Recovery-oriented interventions are receiving increasing attention globally. 1 Peer support is an established recovery-oriented intervention in which a person in recovery from a mental health condition offers support to others living with mental health conditions. Reference Davidson, Chinman, Sells and Rowe2 Peer support workers (PSWs) support their own recovery and that of others by drawing on their lived experience, employing positive self-disclosure, expanding social networks, and promoting hope, empowerment and self-efficacy. Reference Fuhr, Salisbury, De Silva, Atif, van Ginneken and Rahman3,Reference Corrigan, Larson, Smelson and Andra4 The evidence base on peer support for adults with mental ill health is maturing. Reference Johnson, Lamb, Marston, Osborn, Mason and Henderson5,Reference Gillard, Bremner, Patel, Goldsmith, Marks and Foster6 Early research showed that PSWs were able to achieve similar or even slightly better outcomes than professionally trained staff. Reference Fuhr, Salisbury, De Silva, Atif, van Ginneken and Rahman3,Reference Pitt, Lowe, Hill, Prictor, Hetrick and Ryan7 More recent reviews suggested there may be a positive impact on a range of psychosocial and functional outcomes, especially recovery-related outcomes (e.g. social inclusion and empowerment), but that this impact may be rather limited for clinical outcomes such as symptomatology. Reference White, Foster, Marks, Morshead, Goldsmith and Barlow8–Reference Yim, Chieng, Tang, Tan, Kwok and Tan13 The evaluation of peer support is increasingly moving beyond a focus on individual clinical outcomes towards more social and recovery-oriented outcomes, such as social inclusion, which is a key outcome in global mental health. Reference Baumgartner and Burns14 There is broad consensus that there are significant gaps in the evidence base on peer support in low- and middle-income countries (LMICs) and in non-Anglophone high-income countries (HICs), including measuring recovery-oriented outcomes. Reference Vally and Abrahams15 Although peer support is spreading rapidly all over the world, Reference Stratford, Halpin, Phillips, Skerritt, Beales and Cheng16 cross-cultural key issues remain, including role expectations, initial training, type of contact, role extension, workplace support for PSWs, recruitment and supervision. Reference Vally and Abrahams15,Reference Charles, Thompson, Nixdorf, Shamba, Kalha and Moran17 We need a better understanding of how peer support needs to be adapted for cultural reasons, Reference Charles, Thompson, Nixdorf, Shamba, Kalha and Moran17 and how best to support implementation, Reference Ibrahim, Thompson, Nixdorf, Kalha, Mpango and Moran18 to ensure that peer support is provided in accordance with the fundamental values of civil rights and social justice and at the same time takes into account differing worldviews. Reference Stratford, Halpin, Phillips, Skerritt, Beales and Cheng16 There is a need for large-scale international trials across diverse cultural and resource settings, emphasising user-centred outcomes, to further strengthen the evidence base for peer support for people with mental ill health.
This paper presents findings from a multi-country randomised controlled trial that tested the effectiveness of a manualised peer support intervention for people with severe mental health conditions in a range of high-, middle- and low-income countries. A priori hypotheses were that 8 months after baseline, participants who received the intervention, as compared with participants allocated to the wait-list control group, would show: (a) improved social inclusion (primary outcome); and (b) improved empowerment, hope, recovery, health and social functioning (secondary outcomes).
Method
UPSIDES-RCT is a pragmatic parallel-group multicentre randomised controlled trial with a wait-list control group and four measurement points: baseline (t 0), 4 months (t 1), 8 months (t 2, primary clinical endpoint) and 12 months (t 3). Participants allocated to the intervention group were offered UPSIDES peer support after having been informed about allocation. The study was carried out at six study sites: (a) Ulm, Germany: rural catchment area of Ulm University’s Clinic for Psychiatry and Psychotherapy II; (b) Hamburg, Germany: University Medical Centre Hamburg-Eppendorf and community services all over Hamburg; (c) Butabika, Uganda: Butabika National Referral Hospital which is the main psychiatric referral hospital situated in the capital city Kampala; (d) Dar es Salaam, Tanzania: Department of Psychiatry and Mental Health at Muhimbili National Hospital; (e) Be’er Sheva, Israel: two community rehabilitation organisations (‘Kidum Proyektim Shikumiim’ and ‘Enosh’) which provide services across the country, supported by the Ministry of Health; (f) Pune, India: Hospital for Mental Health in Ahmedabad, Gujarat, which is a public mental health facility and Gujarat’s largest psychiatric speciality hospital.
Written informed consent was obtained from study participants. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. All procedures involving human participants and/or patients were approved by ethics boards at all study sites.
The trial has been prospectively registered (ISRCTN registry, ISRCTN26008944). See the supplementary material available at https://doi.org/10.1192/bjp.2025.10299 for further information about procedures, including details of ethics review boards, data collection, responses to challenges arising from the COVID-19 pandemic and assessment of adverse events. Reporting of the results follows the Consolidated Standards of Reporting Trials (CONSORT) statement. Reference Zwarenstein, Treweek, Gagnier, Altman, Tunis and Haynes19
Participants
To be eligible for inclusion, potential participants had to be aged 18 to 60 years at intake and have a severe mental health condition, defined as a long-standing mental health condition of any kind which has resulted in substantial functional impairment limiting major life activities (Threshold Assessment Grid Reference Rosen, Strathdee, Slade and Powell20 score ≥5 points and illness duration ≥2 years). Diagnoses could be established by case notes, staff communication or self-report. Further inclusion criteria were sufficient command of the dominant language at each study site and ability to provide informed consent. Exclusion criteria were: a main diagnosis of learning disability, dementia, substance use disorder or organic brain disorder; and cognitive impairment severe enough to make it impossible to give informed consent or complete study measures. Potential participants were approached using several means, including through in-patient, out-patient and community mental health services, patient and carer organisations, local newspapers, social media, community leaders and word of mouth.
Intervention
UPSIDES peer support is a formal service delivered by a trained person with lived experience of recovery from a mental health condition to another person with a serious mental health condition. The intervention has been designed to adhere to the core principles of peer support (e.g. mutual, reciprocal, non-directive, strength-based, and recovery- and community-oriented), as specified in the UPSIDES conceptual framework (see the training manual Reference Mahlke, Nixdorf, Repper, Charles, Slade and Ryan21 for details), while allowing enough flexibility to adapt to each site’s unique social, cultural and organisational contexts. It has been developed by all UPSIDES partners through literature review and adaptation of existing programmatic materials. Reference Hall, Baillie, Basangwa, Atukunda, White, Jain, Orr and Read22–Reference Moran27 The primary training concept was delivered in a train-the-trainer-workshop with PSWs from all sites, further adapted through focus groups reflecting on the usability for the respective settings, Reference Nixdorf, Kotera, Baillie, Garber Epstein, Hall and Hiltensperger28 and piloted at all study sites. Reference Nixdorf, Nugent, Aslam, Barber, Charles and Gai Meir29 The UPSIDES peer support training consists of 12 core modules (e.g. PSW role, recovery, network, trialogue, communication), with additional modules addressing site-specific topics (see the training manual Reference Mahlke, Nixdorf, Repper, Charles, Slade and Ryan21 for details). The implementation manual Reference Nakku, Ryan, Aslam, Baillie, Ben-Dor and Charles30 sets out further guidance, including essentials for UPSIDES sites as well as additional recommendations based on programmatic experience and guidance, Reference Repper, Aldridge, Gilfoyle, Gillard, Perkins and Rennison31 across six key areas of implementation (e.g. PSW recruitment, capacity-building, quality assurance).
UPSIDES PSWs were adults (aged 18 to 60 years) who were in recovery and had not been admitted to hospital for at least 3 months before training. UPSIDES PSWs were compensated for their work, with financial arrangements differing among study sites (paid positions or pay-per-day), and received support in different ways (regular supervision and various activities to promote well-being). For instance, at Butabika, PSWs received individual as well as group supervision, to review the recovery skills they were using to support their clients and to provide additional mentoring based on the training manual. Supervisors also provided medical review and care, including medicine refills and psychological support when needed, without the PSW having to queue up in the clinic. In addition, team building events with cake-cutting were organised, as well as lunches with the research teams, and branded T-shirts were provided to make PSWs feel they belonged. This energised the PSWs. See the implementation manual Reference Nakku, Ryan, Aslam, Baillie, Ben-Dor and Charles30 for details.
UPSIDES peer support can be delivered in either an individual or group format, or as a combination of the two. It was delivered in a one-to-one format at five study sites (Ulm, Hamburg, Butabika, Dar es Salaam and Pune), of which two (Hamburg and Dar es Salaam) also offered additional groups, and in a small group format (‘Chevruta’) in Be’er Sheva, as this was found to be a better fit for the organisational structure of the existing community mental health services. Reference Goldfarb, Grayzman, Meir, Grundman, Rabinian and Lachman32 The intended duration of UPSIDES peer support was up to 6 months, with a minimum of three contacts. Weekly or fortnightly meetings were recommended, but the frequency could vary depending on the needs of patients, PSWs and study sites. Participants allocated to the intervention group were offered UPSIDES peer support immediately after allocation. Participants allocated to the control group were put on a waiting list and were offered the intervention after follow-up of the intervention group had been completed. All participants received treatment as usual; this consisted of a mix of in-patient, out-patient and community services, with substantial variation across sites (see the supplementary material for details).
Outcomes
The primary outcome was measured using the Social Inclusion Scale (SIS Reference Charles, Korde, Newby, Grayzman, Hiltensperger and Mahlke33 ), which has 16 items to be answered on a four-point Likert scale with responses ranging from ‘not at all’ to ‘yes definitely’. After reverse-scoring three negatively worded items, the total SIS score was calculated as the sum over the 16 items, ranging from 16 (low social inclusion) to 64. The SIS has three subscales: social isolation, referring to the amount of contact an individual has with people and society (four items); social relations, referring to relationships between people (nine items); and social acceptance, referring to a person’s sense of being accepted within their social contexts (five items). Secondary outcomes measures were as follows. (a) Empowerment, measured with the Empowerment Scale, Reference Rogers, Ralph and Salzer34 a 28-item instrument designed to tap into subjective feelings of empowerment on a four-point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’. After reverse-scoring of nine negatively framed items, the total score is the sum of all items, ranging from 28 (low empowerment) to 112. (b) Hope, measured with the HOPE scale, Reference Snyder, Harris, Anderson, Holleran, Irving and Sigmon35 which consists of 12 items rated on an eight-point Likert scale ranging from ‘definitely true’ to ‘definitely false’. The total score is the sum of eight items (excluding four ‘filler’ items), ranging from 8 (low hope) to 64. (c) Recovery, measured with the Stages of Recovery Instrument (STORI-30 Reference Andresen, Caputi and Oades36 ), which consists of 30 items representing five stages of recovery 5, growth), rated on a six-point Likert scale ranging from ‘not at all true now’ to ‘completely true now’. The stage subscale with the highest total is the person’s stage of recovery. Where the highest score was equal for two stages, the higher stage was used. (d) Health and social functioning, measured with the Health of the Nations Outcome Scales (HoNOS Reference Wing, Beevor, Curtis, Park, Hadden and Burns37 ), which consists of 12 items rated on a five-point Likert scale ranging from ‘no problem’ to ‘very severe problem’. The total score is the sum of all items, ranging from 0 (low impairment) to 48.
All outcome measures except for the HoNOS were collected using patient-reported measures. HoNOS was researcher-rated, applied by study workers who had received instrument training. All total scores were prorated in cases of missing values for fewer than 20% of the single items making up the score. Established state-of-the-art translation guidelines Reference Wild, Eremenco, Mear, Martin, Houchin and Gawlicki38 were followed to translate and locally validate the standardised outcome measures (including administration instructions) used, with special attention paid to psychometric evaluation of the primary outcome. Reference Charles, Korde, Newby, Grayzman, Hiltensperger and Mahlke33
Sample size
Sample size calculation was performed for testing whether the primary outcome (social inclusion at t 2) was affected by allocation. For six study sites, three time points and an estimated panel attrition of 10% at each time point, N = 558 participants (N = 93 per site) were needed to detect a small effect size (0.25 s.d. units) with a power of 0.80 at a two-tailed significance level of 0.05. Sample size calculation was done using RMASS for a three-level mixed-effects linear regression model, assuming a linear effect over time; compound symmetry for error variance covariance; person-level covariance values (int, cov, slope) of 0.300, 0.150 and 0.100, respectively; and centre-level covariance values of 0.050, 0.025 and 0.020 respectively.
Randomisation
Participants were randomly assigned to either the control or the intervention group with one-to-one allocation using a computer-generated randomisation schedule, stratified by site using permuted blocks of random sizes. To ensure concealment, block sizes were not disclosed, and the randomisation code was not released until the participant had been recruited into the trial and baseline assessments had been completed. The sequence was generated by an independent service (Institute for Epidemiology and Medical Biometry, Ulm University, Germany) to keep the data management team and study statistician blind to the study allocation for as long as the data bank was open. Trained research workers enrolled participants and informed them about their allocated trial group. Owing to the nature of the intervention, participants, PSWs and research workers collecting data could not be blinded. Researchers who analysed study data were not involved in data collection and were blinded until the data collection and data checks had been completed.
Statistical analysis
Descriptive reports include absolute and relative frequencies for categorical variables and means and standard deviations for continuous variables. Differences in baseline characteristics by site were tested using chi-squared tests for categorical variables and t-tests or analyses of variance for continuous variables. Primary and secondary outcomes from measurement points t 0, t 1 and t 2 were subjected to hierarchical linear models with the time variable t (actual time in months, including delays due to pausing for COVID-19 lockdowns), allowing inclusion of cases with incomplete (unbalanced) data across panels. Reference Raudenbush and Bryk39 Random effects were observations within participants over time, and fixed effects were effects of time and allocation on the outcome measure, controlled by study site (which was used as stratification variable in randomisation; see above). Differences in slope, i.e. in monthly change rate of the given outcome due to allocation, constituted the criterion for effect. Analyses followed the intention-to-treat principle, i.e., they were performed without knowledge of any participants allocated to the intervention group missing (parts of) the intervention, and all available data were used in the data analysis. The per-protocol analysis included participants who had received at least three peer support sessions. Numbers in Tables 1 and S1 were calculated using R (version 4.3.1 for Windows). S-Plus (version 8.2 for Windows; TIBCO Software Inc., Palo Alto, USA; https://docs.tibco.com/products/tibco-spotfire-s-8-2-0.) was used for the effectiveness analyses. All other analyses used SPSS (version 28 for Windows).
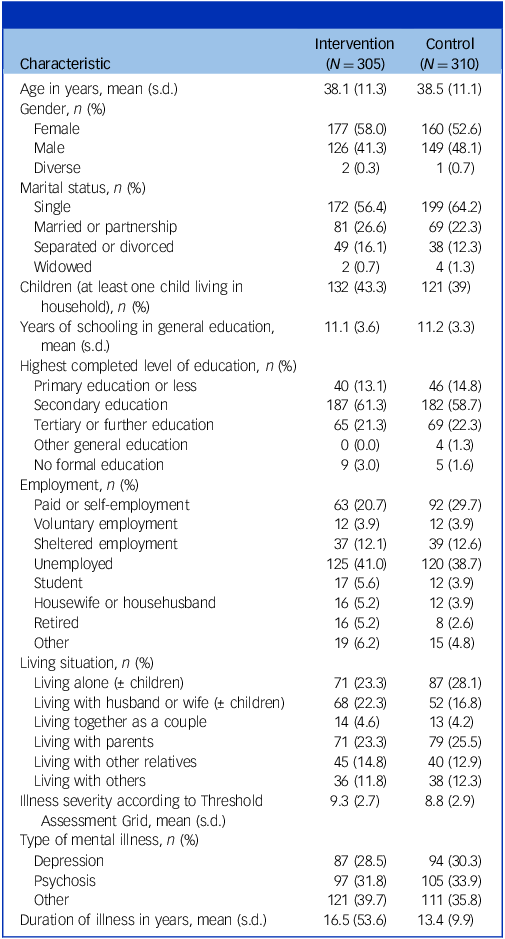
Table 1 Baseline characteristics
Results
Study participants
A total of 615 participants were recruited between 1 January 2020 and 12 August 2021, of whom 305 were randomised to the intervention group and 310 to the control group, respectively. Figure 1 shows the flow of participants through the different stages of the trial. Baseline characteristics of the 615 participants are shown in Table 1. On average, participants were in their late 30s, more than half identified as women, most were single, and most had completed secondary education. Many participants were unemployed and living alone or with their parents. Diagnoses of mental illness were a mix of depression, psychosis and other conditions, and illness duration was approximately 15 years. Key baseline characteristics varied substantially by study site (supplementary Table 1).
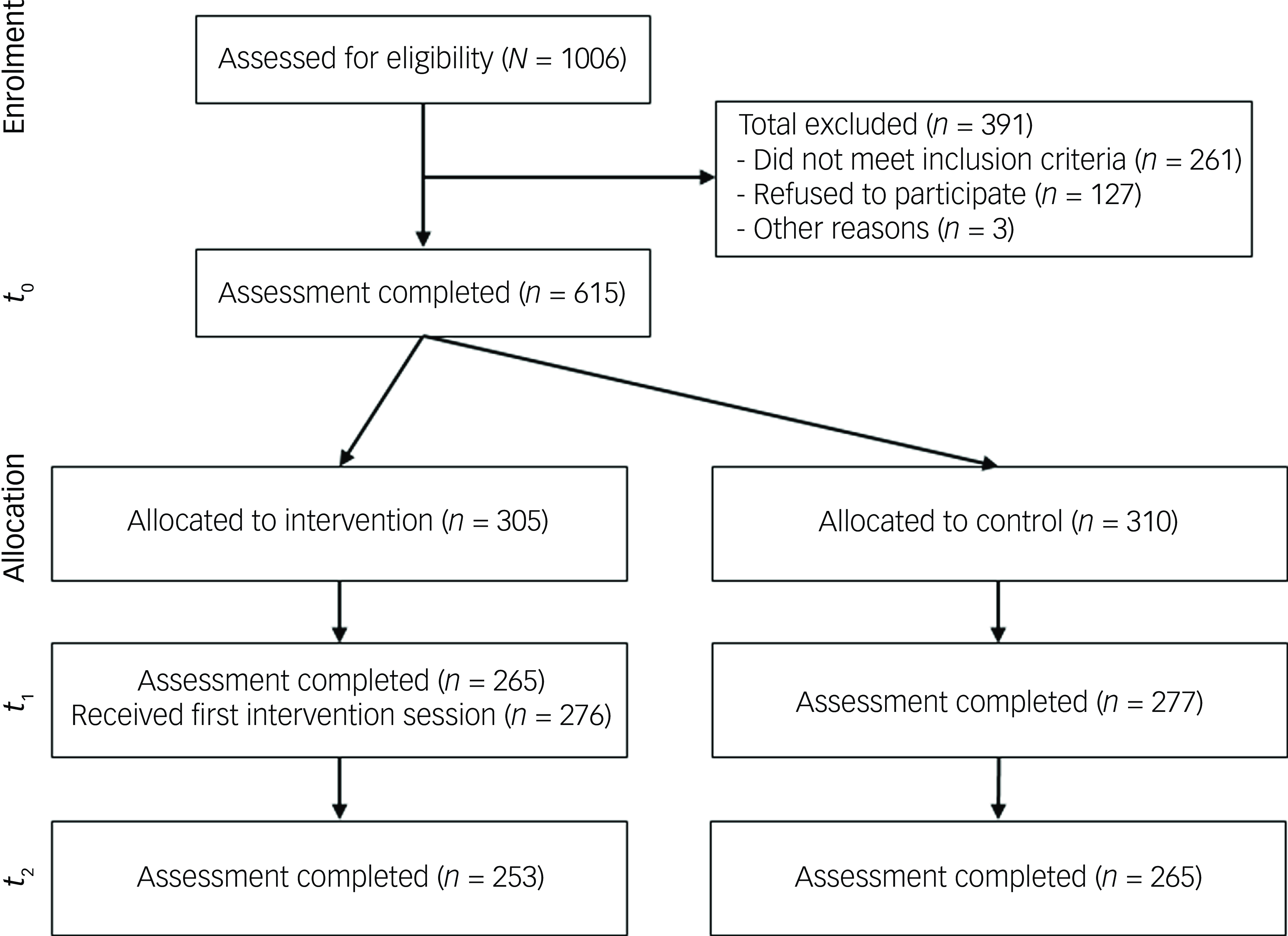
Fig. 1 Participant flow (CONSORT diagram).
Uptake of the intervention
Details about uptake of the intervention are shown in Table 2. A total of 276 (90.4%) participants allocated to the intervention group received at least one session of UPSIDES peer support over the course of the intervention period, which lasted approximately 4 months. On average, participants received seven sessions, which often lasted 30 min or more. The vast majority of sessions were held in a one-to-one (individual) format. Some sessions were held in a group format, with a mean number of 5.11 (s.d. = 2.72) participants. In Ulm, Butabika and Pune, all sessions were held in a one-to-one format, whereas in Be’er Sheva, all sessions were held in group format. In Hamburg and Dar es Salaam, six and 26 participants, respectively, received both one-to-one and group peer support; the rest received one-to-one support. Across all sites, a total of 1559 individual and group sessions were provided. Across all sessions, 87.2% were held in person (during a home visit, at the institution or in a public meeting place), and 11.7% of sessions were held remotely (via phone call or video call). Thirty-two participants dropped out without having participated in any intervention session.
Table 2 Uptake of the intervention
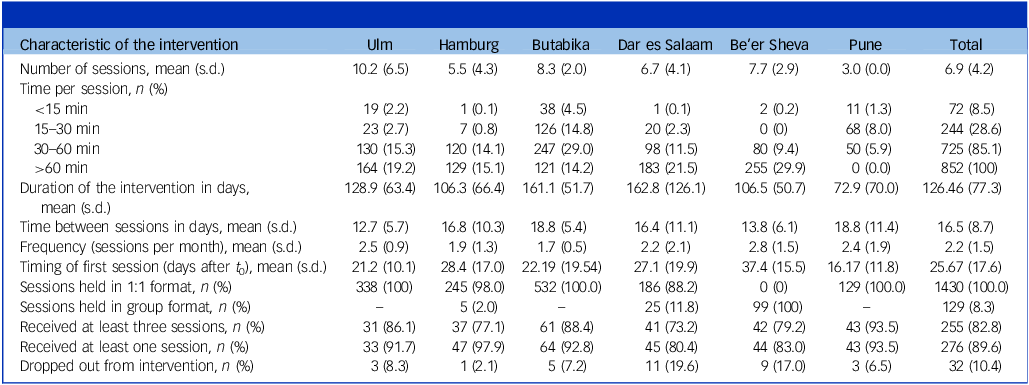
We report the following protocol deviations: ten participants (3.62%) received sessions during official government lockdowns, 99 participants (35.87%) received their first session more than 31 days after t 0 assessment, 46 participants (16.67%) received the intervention for longer than 6 months and 21 participants (7.61%) received fewer than three sessions. Finally, at one site, five group sessions were mistakenly held with a mix of participants from the intervention and the control group.
Effectiveness
As shown in Table 3, the intention-to-treat analysis found significant effects of the intervention for two of the three SIS (primary outcome) subscales: social isolation and social acceptance. Among secondary outcomes, empowerment and hope significantly improved, whereas there were no significant effects for STORI or HoNOS. After exclusion of the 50 participants in the intervention group who had received fewer than three peer support sessions, the per-protocol analysis showed that the improvement in SIS total score was significantly greater in the intervention group, and the magnitude of all other effects shown in the intention-to-treat analysis increased. Detailed statistics for all outcome analyses are shown in supplementary Tables 2 and 3.
Table 3 Effectiveness of UPSIDES peer support
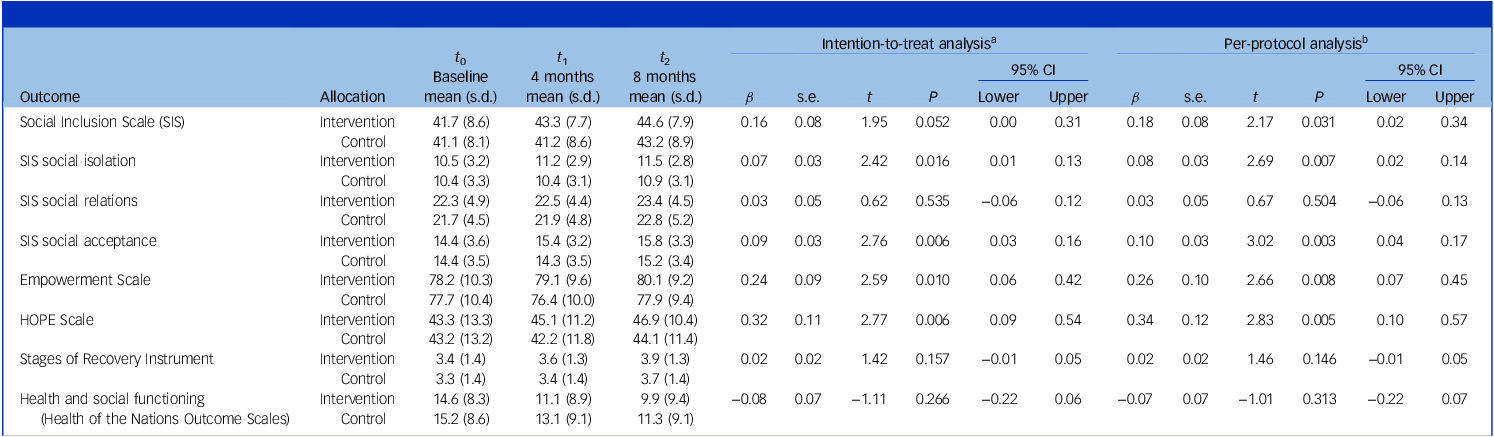
In the intention-to-treat analysis, the number of observations ranged from 1651 (HOPE scale) to 1661 (SIS social isolation), for 613 (Empowerment Scale), 614 (SIS and its subscales) or 615 (all other measures) participants.
In the per-protocol analysis, the number of observations ranged from 1561 (HOPE scale) to 1571 (SIS social isolation) for 563 (Empowerment Scale), 564 (SIS and its subscales) or 565 (all other measures) participants.
We report a total of 52 serious adverse events for 40 participants (26 women, 14 men; 21 in the intervention group and 17 in the control group; two before randomisation). The events reported were death (six events), life-threatening occurrences (two events) and admission to hospital (44 events). None of the reported serious adverse events was related to study participation or receiving the intervention.
Discussion
Our key finding was that UPSIDES peer support improved social inclusion, hope and empowerment, when tested through a multisite randomised controlled trial including samples from high-, middle- and low-income countries. This study was novel not only in its selection of diverse study sites (which included non-Anglophone HICs in Europe and the Middle East, as well as LMICs in South Asia and sub-Saharan Africa) but also in its investigation of social inclusion and other outcomes of particular relevance to the field of global mental health as it seeks to move past its traditional biomedical focus. Reference Baumgartner and Burns14 The effect on overall social inclusion as the primary outcome did not quite reach statistical significance in the intention-to-treat analysis, which included non-engaging participants. On the other hand, effects were stable for two of the three subscales of the social inclusion measure (social isolation and social acceptance) in both intention-to-treat and per-protocol analyses, whereas one subscale (social relations) failed to show an effect in either. Social relations is the most behavioural subscale, with items including going to new places, doing cultural activities and walking around the neighbourhood. As much of the trial took place during the COVID-19 pandemic, it seems reasonable to assume that these specific aspects of social inclusion were less amenable to improvement owing to lockdown restrictions and public health advice to reduce social mixing. By contrast, it is striking that the social isolation subscale (with items related to feeling alone and accepted) and the social acceptance subscale (with items related to expression of beliefs and acceptance from friends and neighbours) both showed significant improvements, despite pandemic-related restrictions. We may cautiously assume that without an epidemic requiring social isolation, effects would have been found across all aspects of social inclusion. However, also the opposite argument may be considered: that owing to COVID-19 restrictions, additional efforts were made by research staff to include and keep study participants, which may have made them feel particularly appreciated, and that effects may have been smaller without such restrictions.
Effects of the intervention were substantial for empowerment and especially for hope, but no improvements were found for health or social functioning. This reinforces previous findings that peer support is especially beneficial for recovery-related and patient-rated outcomes but has little effect on clinical and staff-rated outcomes. Reference White, Foster, Marks, Morshead, Goldsmith and Barlow8–Reference Høgh Egmose, Heinsvig Poulsen, Hjorthøj, Skriver Mundy, Hellström and Nørgaard Nielsen11 Moreover, although there was a visible effect for recovery measured via STORI-30, this failed to reach statistical significance. It could be that the observation period of 8 months was too short to pick up changes in stage of recovery, which might take longer to evolve. Reference Linde, Schmid, Ruud, Skar-Fröding and Biringer40 Recovery is also notoriously difficult to measure, and current measurement tools are rooted in mainly Western individualistic models, which have been criticised for neglecting collectivistic values and other priorities. Reference Tse and Ng41 For example, the Chinese version of the STORI-30 did not replicate the five-factor structure yielded by the original Australian samples. Reference Lau, Law and Ng42 Although stage 1 was replicated, the items in the other four stages in the original version were merged into two stages in the Chinese version. This suggests that the foundational concepts of the STORI-30 are not culturally adapted. For example, concepts such as ‘separation of self from illness’ (in stage 2), ‘take control of their life’ in (stage 4) and ‘meaningful future’ (in stage 5) may have different meanings across cultures. Progress has been made in cross-cultural adaptation of outcome measures in recent years, Reference Chan and Huxley43 and all measures used in this study were carefully translated to ensure cultural appropriateness. Nevertheless, the meaning of the concepts behind these measures may vary across cultures. For example, it has been argued that recovery may take different forms in non-Western cultures, with more emphasis on trauma, a person’s choice, risk-taking, coping with challenges and spirituality, Reference van Weeghel, van Zelst, Boertien and Hasson-Ohayon44,Reference Kpanake45 and that cultural understandings of recovery need to be broadened. Reference Slade, Amering, Farkas, Hamilton, O’Hagan and Panther46
Our findings contradict results of a recent large trial from England (ENRICH) which did not find effects of peer support on social inclusion and hope. Reference Gillard, Bremner, Patel, Goldsmith, Marks and Foster6 This might be because of differences in measurement, as the ENRICH study used different scales and measured earlier changes (at 4 months). Moreover, the focus of the intervention was different, with an emphasis on PSWs enabling the patient to access available social support rather than directly providing support. Such variations in the emphasis of practice in peer support can help to explain differences in outcomes. A recent typology identified the key components of peer support, showing that components such as ‘relationship building’ and ‘sharing lived experience’, which were essential elements of UPSIDES peer support, were less prominent in the ENRICH intervention. Reference Kotera, Newby, Charles, Ng, Watson and Davidson47 Discrepancies in findings might also have been due to variations between settings, with UPSIDES including many study sites in LMICs, whereas ENRICH took place in one HIC. Further analyses of between-site differences will show whether results in UPSIDES Western European study sites were more similar to those of ENRICH.
Strengths and limitations
This trial had a number of strengths. It had the largest sample size of any randomised controlled trial of peer support for people with mental ill health to date. All participants were recruited from routine clinical services, which increased the generalisability of findings. It was also the first study to evaluate peer support in lower-resources settings and the first multinational evaluation. We acknowledged the importance of co-creation, Reference Åkerblom and Ness48 and all aspects of preparing and carrying out the trial took place in close cooperation between researchers and PSWs from all study sites, including development of the intervention, Reference Nixdorf, Nugent, Aslam, Barber, Charles and Gai Meir29 implementation and training, Reference Ibrahim, Thompson, Nixdorf, Kalha, Mpango and Moran18,Reference Hiltensperger, Ryan, Ben-Dor, Charles, Epple and Kalha49 translation and validation of measures and tools, Reference Charles, Korde, Newby, Grayzman, Hiltensperger and Mahlke33 and evaluation. UPSIDES also built on years of innovation, research and practical experience of peer support across several of the participating study sites, which was essential in developing a flexible intervention that could be adapted to diverse contexts. For example, all three LMIC sites had prior experience in delivering peer support either for people with severe mental health conditions Reference Hall, Baillie, Basangwa, Atukunda, White, Jain, Orr and Read22,Reference Pathare, Kalha, Joseph, Funk, Drew-Bold, Khenti, Kerrigan, Bhattacharya, Peel, Sá, Kishore and Wade25 or in the context of HIV, Reference Smith Fawzi, Siril, Larson, Aloyce, Araya and Kaale26 and two of the three had substantial prior knowledge of research on recovery-oriented interventions, including peer support for people with mental ill health. There was also rich south–north learning, e.g. role modelling of PSWs in LMICs not only for their clients but also for fellow PSWs in HICs and the study team.
Data collection followed standardised procedures across all study sites, with research workers being continuously trained and data quality monitored. Data checks, including review of the data for completeness, logic and consistency, were extensive. We exceeded recruitment targets, delivered the intervention with few protocol violations and obtained outcome data from nearly all participants, despite the challenges of the COVID-19 pandemic. Finally, effects were stable when site was included as an independent variable in the outcome analysis to control for heterogeneity across study sites with respect to participant characteristics and the amount of intervention received. Thus, the pragmatic aspects of our study increased its real-world relevance and meant that the variability in number of sessions was a strength reflecting different resource levels.
This trial also had several limitations. First, we were greatly affected by the COVID-19 pandemic, which required several contingency measures, including deviations from the originally planned timelines. Second, there was heterogeneity not only in terms of the characteristics of participants across sites but also in various aspects of implementation, including the format of delivery (individual or group peer support, or a combination of both). Although this heterogeneity might again be seen as a strength in terms of the trial’s relevance to real-world conditions in a diverse and often unpredictable global context, it also makes it difficult to replicate our results. Third, there were some protocol violations in the delivery of the intervention which could have diluted the observed effects. Fourth, blinding was limited to researchers carrying out data checks and data analysis. Owing to the nature of the intervention, only researchers analysing data could be blinded; research workers collecting data and UPSIDES PSWs could not be masked to allocation status. Fifth, in the absence of a control intervention, non-specific factors could have influenced the results in favour of the intervention arm. Finally, a clinician-based tool was used for health and social functioning; it is probable that other measures could better capture the perspective of the patient.
Outlook
By addressing the holistic and diverse needs of people with severe mental health conditions, peer support interventions such as UPSIDES go beyond the World Health Organization’s mhGAP recommendations, Reference Omigbodun, Ryan, Fasoranti, Chibanda, Esliker and Sefasi50 towards realising recovery-oriented, person-centred, empowering and rights-based mental healthcare. 51 Although we showed that UPSIDES peer support is feasible and effective internationally at very different sites, challenges to implementation varied widely. In line with multi-country evaluations of complex interventions, Reference Masset, Shrestha and Juden52 there needs to be differentiation between core principles of peer support and variable specific implementation practices, e. g. one-to-one versus group delivery. As a global mental health trial with a focus both on evaluation and capacity-building, our study was perhaps more amenable to context-specific modification than single-site studies in HICs with a primary focus on evaluation. This balance of evaluation and capacity-building may provide future pathways to further scale up (adapting to different settings) and scale out (reaching out to other target groups, e.g. younger people Reference Gardner, Filia, Killackey and Cotton53 and older adults Reference Ronzi, Orton, Pope, Valtorta and Bruce54 ) UPSIDES peer support by selectively prioritising intervention elements on the basis of contextual factors and target populations.
Our next planned analyses include a process evaluation focusing on mediators and moderators of effect, with a special focus on site-specific differences and fidelity; Reference Hiltensperger, Kotera, Wolf, Nixdorf, Charles and Farkas55 a cost-effectiveness analysis; and investigation of effect duration using 4- and 12-month data. We also plan to investigate the impact on PSWs, with a focus on the mechanisms involved in their provision of peer support, such as the impact of repeated self-disclosure on PSWs in high-stigma sites. Although our findings indicate promising effects, more trials are needed in LMICs to advance global mental health insights. Implementation science studies, e.g. hybrid implementation–effectiveness research designs, may be more appropriate to better understand how differences in implementation affect outcomes, while advancing the science of peer support. Another important direction will be to evaluate peer support in humanitarian contexts, as we found an effect even in the context of significant disruption by the COVID-19 pandemic.
Our trial provides evidence that peer support can serve as an effective component of recovery-oriented mental healthcare in diverse settings. Ultimately, UPSIDES will inform mental health policy, implementation and practice, ensuring that the perspectives and unique contributions of people with lived experience are considered in moving mental health systems towards a recovery- and rights-based orientation.
Supplementary material
The supplementary material is available online at https://doi.org/10.1192/bjp.2025.10299
Data availability
Individual participant data that support the findings of this study, after de-identification, and the statistical analysis plan and analytical code will be available in the OPARU repository at https://oparu.uni-ulm.de/xmlui/, following an embargo until 31/12/2025, to allow prioritised generation of research findings by members the UPSIDES consortium.
Acknowledgements
The study Using Peer Support In Developing Empowering Mental Health Services (UPSIDES) is a multicentre collaboration between the Department for Psychiatry and Psychotherapy II at Ulm University, Germany (B.P., coordinator); the Institute of Mental Health at the University of Nottingham, UK (M.S.); the Department of Psychiatry at University Hospital Hamburg-Eppendorf, Germany (C.M.); Butabika National Referral Hospital, Uganda (J.N.); the Centre for Global Mental Health at London School of Hygiene and Tropical Medicine, UK (G.R.); Ifakara Health Institute, Dar es Salaam, Tanzania (D.S.); the Department of Social Work at Ben Gurion University of the Negev, Be’er Sheva, Israel (G.M.); and the Centre for Mental Health Law and Policy, Pune, India (J. Kalha). For their valuable contributions to this work, we thank: the members of the UPSIDES-RCT Trial Steering Committee (Carrie Brooke-Sumner, South African Medical Research Council, Cape Town, South Africa; Dickens H. Akena, Makerere University College of Health Sciences, Kampala, Uganda; Peter Brieger, kbo-Isar-Amper-Klinikum, Munich, Germany); the members of the UPSIDES Data Safety and Monitoring Board (Stefan Wesner, University of Cologne, Germany; David Jemba, IT consultant, Entebbe, Uganda); the members of the UPSIDES International Advisory Board (Marianne Farkas, Boston University, USA; Michelle Funk, World Health Organization, Geneva, Switzerland; Nigel Henderson, Penumbra, Edinburgh, Scotland; Sylvia Kaaya, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; Stefan Weinmann, Klinik an der Lindenhöhe, Offenburg, Germany; and Charlene Sunkel, Global Mental Health Peer Network, Paarl, South Africa); and UPSIDES ethics advisor Felicitas Söhner, Düsseldorf University, Germany.
Author contributions
B.P., M.S., C.M., J.N., G.R., D.S., G.M. and J. Kalha conceived the trial and also wrote the trial protocol, with the help of A.M.-S., S.K., A.C., R. Nixdorf, R. Mpango, M.R., A.G., S.P., B.M., M.L. and P.G.-E. All authors contributed to implementation in various roles (recruitment, training and delivery of the intervention, data collection, data check, data analysis). B.P., J.N., R.H. and P.W. wrote the initial draft of the manuscript, supported by M.S. and G.R. All authors read and revised the manuscript and approved the final version.
Funding
UPSIDES has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement no. 779263. This publication reflects only the authors’ views. The Commission is not responsible for any use that may be made of the information it contains.
Declaration of interest
None.







eLetters
No eLetters have been published for this article.