Inflammatory markers encompass a variety of proteins and signaling molecules that facilitate immune activity and maintain overall health. Concentrations of inflammatory markers measured in the blood are often used to assess immune functioning. Chronic inflammation, marked by a persistent state of heightened immune activity, is associated with the development of conditions including heart disease and type 2 diabetes (Danesh et al., Reference Danesh, Kaptoge, Mann, Sarwar, Wood, Angleman and Gudnason2008; Theuma & Fonseca, Reference Theuma and Fonseca2003). Psychosocial stressors can activate inflammatory responses with implications for a variety of health outcomes (Liu, Wang, & Jiang, Reference Liu, Wang and Jiang2017; Steptoe, Hamer, & Chida, Reference Steptoe, Hamer and Chida2007). Childhood adversity in particular is an established environmental risk factor for the health conditions mentioned above and chronic inflammation later in life (Hostinar, Lachman, Mroczek, Seeman, & Miller, Reference Hostinar, Lachman, Mroczek, Seeman and Miller2015; Kerr, McDonald, & Minnis, Reference Kerr, McDonald and Minnis2021; Lacey, Pinto Pereira, Li, & Danese, Reference Lacey, Pinto Pereira, Li and Danese2020). Thus, inflammation is likely a biological mechanism connecting childhood adversity to poor health during adulthood. However, not all individuals with childhood adversity exhibit later inflammation. Differences among individual vulnerabilities to stressors may play a role. Using a nationally representative sample of United States adults, we investigated whether the association between early adversity and adult inflammation is moderated by past 12-month emotional distress symptoms and trait neuroticism.
There is a reliable association between early life stress and increased health complications in adulthood (e.g. chronic inflammation); however, the severity and frequency of these outcomes can vary widely across individuals (Hostinar & Miller, Reference Hostinar and Miller2019; Oh et al., Reference Oh, Jerman, Silvério Marques, Koita, Purewal Boparai, Burke Harris and Bucci2018). Factors tied to stress vulnerabilities, including how individuals tend to appraise and respond to adversity, may modulate these health outcomes. For example, a recent study using data from the Midlife in the United States (MIDUS) project found that adults with a history of early adversity using more adaptive coping strategies experienced fewer physical health conditions, including autoimmune and bone conditions, compared to those using these strategies less often (Sheffler, Piazza, Quinn, Sachs-Ericsson, & Stanley, Reference Sheffler, Piazza, Quinn, Sachs-Ericsson and Stanley2019). Similarly, in adults who experienced childhood maltreatment, higher self-reported control of emotions was associated with lower inflammation (Gouin, Caldwell, Woods, & Malarkey, Reference Gouin, Caldwell, Woods and Malarkey2017; Jones, Marsland, & Gianaros, Reference Jones, Marsland and Gianaros2023). Therefore, the long-term effects of early life stress may vary as a function of trait-level individual differences – one's personal capacity to respond adaptively may influence the likelihood of chronic inflammation during adulthood.
Emotional distress psychopathology along with elevated personality traits of neuroticism reflect putative stress vulnerabilities capable of moderating the association between early adversity and later inflammation. Emotional distress conditions (e.g. generalized anxiety disorder [GAD] and major depressive disorder [MDD]) are more common among individuals who have experienced early adversity (Danese et al., Reference Danese, Moffitt, Pariante, Ambler, Poulton and Caspi2008; Nanni, Uher, & Danese, Reference Nanni, Uher and Danese2012). Moreover, these conditions have been shown to be associated with reduced immune system functioning (Beurel, Toups, & Nemeroff, Reference Beurel, Toups and Nemeroff2020). Despite this, symptoms of anxiety and depression, if included in statistical models of adversity and inflammation, are often treated as confounds (and modeled as covariates) rather than as potential moderators (Coelho, Viola, Walss-Bass, Brietzke, & Grassi-Oliveira, Reference Coelho, Viola, Walss-Bass, Brietzke and Grassi-Oliveira2014). Conversely, in studies examining MDD and GAD as main effect statistical predictors of inflammatory markers (Costello, Gould, Abrol, & Howard, Reference Costello, Gould, Abrol and Howard2019; Duivis, Vogelzangs, Kupper, de Jonge, & Penninx, Reference Duivis, Vogelzangs, Kupper, de Jonge and Penninx2013; Michopoulos, Powers, Gillespie, Ressler, & Jovanovic, Reference Michopoulos, Powers, Gillespie, Ressler and Jovanovic2017; Ogłodek, Szota, Just, Szromek, & Araszkiewicz, Reference Ogłodek, Szota, Just, Szromek and Araszkiewicz2016), the role of early adversity is not always examined. While some studies have examined the joint effects of emotional distress symptoms and early adversity on inflammation at midlife, inconsistencies exist. Specifically, some studies indicate that individuals with both depressive symptoms and early adversity have higher inflammation levels than those with only adversity but no depressive symptoms (Danese et al., Reference Danese, Moffitt, Pariante, Ambler, Poulton and Caspi2008; Gill et al., Reference Gill, El-Halabi, Majeed, Gill, Lui, Mansur and Rosenblat2020). However, other studies have found no differences in inflammatory markers when comparing these groups (Baumeister, Akhtar, Ciufolini, Pariante, & Mondelli, Reference Baumeister, Akhtar, Ciufolini, Pariante and Mondelli2016; Coelho et al., Reference Coelho, Viola, Walss-Bass, Brietzke and Grassi-Oliveira2014; Palmos et al., Reference Palmos, Watson, Hughes, Finkelmeyer, McAllister-Williams, Ferrier and Powell2019).
Inconsistencies surrounding the combined influence of emotional distress symptoms and early adversity may stem in part from reliance on case-control methodology. Case-control designs group individuals based on discrete diagnostic categories such as MDD or GAD, which limits the ability to study how symptoms co-occurring across diagnoses may influence inflammatory outcomes (Moriarity & Alloy, Reference Moriarity and Alloy2020; Thylur & Goldsmith, Reference Thylur and Goldsmith2022). Transdiagnostic internalizing (i.e. emotional distress) symptoms are psychiatric comorbidities commonly observed across depression, anxiety, and fear-based conditions (Krueger, Reference Krueger1999). These transdiagnostic features are often overlooked in case-control research, potentially obscuring when similar associations with inflammation exist across various internalizing conditions. Indeed, one meta-analysis found that diagnoses of clinical depression and anxiety both demonstrated similarly elevated inflammation compared to non-clinical populations (Tursich et al., Reference Tursich, Neufeld, Frewen, Harricharan, Kibler, Rhind and Lanius2014); this is consistent with a shared, transdiagnostic mechanism across these conditions.
Neuroticism is a broad personality trait associated with heightened emotional reactivity, tendencies towards negative affect, and increased sensitivity and reactivity to stressors (Claridge & Davis, Reference Claridge and Davis2001; Griffith et al., Reference Griffith, Zinbarg, Craske, Mineka, Rose, Waters and Sutton2010). It is relatively stable during adulthood and acts as a non- specific predictor of various internalizing conditions (Costa & McCrae, Reference Costa and McCrae1988; Ormel & Wohlfarth, Reference Ormel and Wohlfarth1991). Importantly, measures of neuroticism assess content closely associated with the transdiagnostic comorbidities common across emotional distress diagnoses. In other words, neuroticism can serve as an effective marker of the shared variance across depression, anxiety, and fear-based psychopathologies (Griffith et al., Reference Griffith, Zinbarg, Craske, Mineka, Rose, Waters and Sutton2010). Evidence for associations between neuroticism and chronic inflammation is mixed. An earlier meta-analysis, which included MIDUS data, did not observe a consistent main effect association between neuroticism and inflammation (Luchetti, Barkley, Stephan, Terracciano, & Sutin, Reference Luchetti, Barkley, Stephan, Terracciano and Sutin2014). Yet, the combined effect of neuroticism and adversity can be critical when considering associations with inflammation (Wang et al., Reference Wang, Lin, Liu, Lv, Wang, Wei and Si2022). Elliot, Turiano, and Chapman (Reference Elliot, Turiano and Chapman2017) performed a moderation analysis within a subsample of MIDUS examining the personality trait of neuroticism combined with socioeconomic status (SES) to predict individual inflammation markers. Lower SES was associated with inflammation, but only when neuroticism was high. Given the known connection between lower SES and adverse childhood experiences (Walsh, McCartney, Smith, & Armour, Reference Walsh, McCartney, Smith and Armour2019), it is possible that neuroticism specifically and transdiagnostic emotional distress more generally also reflect vulnerabilities to adverse life events on health outcomes.
The current study expands upon previous MIDUS research, which demonstrated associations between early adversity and individual markers of adult inflammation (Hostinar et al., Reference Hostinar, Lachman, Mroczek, Seeman and Miller2015), as well as separate associations between transdiagnostic internalizing psychopathology and general health outcomes (e.g. all-cause mortality; Kim et al., Reference Kim, Turiano, Forbes, Kotov, Krueger and Eaton2021). Specifically, we investigated whether (Aim 1) the relationship between childhood adversity and inflammation at midlife is moderated by a latent estimate of past 12-month internalizing symptomatology and trait neuroticism using confirmatory factor analysis (CFA). In addition, we directly compared (Aim 2) transdiagnostic v. disorder-specific emotional distress (i.e. residual terms) when examining the connection between early adversity and inflammation in adulthood. Furthermore, our analyses used a latent estimate of chronic inflammation across multiple biomarker assays. This study is consistent with the goals of MIDUS to better understand the transdiagnostic processes of psychosocial resilience, adult well-being, and physical health. Ultimately, this may aid in identifying adults with childhood adversity who are vulnerable to worse health outcomes at midlife, thereby informing screening efforts focused on prevention and treatment.
Methods
Sample
This study used publicly available data from the MIDUS project (Ryff et al., Reference Ryff, Almeida, Ayanian, Carr, Cleary, Coe and Williams2007). In 1995, MIDUS recruited 7108 non-institutionalized adults via random digit dialing from the contiguous United States. In 2004, 5555 participants (75%) of the original sample were recruited for a second wave of data collection (MIDUS II). In the second wave, The Biomarker Project was initiated, involving a subsample (n = 1054) who underwent a 2-day study visit, including the collection of blood. Additionally, an African American subsample from MIDUS I was re- recruited and 201 of these individuals completed the Biomarkers protocol. In total, 1255 participants contributed valid biomarker data. The average time between the questionnaires/phone interviews and biomarker collection was 26.5 (s.d. = 14.0) months. For our analyses, 1.5% of the data was missing. Missing data was deemed completely at random using the vis_miss() visualization function within the R package Naniar (Tierney & Cook, Reference Tierney and Cook2020); multiple imputation was employed (Slopen et al., Reference Slopen, Lewis, Gruenewald, Mujahid, Ryff, Albert and Williams2010). All data transformations were performed after reporting sample characteristics in Table 1.
Table 1. Descriptive statistics of study sample
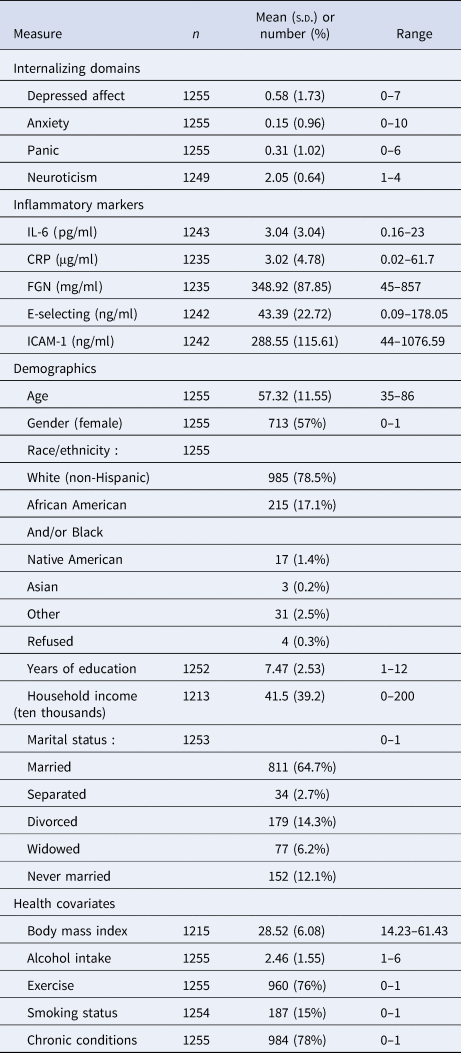
Note. Descriptive statistics of study variables.
Measures
Inflammation
Serum markers of inflammation were collected from fasting blood samples. C-Reactive Protein (CRP) was quantified using a particle-enhanced immunonephelometric assay (BNII nephelometer, Dade Behring Inc., IL). Interleukin-6 (IL-6) was measured with the Quantikine High-sensitivity ELISA kit #HS600B (R&D Systems, MN). Fibrinogen (FGN) assessment used the BNII nephelometer (N Antiserum to Human Fibrinogen; Dade Behring Inc., IL). E-Selectin was measured through a high-sensitivity ELISA assay (Parameter Human sE-Selectin Immunoassay; R&D Systems, MN). Soluble Intracellular Adhesion Molecule-1 (ICAM-1) was quantified with an ELISA assay (Parameter Human sICAM-1 Immunoassay; R&D Systems, MN). Intra- and inter-assay coefficients of variance were in acceptable range (<10%) for all assays. Guided by previous MIDUS analyses (Hostinar et al., Reference Hostinar, Lachman, Mroczek, Seeman and Miller2015), values exceeding the 99.9th percentile were replaced with values 4 s.d.s from the mean. IL-6 and CRP were log-transformed to correct for positively skewed distributions (Friedman & Herd, Reference Friedman and Herd2010; Slopen et al., Reference Slopen, Lewis, Gruenewald, Mujahid, Ryff, Albert and Williams2010; Straka, Tran, Millwood, Swanson, & Kuhlman, Reference Straka, Tran, Millwood, Swanson and Kuhlman2021). All inflammatory variables were z-transformed.
Internalizing distress
Four continuous mental health measures were used to model a transdiagnostic internalizing distress factor (Kim et al., Reference Kim, Turiano, Forbes, Kotov, Krueger and Eaton2021). Past 12-month depression, anxiety, and panic were assessed using the Composite International Diagnostic Interview–Short Form (CIDI-SF) version 10. Thus, this assessment timeframe reflects more typical emotional functioning rather than acute states. The CIDI-SF has high agreement (91–94%) with its lengthier CIDI counterpart (Kessler, Andrews, Mroczek, Ustun, & Wittchen, Reference Kessler, Andrews, Mroczek, Ustun and Wittchen1998). The fourth indicator assessed neuroticism, which was developed from existing personality inventories and exhibits acceptable internal consistency (Cronbach's α = 0.74) (Lachman & Weaver, 2007). Neuroticism reflects a general disposition towards negative emotions and is an effective transdiagnostic marker of internalizing distress (Griffith et al., Reference Griffith, Zinbarg, Craske, Mineka, Rose, Waters and Sutton2010). Depression, anxiety, and panic measures were log-transformed following other MIDUS analyses (Eaton, Krueger, & Oltmanns, Reference Eaton, Krueger and Oltmanns2011). All internalizing measures were z transformed.
Adverse childhood experiences
A cumulative sum of adverse childhood experiences (ACEs) (Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards and Marks1998) was constructed consistent with previous MIDUS studies (Hostinar et al., Reference Hostinar, Lachman, Mroczek, Seeman and Miller2015; Sheffler et al., Reference Sheffler, Piazza, Quinn, Sachs-Ericsson and Stanley2019). MIDUS assessed eight historical experiences (before age 18): physical abuse, emotional abuse, sexual abuse, emotional neglect, physical neglect, parental divorce, parental substance abuse, and parental depression. The first five ACEs listed above were obtained from Childhood Trauma Questionnaire (CTQ) scales and collapsed into binary responses using thresholds listed in the manual (Bernstein & Fink, Reference Bernstein and Fink1998). The CTQ is an established measure of childhood adversity demonstrates high agreement with external sources (Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia and Zule2003). The latter three ACEs items are specific to MIDUS II questionnaires (yes/no format) with questions like ‘Parent's drug use ever caused problems?’ and ‘Mother depression?’ Only events occurring before age 18 were counted. Due to less frequent endorsement of 4 or more items as well as evidence that 4 or more ACEs is associated with worse clinical outcomes (Mersky, Topitzes, & Reynolds, Reference Mersky, Topitzes and Reynolds2013), total scores equal to or greater than 4 were collapsed into one category. Pre-imputation class memberships for ACEs levels were as follows: 0 (n = 583), 1 (n = 286), 2 (n = 132), 3 (n = 90), and ⩾ 4 (n = 103).
Covariates
Sociodemographic variables were included as covariates in follow-up analyses ([see Analyses] [https://midus.wisc.edu/] Ryff et al., Reference Ryff, Almeida, Ayanian, Carr, Cleary, Coe and Williams2007). Sex assigned at birth and marital status were dummy coded (0 = male, 1 = female; 0 = married, 1 = non-married). Following previous methods (Elliot & Chapman, Reference Elliot and Chapman2016; Friedman & Herd, Reference Friedman and Herd2010), the most common race/ethnicity (white-non-Hispanic) was used as the reference, while less common African American, Hispanic, or other race/ethnicity identities were collapsed to 1. Household income reflected total family income in the past 12 months. Educational attainment ranged from 1 = no school/grade school to 12 = Ph.D./M.D./professional degree. Sociodemographic factors such as these have been associated with inflammation (Friedman & Herd, Reference Friedman and Herd2010; Nowakowski & Sumerau, Reference Nowakowski and Sumerau2015).
Furthermore, smoking status and past month alcohol consumption served as health covariates in follow-up analyses (see Analyses). Smoking status was dummy coded, with non- smokers as the baseline. Alcohol consumption was categorized as 1 = Never, 2 = Less than 1x/week, 3 = 1–2x/week, 4 = 3–4x/week, 5 = 5–6x/week, and 6 = Daily. Both smoking status and alcohol intake have been found to influence inflammation (Gonçalves et al., Reference Gonçalves, Coletta, Silvério, Benevides, Casati, da Silva and Nociti2011; Imhof et al., Reference Imhof, Froehlich, Brenner, Boeing, Pepys and Koenig2001). Body mass index (BMI), exercise, and presence of medical conditions were also examined as health covariates due to their known associations with inflammation (Metsios, Moe, & Kitas, Reference Metsios, Moe and Kitas2020; Pahwa, Goyal, & Jialal, Reference Pahwa, Goyal and Jialal2023; Rodríguez-Hernández, Simental-Mendía, Rodríguez-Ramírez, & Reyes-Romero, Reference Rodríguez-Hernández, Simental-Mendía, Rodríguez-Ramírez and Reyes-Romero2013). Exercise was binary (1 = 20 min or more physical activity 3x/week). Various other chronic conditions were coded as 0 = No Condition and 1 = Present Condition.
Analyses
All analyses were performed using RStudio version 1.4.1717 (R version 4.1.0). We performed exploratory factor analyses (EFA; ‘Psych’ package) with oblimin rotations to examine the factor structure of mental health and inflammation variables. We used scree plots and initial loading cutoff values of 0.3 to guide interpretations and modeling decisions. We conducted CFAs using the ‘lavaan’ package to build latent measurement models of internalizing and inflammation (Rosseel, Reference Rosseel2012). Model fit was assessed with the χ2 goodness-of-fit statistic, confirmatory fit index ([CFI] Bentler, Reference Bentler1990), Tucker Lewis Index (TLI), standardized root mean square residual (SRMR), and root mean square error of approximation ([RMSEA] Steiger, Reference Steiger1990). In addition, Akaike information criterion (AIC) and Bayesian information criterion (BIC) were used to compare different models.
We used a series of hierarchical linear regressions to predict the factor scores of inflammation (Aim 1). In the first step, ACEs and the broad internalizing factor were used as separate main effect predictors. The interaction term with internalizing and ACEs was included in the second step. Johnson-Neyman analyses were used to probe and visualize the interaction. Sociodemographic covariates were included in the third step and health covariates were introduced in the fourth step. This was done to explore if the internalizing-ACEs interaction term predicted inflammation over-and-above the associations between covariates and inflammation.
Inclusion of health covariates in particular can diminish effect sizes between mood indices and inflammation (Appleton, Buka, Loucks, Gilman, & Kubzansky, Reference Appleton, Buka, Loucks, Gilman and Kubzansky2013; Winter, Riordan, Conner, & Jose, Reference Winter, Riordan, Conner and Jose2021). This may be due to shared processes underlying inflammation and physical health. We performed follow-up analyses considering each health covariate individually. After observing how BMI eliminated the significant internalizing-ACEs effect, we repeated hierarchical regression models using BMI as the outcome variable instead of inflammation. Therefore, we tested if internalizing distress was functioning as a similar vulnerability with ACEs when predicting BMI.
Finally, we examined whether transdiagnostic internalizing or disorder-specific features moderated the association between ACEs and inflammation (Aim 2; i.e. broad comorbidity v. disorder-specific symptoms). Two simultaneous interaction terms were incorporated into the model: ACEs interacting with the broad internalizing factor scores and ACEs interacting with each unique residual component for a specific disorder. Only one disorder residual was included at a time. The neuroticism residual was conceptualized as measurement error and was not included. Neuroticism was included solely to improve our estimate of latent internalizing distress given the item content with relevance for all three disorder-specific domains in these models. For all study models, main and interaction effects were examined at α = 0.05.
Results
Latent measurement models
All inflammation markers were positively correlated (mean r = 0.26, range [0.09–0.52]; Table 2). EFA supported either a one- or two-factor solution. The one-factor CFA model showed excellent fit (Fig. 1). A two-factor model was initially considered because markers E-Selectin and ICAM-1 had EFA loadings below 0.6 in the one-factor model, but CFA fit for the two-factor model (CFI = 0.99, TLI = 0.98, RMSEA = 0.04, SRMR = 0.02, AIC = 16 788, BIC = 16 845) did not meaningfully improve over the one-factor model (AIC = 16 788, BIC = 16 840). Therefore, the shared variance of the inflammatory indicators was extracted using a single inflammation factor.
Table 2. Bivariate correlations amongst study variables
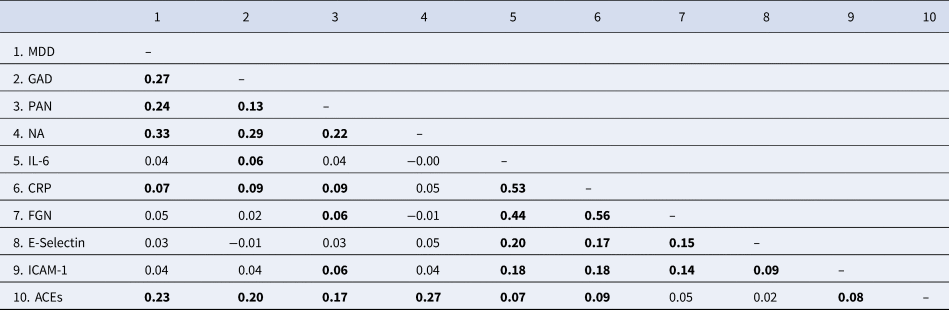
MDD, major depressive disorder; GAD, generalized anxiety disorder; PAN, panic disorder; NA, neuroticism; IL-6, interleukin 6; CRP, c- reactive protein; FGN, fibrinogen; ICAM-1, intercellular adhesion molecule; ACEs, adverse childhood experiences.
Note. Bolded coefficients p < 0.05. Internalizing and inflammatory measures are grouped separately in shaded boxes.
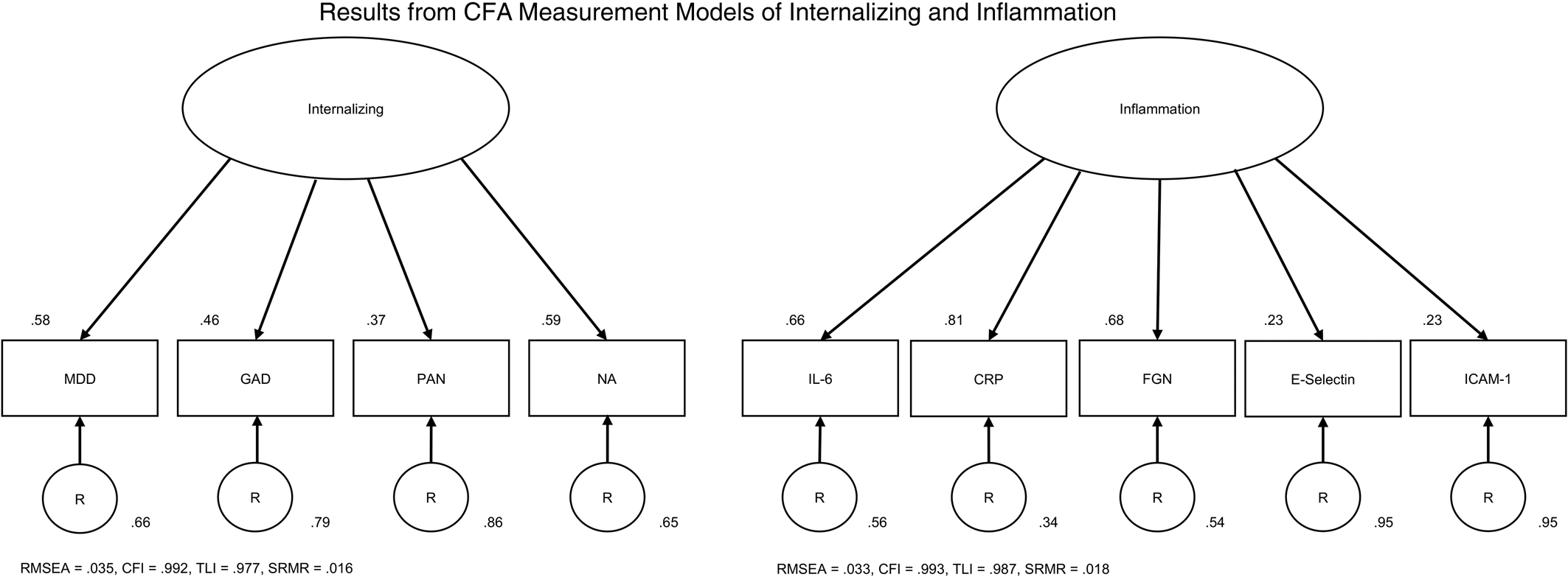
Figure 1. Results from CFA measurement models of internalizing and inflammation. Note: Arrows flowing from the latent factor to its indicators represent factor loadings. Arrows leading from each of the residuals to the indicators represent residual variance. Factor loadings and residual variances obtained using the completely standardized solution. Model fit indices are listed below each measurement model. MDD – major depressive disorder, GAD – generalized anxiety disorder, PAN – panic disorder, NA – neuroticism, IL-6 – interleukin 6, CRP – c-reactive protein, FGN – fibrinogen, ICAM-1 – intercellular adhesion molecule 1, RMSEA – root mean square error of approximation, CFI – comparative fit index, TLI – Tucker-Lewis index, SRMR – standardized root mean square residual.
All four internalizing distress measures were positively correlated (mean r = 0.24, range [0.13, 0.33]; Table 2). EFA results were consistent with the one-factor solution reported in past MIDUS analyses (Kim et al., Reference Kim, Turiano, Forbes, Kotov, Krueger and Eaton2021). The CFA model of internalizing exhibited excellent fit (Fig. 1). Both shared (transdiagnostic internalizing distress) and unique components (depression, anxiety, and panic) were extracted for subsequent analyses.
Internalizing distress psychopathology and early adversity
We examined internalizing distress, ACEs, and their associations with inflammation (Table 3). For the first model step, internalizing (β = 0.083) and ACEs (β = 0.060) both independently predicted greater inflammation. With the second step, the interaction term between internalizing and ACEs was significantly associated with inflammation (β = 0.141); Fig. 2). Johnson-Neyman analyses revealed that a minimum of 2 ACEs was required before a significant positive association emerged between transdiagnostic internalizing distress and inflammation. Also, internalizing distress scores needed to be at the 53rd percentile before a positive association emerged between ACEs and inflammation. After adding sociodemographic variables as covariates in the third step, the interaction between internalizing and ACEs remained significant (β = 0.130).
Table 3. Interactions between ACEs and internalizing on inflammation
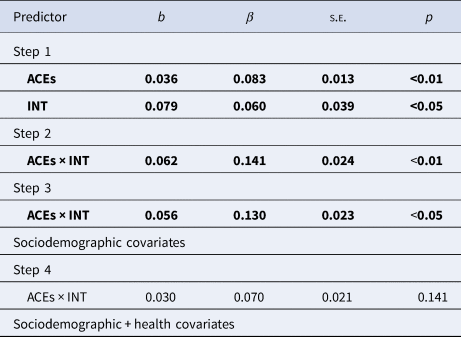
Note. Regression results using internalizing and ACEs as predictors. Bolded text indicates significant effect. ×: Examined for interaction. INT – latent internalizing. ACEs – adverse childhood experiences.
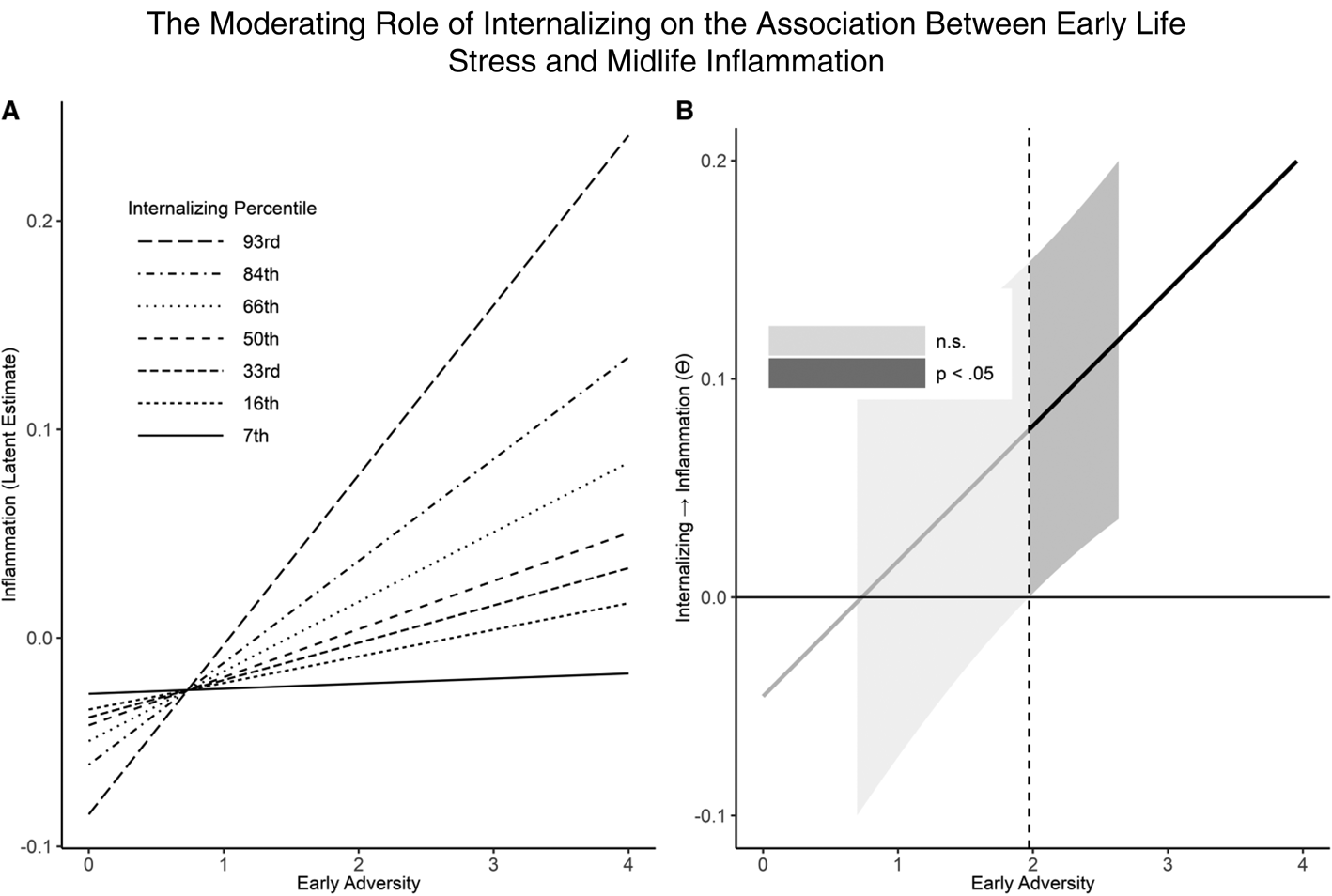
Figure 2. The moderating role of internalizing on the association between early life stress and midlife inflammation. Note: In Figure 2A, associations between early adversity and inflammation are depicted based on internalizing scores. Figure 2B presents a Johnson-Neyman plot illustrating the interaction and highlighting the threshold value of early adversity where a significant interaction emerges. n.s. – not significant.
When adding multiple health covariates simultaneously in the fourth step, the statistical interaction with ACEs and internalizing became non-significant (β = 0.070). We repeated the model by instead adding one health covariate at a time. We found that the interaction between ACEs and internalizing distress was only non-significant when BMI was included. Given the positive correlation between BMI and latent inflammation (r = 0.43), it is possible that BMI may reflect a similar biological process as the inflammation biomarkers. Subsequently, we examined if transdiagnostic internalizing distress and ACEs similarly predicted BMI. First, the internalizing factor and ACEs were used as main effect predictors for BMI (online Supplementary Table S1). Only ACEs exhibited a positive association with BMI (b = 0.435, p < 0.001, 95% CI [0.169–0.701], β = 0.096); internalizing distress was not significant (b = 0.325, p = 0.429, 95% CI [−0.481 to 1.13], β = 0.024). In the second model step, the ACEs-internalizing interaction term was significantly associated with BMI (b = 0.705, p = 0.004, 95% CI [0.220–1.189], β = 0.051). Johnson-Neyman analyses revealed that a minimum of 3 ACEs was required before a significant positive association emerged between the internalizing factor and BMI. Also, internalizing distress scores needed to be at the 39th percentile before a positive association between ACES and BMI emerged. Thus, we observed a similar moderation effect between transdiagnostic internalizing distress and ACEs when predicting BMI.
We also created two new ACEs subscales focused on abuse and neglect (see online Supplemental Materials). There was a significant interaction between abuse and latent internalizing (b = 0.094, p = 0.003, 95% CI [0.031–0.157], β = 0.137). Abuse predicted inflammation, but only when current internalizing was also elevated. In a separate model, neglect predicted inflammation as a main effect, but the interaction term with latent internalizing was not significant (b = 0.063, p = 0.053, 95% CI [−0.001 to 0.128], β = 0.101). Although the effect sizes are similar, abuse better explained the ACEs total score -by- internalizing moderation effect described above. Online Supplemental Tables S2–S4 summarize results comparing the broad internalizing factor score v. the disorder-specific residuals. The residual of depression did not interact with ACEs to predict inflammation (b = −0.010, p = 0.319, 95% CI [−0.048 to 0.016], β = −0.008), but the interaction between ACEs and broad internalizing remained significant (b = 0.077, p = 0.005, 95% CI [0.022–0.123], β = 0.173). Similarly, the anxiety residual did not significantly interact with ACEs to predict inflammation (b = 0.020, p = 0.281, 95% CI [−0.010 to 0.041], β = 0.015), whereas broad internalizing and ACEs remained significant (b = 0.062, p = 0.042, 95% CI [0.002–0.104], β = 0.140). Lastly, the panic residual did not significantly interact with ACEs to predict inflammation (b = 0.004, p = 0.754, 95% CI [−0.019 to 0.026], β = 0.001), but broad internalizing and ACEs maintained significance (b = 0.071, p = 0.012, 95% CI [0.014–0.108], β = 0.160). In summary, the transdiagnostic internalizing distress dimension was a better predictor of vulnerabilities to ACEs than the disorder-specific residuals of anxiety, depression, or panic.
Discussion
Contrary to previous reports of a simple relationship between early adversity and midlife inflammation, our results revealed that this association depends on transdiagnostic internalizing distress. Within the MIDUS sample, heightened inflammation was best explained when ACEs were also combined with elevations on a broad factor score encompassing past 12-month internalizing symptomatology and trait neuroticism. We also observed that the disorder-specific residuals (MDD, GAD, panic) did not similarly moderate the adversity-inflammation effect.
These results point to the unique biological importance of internalizing comorbidities (DeYoung et al., Reference DeYoung, Blain, Latzman, Grazioplene, Haltigan, Kotov and Tobin2023). Although chronic inflammation across the lifespan may be influenced by adversity, this effect may be at least somewhat conditional on the presence of processes shared across many forms of internalizing psychopathology. There are multiple possible causal sequences that could explain chronic inflammation in this sample. For example, the findings call to mind established models of resilience focused on the individual differences shaping adaptation following adversity (Luthar, Cicchetti, & Becker, Reference Luthar, Cicchetti and Becker2000). Our trait-like rather than state-like index of internalizing and neuroticism may reflect stable vulnerabilities that amplified the long-term impact of adversity. A variety of transdiagnostic individual difference traits related to neuroticism are known to change the impact of stressors such as negative emotionality (Masten et al., Reference Masten, Hubbard, Gest, Tellegen, Garmezy and Ramirez1999), rumination (Abela & Hankin, Reference Abela and Hankin2011), and maladaptive cognitive appraisal patterns (Hankin, Abramson, & Siler, Reference Hankin, Abramson and Siler2001). Similar processes may have led to maladaptive stress responses among these MIDUS participants. Given the cross-sectional design, the extent to which features of internalizing distress were also present during childhood is unknown. It is possible adult internalizing distress is a continuation of the vulnerabilities present at the time of early stressors (Hilsman & Garber, Reference Hilsman and Garber1995), which had long-term consequences on inflammation starting in childhood. It is also possible that current internalizing distress reflects ongoing impairments in stress regulation, which may be contributing to difficulties with managing responses to lingering psychological sequelae of past childhood adversity (e.g. intrusive reexperiencing; Ehlers and Steil, Reference Ehlers and Steil1995). There is a need for additional prospective research to explore the longitudinal dynamics of these effects and determine whether pre- adversity internalizing distress is a true vulnerability for adversity-inflammation associations.
In contrast to a vulnerability hypothesis, a sensitization model highlights an alternative way ACEs together with internalizing may chronically exacerbate inflammation. Early adversity has a privileged role in shaping biological functioning, which can potentially sensitize reactivity to stressors later in life (Hostinar et al., Reference Hostinar, Lachman, Mroczek, Seeman and Miller2015; Miller, Chen, & Parker, Reference Miller, Chen and Parker2011). For instance, people who experienced childhood maltreatment can exhibit exacerbated acute inflammatory activity when exposed to present day stressors (Carpenter et al., Reference Carpenter, Gawuga, Tyrka, Lee, Anderson and Price2010). Transdiagnostic internalizing psychopathology is a stressor because it disrupts role functioning and impairs quality of life. Consistent with this idea, Miller and Cole (Reference Miller and Cole2012) demonstrated that the onset of depressive symptoms among adult women was associated with more inflammation in those with childhood adversity. It is possible the immune response in people with ACEs has been sensitized to stress, which has led them to experience the impairment of internalizing psychopathology differently. Future studies of the inflammatory cascade may benefit from measurement approaches designed to tease apart the specific effects of current psychopathology v. the disability-related consequences of psychopathology.
For our second aim, we directly compared transdiagnostic and disorder-specific features of psychopathology. Inflammation was most closely associated with clinical symptomatology spanning across internalizing disorder measures. Therefore, the intercorrelations between internalizing symptoms and trait neuroticism were more than just a statistical phenomenon – these transdiagnostic associations best explained chronic inflammation following childhood adversity even when directly competing against symptoms specific to depression, anxiety, and panic. This finding provides a path toward synthesizing associations between various individual psychiatric diagnoses and inflammation (Duivis et al., Reference Duivis, Vogelzangs, Kupper, de Jonge and Penninx2013; Hoge et al., Reference Hoge, Brandstetter, Moshier, Pollack, Wong and Simon2009; Michopoulos et al., Reference Michopoulos, Powers, Gillespie, Ressler and Jovanovic2017; Ogłodek et al., Reference Ogłodek, Szota, Just, Szromek and Araszkiewicz2016; O'Donovan et al., Reference O'Donovan, Hughes, Slavich, Lynch, Cronin, O'Farrelly and Malone2010; Wagner et al., Reference Wagner, Wagner, Glaus, Vandeleur, Castelao, Strippoli and von Känel2015). This is also thematically consistent with other studies of general health outcomes, which demonstrate stronger associations with broad internalizing than individual disorders (Eaton et al., Reference Eaton, Krueger, Keyes, Wall, Hasin, Markon and Grant2013; Kim et al., Reference Kim, Turiano, Forbes, Kotov, Krueger and Eaton2021; van de Pavert, Sunderland, Luijten, Slade, & Teesson, Reference van de Pavert, Sunderland, Luijten, Slade and Teesson2017). By explicitly modeling comorbidities, our study demonstrates how transdiagnostic markers can help reveal stronger and more cohesive statistical associations with biological systems (DeYoung et al., Reference DeYoung, Blain, Latzman, Grazioplene, Haltigan, Kotov and Tobin2023; Zald & Lahey, Reference Zald and Lahey2017).
There is value in considering why the moderation effect between ACEs and internalizing distress becomes non-significant after covarying for BMI. Elevated BMI is typically associated with higher adipose fatty tissue concentrations (de Heredia, Gómez-Martínez, & Marcos, Reference de Heredia, Gómez-Martínez and Marcos2012). Inflammatory markers such as IL-6 and CRP are synthesized in response to signaling molecules released through adipose tissue (Ouakinin, Barreira, & Gois, Reference Ouakinin, Barreira and Gois2018). Moreover, research has established a bidirectional relationship between adipose tissue and clinical depression (Shelton & Miller, Reference Shelton and Miller2011). BMI may promote inflammation through similar underlying processes as internalizing psychopathology (e.g. activation of endocrine systems). Therefore, covarying for variables like BMI when predicting inflammation may remove meaningful variance (Slopen, Koenen, & Kubzansky, Reference Slopen, Koenen and Kubzansky2012). Notably, associations among internalizing conditions, inflammation, adverse childhood experiences, and BMI are frequently observed consistent with a shared pathophysiological process (Lamers, Milaneschi, de Jonge, Giltay, & Penninx, Reference Lamers, Milaneschi, de Jonge, Giltay and Penninx2018). BMI may indirectly mediate the relationship between early adversity, adult internalizing, and adult inflammation (Palmos et al., Reference Palmos, Watson, Hughes, Finkelmeyer, McAllister-Williams, Ferrier and Powell2019). Continuing examination of physiological contributors to chronic inflammation could improve our understanding of the underlying mechanistic pathways linking early adversity and internalizing distress.
This study has several limitations that point to important future directions of research. Although we used established methods for analyzing MIDUS inflammatory data (Elliot & Chapman, Reference Elliot and Chapman2016; Friedman & Herd, Reference Friedman and Herd2010; Sheffler et al., Reference Sheffler, Piazza, Quinn, Sachs-Ericsson and Stanley2019; Slopen et al., Reference Slopen, Lewis, Gruenewald, Mujahid, Ryff, Albert and Williams2010), alternative approaches have been proposed. Representing inflammation as a latent construct involves measurement trade-offs. Aggregating multiple indicators together could mask genuine associations specific to particular inflammation indices (Moriarity & Alloy, Reference Moriarity and Alloy2021). It is also possible that replacing extreme inflammatory values removed some relevant information (Moriarity, Reference Moriarity2022). Prior work has shown that baseline inflammation may lead to subsequent depressive symptoms (Valkanova, Ebmeier, & Allan, Reference Valkanova, Ebmeier and Allan2013), but the opposite has also been observed (Copeland, Shanahan, Worthman, Angold, & Costello, Reference Copeland, Shanahan, Worthman, Angold and Costello2012; Glaus et al., Reference Glaus, Vandeleur, von Känel, Lasserre, Strippoli, Gholam-Rezaee and Preisig2014; Zainal & Newman, Reference Zainal and Newman2022). Due to the cross-sectional nature of the data, causality is difficult to determine, although the literature suggests some form of a bidirectional phenomenon. Recall of early adversity can be influenced by current distress (Martin-Wagar et al., Reference Martin-Wagar, Marquardt, Liu, Arbisi, Erbes and Polusny2024), which can result in substantially different associations between retrospective and prospective measures of ACEs (Colman et al., Reference Colman, Kingsbury, Garad, Zeng, Naicker, Patten and Thompson2016; Hardt & Rutter, Reference Hardt and Rutter2004). Studies of past adversity based solely on retrospective measures face challenges when trying to distinguish between current distress and ACEs. Race may also function as a proxy for adversity. Therefore, it is difficult to disentangle these relationships using cross-sectional designs. This was a motivating factor for using hierarchical models with and without covariates. Lastly, the CTQ, which contributed to our ACEs measure, has known limitations. These include a lack of cross-cultural considerations and variability in internal consistency across studies (Georgieva, Tomas, & Navarro-Pérez, Reference Georgieva, Tomas and Navarro-Pérez2021).
In conclusion, a latent factor reflecting past 12-month internalizing distress symptoms and trait neuroticism moderated the relationship between ACEs and midlife inflammation. Therefore, assessment of early adversity and internalizing distress in isolation appears to be insufficient – it was important to consider both together to capture the long-term inflammation effects more fully within the MIDUS sample. In addition, this transdiagnostic factor was a better predictor than disorder-specific facets of depression, anxiety, and panic. Given the growing research base validating transdiagnostic approaches for studying health outcomes, clinicians should be encouraged to also incorporate transdiagnostic symptom measures in their practice (Ruggero et al., Reference Ruggero, Kotov, Hopwood, First, Clark, Skodol and Zimmermann2019). Such assessments may reveal opportunities for intervention, which could shape the long-term physical health trajectories of patients with ACEs.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724002265
Funding statement
This material was supported with resources and the use of facilities at the Minneapolis Veterans Affairs (VA) Health Care System, Minneapolis, Minnesota. ZSM was supported under VA ORD CSR&D grant CX002221-01A1. RFK was supported partly by National Institutes of Health grants R01AG053217, R01AG077742, and U19AG51426. Publicly available data from the MIDUS study was used for this research. Since 1995, the MIDUS study has been funded by the following: John D. and Catherine T. MacArthur Foundation Research Network, National Institute on Aging (P01-AG020166), and National Institute on Aging (U19-AG051426). Biomarker data collection was further supported by the NIH National Center for Advancing Translational Sciences (NCATS) Clinical and Translational Science Award (CTSA) program as follows: UL1TR001409 (Georgetown), UL1TR001881 (UCLA), and 1UL1RR025011 (UW). The content is solely the responsibility of the authors and does not necessarily represent the official views or policy of the U.S. Department of Veterans Affairs. The authors thank Drs. Camelia Hostinar and Daniel Moriarty for comments and guidance on earlier versions of this report.








