to no exposure, may be necessary for mental health difficulties to manifest later in childhood. At 7 years, 7 months, offspring sex was important; for boys, the risk patterns were the same as those found for the entire sample, while smaller effects in magnitude were found for girls, for whom having a father anxious at both times resulted in significantly higher rates only of any anxiety disorders and any disorder, compared to those whose father was not anxious in the perinatal period. However, for female offspring the differences were not significant when adjusting for child temperament and parental mental health. These findings are consistent with studies showing that boys are more vulnerable than girls to the effects of their fathers’ mental illness, including depression (Ramchandani et al., Reference Ramchandani, Stein, Evans and O’Connor2005) and substance abuse (Loukas et al., Reference Loukas, Fitzgerald, Zucker and von Eye2001), and may be partly explained by the fact that fathers tend to spend relatively more time with their sons than with their daughters, possibly because fathers can identify better with a child of the same sex, or because of a belief that their knowledge and skills are more suited to raising a son than raising a daughter, as Lamb and Lewis (Reference Lamb and Lewis2010) theorized. However, societal changes are likely to influence these tendencies (Cabrera & Tamis-LeMonda, Reference Cabrera and Tamis-LeMonda2013; Feldman, Reference Feldman2023). The parent data analyzed in this study were collected in the 1990s, thus likely reflecting different societal and cultural views of fatherhood than 2020s expectations. Hence, to adequately capture the changing involvement of fathers in the family context and their influence on their children’s development, including the potential differential effects on male and female offspring, it is crucial to replicate these findings using more recent cohort data.
At both 3 years, 6 months and 7 years, 7 months, the findings remained generally consistent when we restricted the analyses to the subgroup of families where the biological father was still living with the family at the 3-year assessment.
While our findings do not support our initial hypothesis that direct exposure (i.e., postnatal anxiety only) poses a greater risk than indirect exposure (i.e., prenatal anxiety only) for adverse child outcomes, this may be due to the timing of the paternal postnatal anxiety assessment. Specifically, measuring anxiety at 8 weeks postnatally may be too early to capture its sustained impact on parenting behaviors and child development. This early postnatal period might not provide sufficient opportunity for the effects of paternal anxiety to manifest in ways that significantly influence child outcomes, as many interactions critical for emotional and behavioral development occur over a more prolonged timeframe (e.g., Moss et al., Reference Moss, Dobson and Mishra2020; Netsi et al., Reference Netsi, Pearson, Murray, Cooper, Craske and Stein2018). Future research would benefit from examining paternal anxiety over a longer duration postnatally to better capture its potential contributions to intergenerational risk transmission.
Strengths
The study has several strengths. It includes longitudinal data from a large, unselected population sample and long-term follow-ups, with assessments that spanned from before birth up to the age of seven years. We used well-validated measures to assess parental and offspring mental health, and reduced the risk of rater bias by using paternal self-reported measures of psychopathology and maternal and/or professional ratings of child difficulties. The unique nature of the rich longitudinal data enabled us to conduct a large prospective study, incorporating prenatal and postnatal exposure data to begin to disentangle direct vs indirect mechanisms of intergenerational risk transmission. Further, we controlled for the effect of maternal mental health, child temperament, and key sociodemographic variables in our analyses (Zecchinato et al., Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024). Notably, the significance of the findings after adjusting for covariates provides key evidence of the unique contribution of paternal anxiety in the perinatal period for subsequent adverse child mental health. Finally, we conducted sensitivity analyses to test any effect of child sex and of excluding families where the biological father was not present in the first three years of the child’s life.
Limitations
Sample size and statistical power
For the analyses looking at outcomes at both time points, the numbers in each of the risk groups are small in the context of the whole sample and compared to the non-anxious group. This is reasonable and reflects the natural distribution of the data within this large cohort; moreover, it is in line with Ramchandani et al. (Reference Ramchandani, O’Connor, Evans, Heron, Murray and Stein2008). However, these smaller subgroups may have limited our statistical power and the precision of our estimates, resulting in wider confidence intervals and potentially underestimating significant effects. Furthermore, the relatively small size of these risk groups may not fully capture the variability (e.g., demographic characteristics) within those populations, potentially restricting the generalisability of the findings to other populations. Hence, replication in other cohorts with larger subgroup sizes is needed to confirm these results.
Unmeasured confounders and genetic factors
Several factors, that were not accounted for in our study, are likely to play a role in the association between paternal anxiety and child outcomes and in the risk transmission, including assortative mating (Smolen et al., Reference Smolen, Jensen, Dyer, Pizzo, Tyryshkina, Banerjee, Rohan, Huber, El Khattabi and Prontera2023) and shared rater effects between mothers and fathers (Krasikova & LeBreton, Reference Krasikova and LeBreton2012); it is also possible that child’s characteristics influence paternal anxiety symptoms in the postnatal period, resulting in environmentally mediated transactional effects (Villarreal & Nelson, Reference Villarreal and Nelson2018). Additionally, we could not examine genetic confounds, and it is likely that shared genes, as well as other environmental stressors that have not been accounted for in our analyses, have played a role in the strength of the associations.
Potential collider bias
The possibility of collider effects should be considered when interpreting our results. Nevertheless, the models adjusted for maternal mental health and child characteristics showed patterns of significance and effect sizes consistent with the unadjusted models, suggesting that collider bias is unlikely to have substantially influenced the findings.
Use of anxiety cut-off scores
We were unable to use a diagnostic assessment of paternal anxiety, and set cut-off scores to identify anxious fathers. This means that a participant scoring just below the cut-off at one time point of interest and just above at the other may not have had significantly different psychopathological symptoms, but would be rated as non-anxious at one point and anxious at the other. We addressed this by repeating the analyses using continuous paternal anxiety scores. The consistency of the results suggests that the use of cut-offs did not create artefactual findings.
Timing of anxiety assessments
Our groups were created based on scores on a questionnaire repeated over a 6-month time gap. However, these time points are separated by a major life event (birth of a child and consequent transformation of the family system; Kluwer, Reference Kluwer2010), which justifies these relatively close in time assessments of anxiety.
Cohort attrition and missing data
As expected for large observational studies (Wright et al., Reference Wright, Heron, Kipping, Hickman, Campbell and Martin2021), we encountered the issue of cohort attrition, and the covariates presented missing data, which can introduce potential bias in the results and compromise the study inferences. However, we handled missing data using multiple imputation via the multivariate imputation by chained equations algorithm, which is a recommended technique to manage missingness in clinical research (White et al., Reference White, Royston and Wood2011). While this is a robust method, it has some limitations. It assumes that missingness can be adequately modeled using observed data, aligning with the missing at random framework (Van Buuren, Reference Van Buuren2018; White et al., Reference White, Royston and Wood2011); hence, if some data are missing not at random and cannot be explained by observed variables, the imputed values may be biased (Little & Rubin, Reference Little and Rubin2019; White et al., Reference White, Royston and Wood2011). Additionally, the default imputation methods may not fully capture complex relationships or interactions. Model diagnostics help ensure plausible imputations, but challenges in convergence and predictive power of the models remain, particularly in large datasets (Van Buuren, Reference Van Buuren2018; White et al., Reference White, Royston and Wood2011). Furthermore, imputations tailored to the ALSPAC cohort may not generalize to other datasets, and although the number of imputations followed standard guidelines (Rubin, Reference Rubin2004), additional imputations could further stabilize estimates (Little & Rubin, Reference Little and Rubin2019).
Generalisability of the findings
The sample comprises mostly White participants. The lack of representation of diverse racial and socioeconomic backgrounds in the current data limits generalisability to diverse populations and future research should aim to include more diverse samples (e.g., Wright et al., Reference Wright, Small, Raynor, Tuffnell, Bhopal, Cameron, Fairley, Lawlor, Parslow, Petherick, Pickett, Waiblinger and West2013).
Multiple testing considerations
Analyses were not corrected for multiple testing, and results should be interpreted with some caution, and in terms of both effect size estimates and associated confidence intervals.
Clinical implications and future directions
Our findings hold important clinical implications, highlighting the risk posed by paternal perinatal mental health, and anxiety specifically, to their offspring mental health, and adding to the evidence of the importance of identifying and treating fathers’ mental health difficulties pre- and postnatally, not only to improve their own quality of life, but also to implement successful preventive interventions or treatments for child mental health (Challacombe et al., Reference Challacombe, Pietikäinen, Kiviruusu, Saarenpää-Heikkilä, Paunio and Paavonen2023; Zecchinato et al., Reference Zecchinato, Ahmadzadeh, Kreppner and Lawrence2024). Indeed, this study underscores the potential value of involving fathers as active agents of change in clinical interventions aimed at addressing (or preventing) child mental ill-health, calling for better family-centered approaches to prevention and treatment that extend beyond the mother-child dyad (Dunn et al., Reference Dunn, Alvarez, Arbon, Bremner, Elsby-Pearson, Emsley, Jones, Lawrence, Lester, Morson, Simner, Thomson and Cartwright-Hatton2024; Peris et al., Reference Peris, Thamrin and Rozenman2021; Strawn & Peris, Reference Strawn and Peris2024).
However, this study does not allow for strong causal conclusions regarding the impact of paternal anxiety on offspring emotional and behavioral problems. More research is needed to clarify the father-specific contribution to child development and to identify the mechanisms underlying the association between paternal anxiety and child mental health outcomes. Future studies should prioritize experimental or quasi-experimental designs to establish the causal role of paternal anxiety symptoms and disorders in the intergenerational transmission of mental illness. These approaches are particularly important for informing the development of effective prevention and intervention strategies that target modifiable risk factors to reduce mental health risks among young children. Existing theory and research suggest that specific parenting behaviors, particularly parental modeling of anxious behaviors (Ginsburg et al., Reference Ginsburg, Drake, Tein, Teetsel and Riddle2015; de Rosnay et al., Reference de Rosnay, Cooper, Tsigaras and Murray2006) and overcontrolling parenting styles (Thirlwall & Creswell, Reference Thirlwall and Creswell2010), may act as key mechanisms in risk transmission. However, most empirical evidence to date has focused on maternal influences. Future research should investigate whether these same mechanisms apply to fathers or whether distinct paternal influences shape child emotional and behavioral outcomes. For instance, given differences in maternal and paternal caregiving styles (e.g., fathers displaying more stimulating and challenging parenting, and engaging in rough-and-tumble play, compared to the caring, nurturing and protective behaviors typically considered within the maternal domain; Lawrence et al., Reference Lawrence, Waite, Creswell, Compton, Villabø and Kristensen2019; Majdandžić et al., Reference Majdandžić, Möller, de Vente, Bögels and van den Boom2014; Paquette, Reference Paquette2004), it is possible that paternal anxiety manifests differently in parenting behaviors, with unique consequences for child development.
Furthermore, our findings suggest that the timing of paternal anxiety exposure may play an important role in shaping risk for later child outcomes. The distinct outcomes observed at 3 years, 6 months and 7 years, 7 months raise the possibility that different mechanisms operate at different developmental stages. At 3 years, 6 months, prenatal paternal anxiety appears to be a key risk factor, even in the absence of postnatal anxiety, potentially reflecting indirect influences via genetic or epigenetic pathways, maternal stress transmission, or family relationship dynamics (Cardenas et al., Reference Cardenas, Morris, Marshall, Aviv, Martínez García, Sellery and Saxbe2022; Ramchandani & Psychogiou, Reference Ramchandani and Psychogiou2009; Van den Bergh et al., Reference Van den Bergh, Mulder, Mennes and Glover2005), operating in a period of heightened vulnerability (Arango et al., Reference Arango, Díaz-Caneja, McGorry, Rapoport, Sommer, Vorstman, McDaid, Marín, Serrano-Drozdowskyj, Freedman and Carpenter2018; Michael et al., Reference Michael, Gard, Tillem, Hardi, Dunn, Smith, McLoyd, Brooks-Gunn, Mitchell, Monk and Hyde2024). By 7 years, 7 months, it is possible that cumulative exposure to paternal anxiety across both the prenatal and postnatal periods amplifies risk through sustained disruptions to family dynamics and father-child interactions, including lower sensitivity, increased withdrawal, or heightened parental control (Bronfenbrenner, Reference Bronfenbrenner1979; Dunn, Reference Dunn2004; Göksun et al., Reference Göksun, Aktan-Erciyes, Karadöller and Demir-Lira2024; Ramchandani & Psychogiou, Reference Ramchandani and Psychogiou2009), although it was not possible to test this hypothesis in the present study. This distinction aligns with theoretical models of early vulnerability versus cumulative risk exposure (Appleyard et al., Reference Burt, Van Dulmen, Carlivati, Egeland, Sroufe, Forman, Appleyard and Carlson2005; Evans et al., Reference Evans, Li and Whipple2013), highlighting the need for research that tracks paternal anxiety and child development across multiple time points. Examining offspring mental health trajectories in relation to the persistence, fluctuation, or resolution of paternal anxiety over time could provide insights into critical periods of risk exposure and potential intervention windows.
By addressing these gaps, future research can refine intervention strategies aimed at reducing intergenerational risk transmission. Specifically, studies should explore whether prenatal interventions focused on expectant fathers’ mental health can mitigate early risk pathways, while postnatal interventions targeting father-child interactions and parenting behaviors may be more effective for reducing later mental health difficulties in school-aged children (rather than pre-school-aged children). Identifying these developmental windows for intervention will be essential for designing tailored, evidence-based approaches to supporting paternal mental health and improving child outcomes.
Conclusion
This study built on the existing research focused on fathers’ contribution to child development by testing the role of the timing of paternal perinatal anxiety exposure in children’s subsequent psychological functioning. We took advantage of rich longitudinal data on paternal anxiety and offspring emotional and behavioral outcomes collected in a large UK-based birth cohort study (ALSPAC) and conducted a prospective study adopting a prenatal vs postnatal design. Although our design does not allow us to draw strong causal conclusions, we found that children whose fathers are anxious in the perinatal period, compared to children of non-anxious fathers, are more likely to present mental health difficulties at 3 years, 6 months and 7 years, 7 months. This demonstrates that paternal perinatal anxiety is an important risk factor for adverse child outcomes, even after accounting for maternal mental health, child temperament, and key sociodemographic factors, and should not be overlooked in research and clinical practice. However, further research is needed i) to identify the precise mechanisms by which indirect and direct risk transmission occurs so as ii) to enable the development of preventative strategies and interventions to reduce risks for young children.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579425000343.
Data availability
Access to ALSPAC data is through a system of managed open access (http://www.bristol.ac.uk/alspac/researchers/access/).
Acknowledgements
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses.
Author contribution
P.J.L., J.M.K. and F.Z. conceptualized the research question and developed the analysis plan. F.Z. analyzed the data and drafted the manuscript. P.J.L. and J.M.K. reviewed results, and provided guidance on methodology. All authors reviewed and contributed to the manuscript and approved the final version of the manuscript.
Funding statement
The UK Medical Research Council and Wellcome (Grant ref: 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors and Peter J. Lawrence and Francesca Zecchinato will serve as guarantors for the contents of this paper. A comprehensive list of grants funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf). This research was specifically funded the Economic and Social Research Council South Coast Doctoral Training Partnership Grant Number ES/P000673/1.
Competing interests
None.
Analytic code availability
Our protocol and analytic code are openly accessible via the Open Science Framework (https://doi.org/10.17605/OSF.IO/DJUKV).








