Since the emergence of COVID-19, there remains limited insights on healthcare personnel (HCP) perceptions and barriers to personal protective equipment (PPE) use and guidance in ambulatory settings. While most guidelines focus on direct application of transmission-based precautions developed in inpatient settings, outpatient implementation poses unique challenges regarding feasibility, resource availability, and HCP burden. Reference Houghton, Meskell and Delaney1–Reference Kim, Park and Choi5 Walk-in clinics (WIC), urgent care and primary care clinics are often the first point of medical contact by patients seeking evaluation for respiratory viral illnesses, underscoring the need to understand ambulatory HCP knowledge, perceived challenges to compliance and awareness of current PPE guidelines.
Transmission-based precaution guidelines for suspected or confirmed cases of COVID-19 per the Centers for Disease Control and Prevention in any healthcare setting, including ambulatory, recommend airborne, contact and eye protection (N-95 mask, gown and gloves, face shield or goggles). 6 This pilot was conducted in WICs to evaluate HCP perspectives on benefits and challenges of a system to identify patients with suspected or confirmed COVID-19 upon check-in and guideline-directed PPE use.
Methods
The pilot occurred in four WICs across a large academic medical center from July-October 2024. Participation by HCP was voluntary. HCP at selected WICs were sent an electronic link to complete an anonymous, voluntary REDCap survey to evaluate attitudes, knowledge and challenges to comply with PPE guidance, pilot educational resources, technology tools (symptom check-in list to identify potential COVID-19 cases which trigger a flag on Epic® and provider dashboards), and clinical workflow impacts. Educational Power Point slides illustrated how to navigate Epic® flag notifications for PPE and reviewed transmission-based isolation precautions for COVID-19. Survey responses were scored using a 5-point Likert scale with an optional feedback section.
Results
The survey response rate was 53.1% (N = 26/49). Respondent roles were predominantly Licensed Practical Nurse (8, 30.8%), patient service specialists (7, 26.9%), or advanced practice providers (4, 15.4%). Groups with two or fewer respondents included physicians, X-ray technologists, medical assistants and one administrator. Most completed the education before the pilot began (21, 80.8%).
Most HCP deemed the educational materials, Epic® tools and support from the infection prevention team, predominantly on-site, as helpful (Table 1). Respondents strongly agreed that PPE increased the time required per patient encountered and burden to HCP. Though HCP could easily identify which patients needed isolation and what PPE to use, most agreed that PPE use made it harder to handle specimens and contributed to excess waste.
Table 1. Healthcare personnel perspectives on isolation precautions pilot resources and workflow impacts in WICs – REDCap survey results
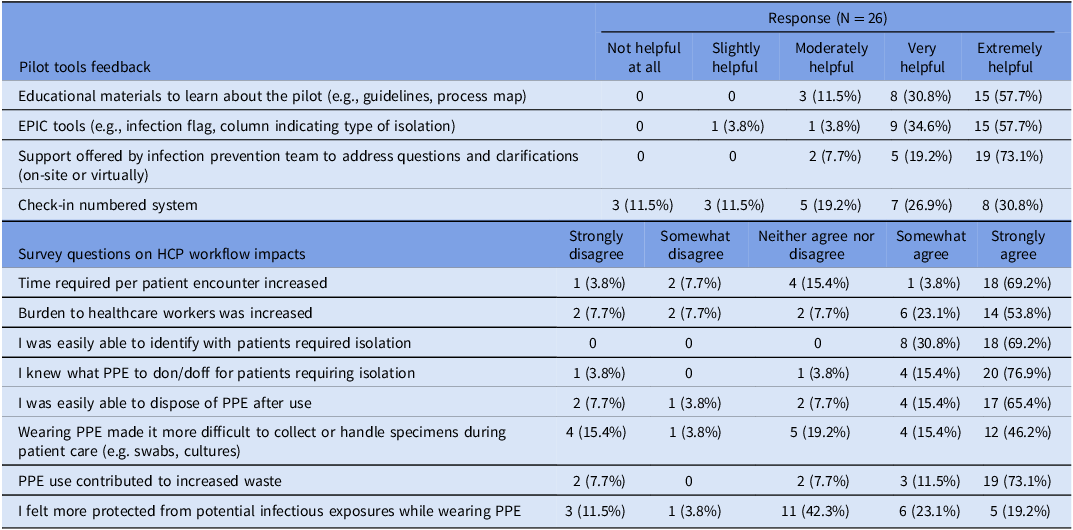
HCP respondents were asked to: 1) evaluate the following tools used in the project on how helpful they were to learn about the processes for isolating patients in the outpatient clinic, 2) indicate their level of agreement or disagreement with statements evaluating workflow impacts during participation in the pilot.
Among voluntary feedback responses, HCP appreciated that tools raised awareness of potentially contagious patients via the Epic® alert. HCP felt more protected while masking but noted several impediments to PPE affecting workflow including difficulty to reliably don and doff with high patient turnover rates, specimen handling issues, waste, and limited clinical relevance during encounters with minimal patient contact.
Discussion
Ambulatory challenges to comply with COVID-19 PPE in this survey of WIC HCP highlight perceived workflow impediments and variable views on the protective effect despite high rates of PPE knowledge and improved access. Heightened awareness has been positively associated with nursing PPE compliance in COVID-19, reinforcing the benefits of developing tools to equip HCP with knowledge and convenient access to PPE. Reference Min, Moon, Jang, Cho, Jeon and Sung4,Reference Kim, Park and Choi5 The pilot symptom-based screening approach with electronic flags enabled clinic teams to better identify potentially contagious patients, isolate earlier and mitigate exposure risks. PPE compliance monitoring by infection control staff has also been found to encourage adherence. Reference Brooks, Greenberg, Wessely and Rubin7
Interestingly, survey responses were mixed regarding whether HCP felt more protected wearing PPE. This appears to be a shift from attitudes early in the pandemic when most HCP deemed PPE to be at least moderately protective. Reference Green-McKenzie, Shofer, Lappin, Cohen, O’Connor and Kuter8 Personal risk calculation by HCP also impacts motivation for PPE adherence, including fear of infecting family or close contacts with high-risk medical conditions. Reference Houghton, Meskell and Delaney1 It is unclear if the relative overall neutral stance to this question reflected HCP self-determination of low risk (e.g., from vaccination, infection with COVID-19, or short clinical encounters).
PPE must be easily accessible to frontline providers to prioritize safety and compliance, reflected by survey feedback about opportunities to expand PPE access. PPE shortages experienced early in the pandemic were a prominent barrier to use and risk to HCP. Reference Houghton, Meskell and Delaney1,Reference Badran, Jarrah and Masadeh2 Associated significantly increased odds of burnout also risked HCP retention. Reference Green-McKenzie, Shofer, Lappin, Cohen, O’Connor and Kuter8 Future infection surges are expected to further strain staffing, clinic capacity and PPE resources, exacerbating workflow burdens and jeopardizing compliance. Healthcare systems serving higher volumes or complexity of patients, with fewer resources, may be more vulnerable to lapses in PPE adherence.
Limitations of this analysis include the small number of respondents in a single healthcare system. The pilot occurred during a low incidence period of COVID-19, which may have reduced concern by HCP for personal exposure risk and contributed to stronger sentiments toward PPE burdens. Though this survey did not assess individual components of PPE, based on voluntary feedback received, responses may have reflected the limited perceived benefits of contact precautions more so than masking. While the survey did not address availability of negative pressure or isolation rooms, these resources are rare commodities in ambulatory settings, emphasizing the importance of PPE to reduce exposure risk. Reference Houghton, Meskell and Delaney1
Successful adaptation of transmission-based isolation protocols for patients with acute respiratory infections in ambulatory sites requires understanding HCP experiences with PPE. Differences between ambulatory and inpatient environments in resource availability, capacity and infrastructure may translate as site-specific barriers to compliance and safety. Identifying these distinctions can be leveraged to improve frontline clinic PPE availability, implement screening tools, tailor education, and promote partnership with infection prevention teams to mitigate risks of communicable disease transmission.
Acknowledgements
The infection prevention team thanks HCP at participating WICs.
Financial support
Institutional funds.
Competing interests
Dr. Talbot serves on the board of directors for OmniSolve. All other authors report no conflicts of interest relevant to this article.




