The Australian Government’s National Critical Care and Trauma Response Centre (NCCTRC) possesses a 60-bed deployable air-conditioned field hospital that provides equipment for emergency/maternity care, resuscitation and radiology. The field hospital is also equipped with a pathology laboratory, pharmacy, sterilization facility, a morgue, and staff habitats with kitchen and storage. 1 The NCCTRC field hospital is ideal for scenarios that allow road access and sufficient time for deployment.
Although preparedness through a readily deployable, fit-for-purpose field hospital is valuable, disasters may unfold rapidly and unpredictably, precluding the possibility of relying on such resources. Empirical research is needed to understand the complexity of the challenge (e.g., if a field hospital set up must be managed locally by the evacuating hospital, without any external supports). This research addresses that by presenting the narrative of a field hospital setup that had to be expedited due to immediate risk of flooding in a 60-bed community hospital. The hospital has more than 100 staff members managing an Emergency Department (ED), rehabilitation unit, hemodialysis unit, and an oncology unit, along with in-patient wards. Extensive flooding in 2 Australian states of Queensland and New South Wales in early 2022 impacted 14 million people, 26 of whom died, and destroyed or damaged 8000 homes, triggering insurance claims of $4.29 billion Australian Dollars. 2 This large-scale flooding also impacted the community hospital as flood waters were forecasted to enter the hospital building in few hours, leaving insufficient time for the NCCTRC field hospital to reach the site and accommodate evacuated patients. Additionally, most of the roads leading to the site were already submerged, making deployment impossible. Despite the presence of back up mechanisms, hospitals can be forced to create their own underequipped field hospitals or shelters, in circumstances where the facility gets isolated. This research aimed to investigate and briefly report an evacuation and field hospital set up to disseminate the key measures that can help other hospitals plan for similar disaster scenarios.
A qualitative study was undertaken which involved primary data collection through 9 key informant interviews and secondary data collection through analyses of published accounts of hospital’s disaster response. A narrative analysis of the collected data provided an interpretive account of key informants’ experiences in hospital evacuation and field hospital set up. All research participants had either led the flood-affected hospital’s evacuation from the ground or directed the whole operation from the hospital network headquarters or the state health department. This included the perspectives of senior management of the hospital network and state government, the physicians that led the evacuation of ED and the wards, and the senior nursing staff that supported all patients during the evacuation.
Primary data was collected through 9 interviews that took place between January 30, 2023 and April 4, 2024. In 1 interview, the account was provided in-person at the headquarters of the hospital network; all remaining sessions were conducted on MS Teams. Inductive thematic analysis on the model of Kiger and Varpio (2020) was conducted to capture the main themes narrated by participants.Reference Kiger and Varpio 3 Narrations of hospital evacuation in the news and a specialty publication were matched with participants’ accounts to strengthen the validity of narrative analysis.Reference Vennell 4 , Reference Knaus 5
Narrative
In early 2022, coincidence of exceptionally high tides and unprecedented riverine swelling threatened an Australian district hospital located next to an estuary on the east coast of Australia. At 6 pm on March 1, 2022, the local police advised the clinicians to evacuate to a nearby school. The advice triggered a process of internal deliberation on the feasibility of sheltering in place to avoid exposing patients to the risks of unplanned evacuation. The hospital staff cross checked the directive with their supervisors at the headquarters of the hospital network and agreed that risks outweighed benefits as flood waters were expected to rise above the ground floor level of the hospital building in few hours. A whole hospital evacuation was then set in motion, which engaged 4 agencies, namely the State Emergency Services (SES), Local Government, the State Police, and the ambulance service, to evacuate 55 patients, essential equipment, and medications. The SES and Police arranged buses for ambulant patients and specialized vehicles for movement of equipment. Clinicians were split between 2 sites so as to have enough staff at both the evacuating hospital and the receiving site, and to also accompany patients in-transit. The staff in different locations coordinated to track the movement of patients each of whom was sent with identification tags, notes, and medication charts.
Clinicians initiated the evacuation work by identifying patients that could be discharged into their family’s care and staff were tasked to make phone calls to families. A relatively healthy patient was evacuated to the field hospital when her family could not be contacted. On the other hand, an acutely unwell immunocompromised patient was transferred to his family’s care to avoid his exposure to unpredictable risks of evacuation and the field hospital environment. The dialysis patients and those at risk of acute deterioration were transferred to the nearest tertiary hospital. The clinicians interviewed reported putting extra emphasis on providing situational awareness to all patients, including those with cognitive decline, to curb their anxiety and assure them of their safety. Effective patient communication was not deprioritized despite scarcity of time, and all patients received personalized briefings from clinicians with whom they were familiar. A quick exodus of patients was planned to have everyone out well before the entry of flood waters on hospital floors, and so healthier patients were moved first.
A doctor and nurse were dedicated to the task of identifying and gathering essential items for the field hospital. They took all medications that could be needed at the field hospital. Figure 1 lists examples of the items that clinicians determined would be necessary to set up an emergency department and manage potential critical patients in the field hospital setting. Most of the essential resources were collected and transported while evacuating the hospital, but some items were either not available or had to be picked up by making trips to the evacuated facility.
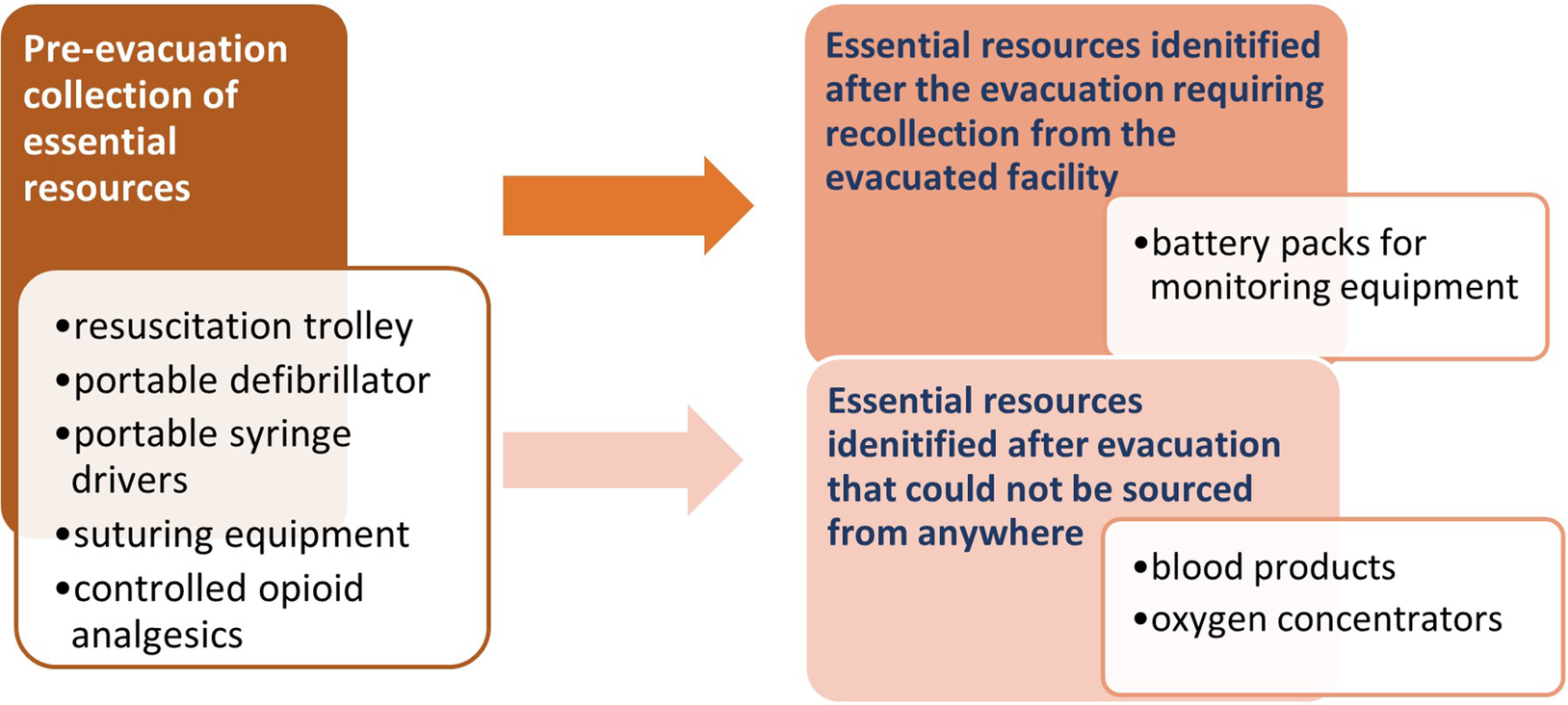
Figure 1. Essential resources required at the field hospital, identified before or after the evacuation.
The hurried identification and transfer of critical medications and equipment, mostly in private cars, proved lifesaving, as within 1 hour of set up, the field ED treated patients suffering from Acute Kidney Injury (AKI), sepsis, dog bites, bowel obstruction, and sodium deficiency.Reference Vennell 4 The triage section of the ED was set up in 1 classroom and the resuscitation subsection in another. A separate area was also created to provide privacy to a patient with a life limiting diagnosis, who later passed away in that space while receiving uninterrupted palliative care. The newly created field hospital used air mattresses for all patients except those in resuscitation subsection of the ED and did not have pathology laboratory, morgue, and staff habitats. Many volunteers stepped in to offer help at the field hospital, but there were not enough generic tasks that could be delegated to each volunteer, creating the problem of unmanaged overcrowding at the field hospital. Research participants acknowledged and appreciated the volunteering spirit but also felt that security should have been provided to manage the crowd of volunteers.
During the evacuation, the clinicians had to work around certain significant disruptions which included power and telecommunication outages, and an incoming emergency patient, flown in on a helicopter. Incident command was not clearly defined, so a nurse manager assumed the role of incident controller, and in the physicians’ space, a doctor improvised to coordinate the work towards the goal of safe evacuation. The hospital floor was expected to be a meter underwater, so before the departure of the last staff member, computers, valuable equipment, and patient trolleys were put on high ground and the facility was locked to protect its remaining contents.
Discussion and Conclusion
The analysis of multiple accounts of the hospital evacuation highlighted both the generalizable safety enhancing measures implemented by clinicians, and the shortcomings that could have compromised patient safety. The positive measures included transferring patients with their notes and improvising an incident command system. The shortcomings included lack of security for crowd control and the absence of a business continuity plan for relocation and field hospital setup.
The hospital staff showed remarkable initiative in transferring patients with their records to assist receiving clinicians in ensuring continuity of care. The evacuation had to be completed before the rise of flood waters and organized management of each patient’s notes is not always possible in time-constrained evacuations or with a large number of patients. A nuclear disaster in 2011 triggered an immediate evacuation of hospital patients in Japan and clinicians were unable to dispatch any records or notes with patients, making it difficult for receiving hospitals to continue care.Reference Yanagawa, Miyawaki and Shimada 6 Similar absence of accompanying patient information was observed in a patient evacuation conducted after a London hospital fire in 2008,Reference Wapling, Heggie and Murray 7 and post-earthquake evacuation in New Zealand in 2011.Reference Irvine, Buttimore, Eastwood and Kendrick-Jones 8 Evacuated patients with cognitive impairments cannot always articulate their symptoms, needs, and ongoing treatment, and so receiving clinicians’ access to such patients’ medical records is imperative to continuity of safe care. Cloud storage, safe from unauthorized access, can work around post-disaster power disruptions to maintain receiving clinicians’ access to medical records.
Various hospitals forced to evacuate their patients after 2005 Hurricane Katrina’s unprecedented flooding faced coordination difficulties due to the lack of clear incident command system.Reference Gray and Hebert 9 Most clinicians interviewed in this research lacked knowledge of hospital’s evacuation plan and so were not aware of the designated incident commander. However, they improvised to set incident controllers or coordinators for both physicians and nurses.
Internal post-evacuation evaluation by hospital network staff highlighted the necessity of having a relocation plan, which did not exist before the flooding. The absence of a tailored plan left evacuating clinicians guessing what they should take to the school (field hospital) to enable continuity of care. The foremost planning measure identified by most research participants was to have a list of equipment, medications, and utilities beforehand that clinicians would need to sustain an isolated or disconnected field hospital for a prolonged period. Although an evacuation plan existed beforehand, clinicians spearheading the evacuation were unaware of the plan and they later recommended task cards providing evacuation or relocation directives instead of thick planning documents to enable quick sourcing of critical information on how to evacuate and what would be needed at the field hospital. Besides lack of knowledge of field hospital requirements, another problem faced by clinicians was the need for security to control the crowds of volunteers. The security was also needed by hospitals evacuating in the aftermath of hurricane Katrina and should be viewed as an essential preparedness measure.Reference Bernard and Mathews 10 , Reference Taylor 11 The practical recommendation of crowd control of volunteers can be implemented by specifying pre-trained security personnel in hospital contingency plans. Such plans should also implement specification of essential relocatable equipment and medications that clinicians would require to sustain evacuated patients’ care in isolated settings.
The narrative analysis highlighted a range of measures that hospitals can plan to enact a rapid field hospital setup and patient evacuation. These generalizable planning measures hold potential in preparing hospitals for unpredictable disaster scenarios and lowering disaster-related mortality and morbidity risks of hospital patients.
Author contribution
FSN conceptualized the research and KC, JCL, MS, and JB co-designed the research. FSN, KC, JCL and MS developed the interview questions and refined the data collection methodology. FSN collected data through online interviews. Data analysis and initial write-up was done by FSN. KC, JL, MS and JB refined the manuscript through multiple revisions. All authors developed the final manuscript.
Acknowledgements
The authors are grateful to all clinicians and administrative managers that participated in meetings and research interviews and are also grateful for the approval and support provided by the Local Health District (LHD). Authors are also grateful for the administrative support of the Australian Institute of Health Innovation.
Funding statement
This work is supported by a Macquarie University Research Excellence (MQRES) Scholarship (20203593), associated with the Australian Institute of Health Innovation. KC, MS, and JB are each supported by an NHMRC Investigator Grant (APP2007765, APP2007970 and APP1176620). MS is also supported by Sydney Horizon Fellowship. The funding bodies did not contribute to the research in any form or manner.
Competing interests
All authors declare that they have no competing interests.
Ethical standard
This research was developed and conducted in accordance with Australia’s National Statement on Ethical Conduct in Human Research 2023. The ethical approval for this research was granted by the Medicine and Health Sciences Subcommittee of Macquarie University’s Human Research Ethics Committee: Reference No: 520221213642123, Project ID: 12136.


