Introduction
The cause of chylothorax is either traumatic or non-traumatic. Non-traumatic chylothorax is often challenging to treat and may be fatal. Reference Resch, Sever Yildiz and Reiterer1 There are some reports of the effectiveness of etilefrine in traumatic chylothorax in adults and children, Reference Guillem, Billeret, Houcke and Triboulet2,Reference Muniz, Hidalgo-Campos, Valdivia-Tapia, Shaikh and Carreazo3 but its effectiveness in non-traumatic chylothorax is unclear. Although the use of etilefrine in combination with pleurodesis or octreotide for idiopathic chylothorax has been reported, Reference Tomobe, Mizuguchi, Shimotakahara, Shimojima and Okazaki4,Reference Kinoshita, Shoya, Shimotakahara, Hataya and Saito5 but there are no reports on the effectiveness of etilefrine alone. Here, we report the effectiveness of etilefrine treatment for refractory non-traumatic chylothorax in a patient with Noonan syndrome. Dietary therapy, octreotide, prednisolone, lymphatic embolisation, and lymphatico-venous anastomosis were all ineffective.
Case report
A boy aged 2 years and 8 months with Noonan syndrome with RIT1 mutation presented with a right pleural and pericardial effusion (Fig 1a). He had undergone right ventricular outflow tract reconstruction due to severe pulmonary valve stenosis at the age of 6 months and was receiving regular follow-ups. Oral diuretics were started on admission. Because there was only a slight improvement, a right chest tube was inserted on day 2 of admission, resulting in the drainage of 95.1 mL/kg of pleural fluid on that day. Pleural fluid examination results were as follows: total protein 4.3 g/dL, lactate dehydrogenase 115 U/L, triglycerides 1215 mg/dL, and white blood cell count 13.4 × 103 /µ, 100% of which are lymphocytes. Additionally, serum total protein was 6.9 g/dL, serum lactate dehydrogenase was 215 U/L, and serum triglycerides were 210 mg/dL. Chylothorax was diagnosed on the basis of these findings. Echocardiography on admission revealed a normal left ventricular ejection fraction (71%), a round shape of the ventricular septum, indicating normal right ventricular systolic pressure, a normal systolic excursion of the tricuspid annular plane (12.6 mm), and a very mild increase in peak pulmonary artery flow velocity (1.7 m/s). There was no stenosis of the superior vena cava or dilatation of the inferior vena cava. Cardiac catheterisation was not performed due to the absence of hepatomegaly and only a very mild increase in brain natriuretic peptide level (21.9 pg/mL). Prednisolone (2 mg/kg/day) and low-fat diet therapy with medium-chain triglyceride milk were started, but the drainage volume was 5–20 mL/kg/day. Therefore, continuous administration of octreotide was initiated on day 7 of admission, and the dose was gradually increased to 10 μg/kg/h.
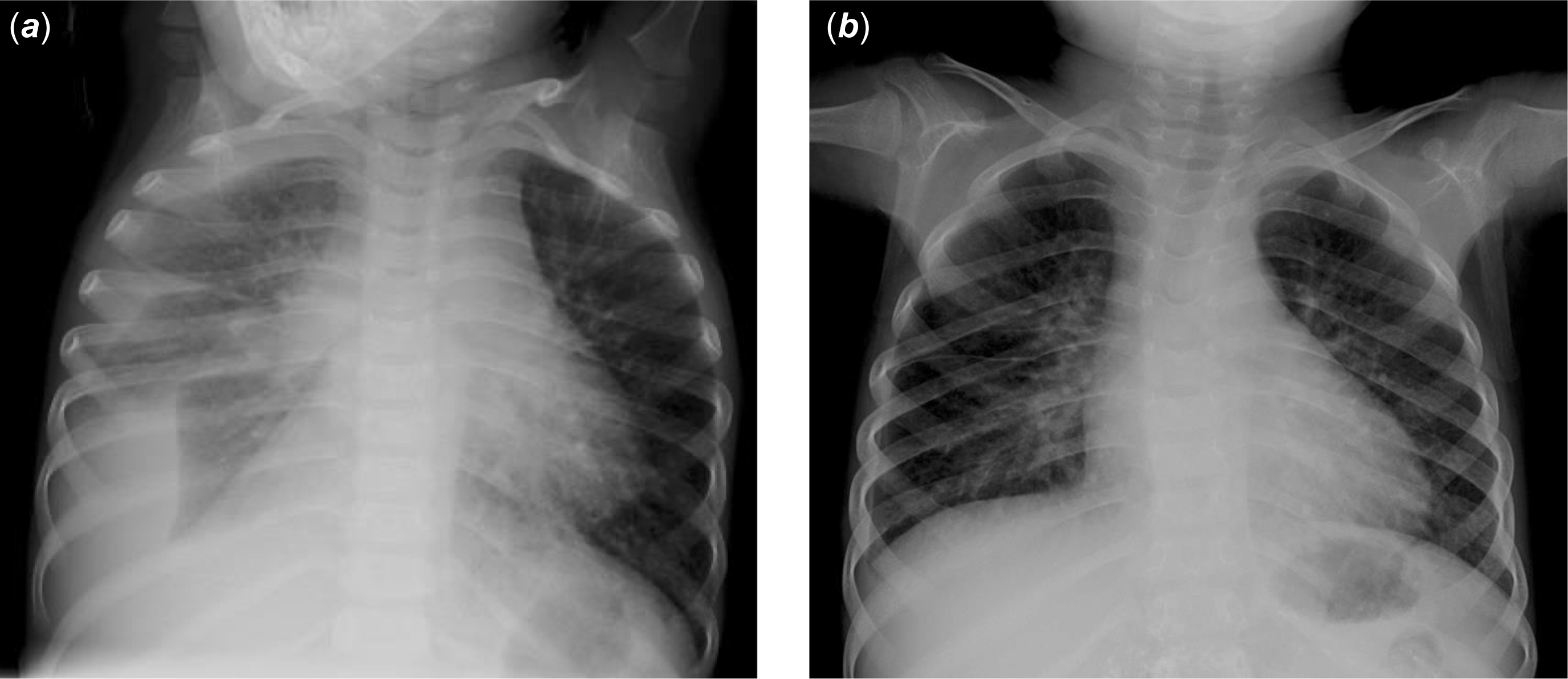
Figure 1. ( a ) chest X-ray at the time of admission. A large volume of pleural fluid is present in the right pleural cavity. ( b ) chest X-ray at 1 month after discharge. There is no pleural effusion.
Despite these treatments, the drainage volume remained at approximately 10–20 mL/kg/day. Injection of indocyanine green into the subcutaneous tissue of the lower extremity revealed indocyanine green leakage into the thoracic cavity, suggesting that the chylothorax was related to abnormal lymphatic flow pathways from the lower extremities to the thorax. Thus, invasive treatment with lymphangiographic embolisation and lower limb lymphatico-venous anastomosis was performed on day 40. During this procedure, the lymphatic vessels supplying the right and left inguinal lymph nodes were microsurgically anastomosed to the femoral vein. CT imaging immediately after lymphangiography demonstrated contrast enhancement in lymph nodes and lymphatic vessels extending from both inguinal regions to the retroperitoneum and parts of the thoracic duct but did not identify the site of chyle leakage. These findings do not definitively indicate that this patient had structural abnormalities of the lymphatic system. However, non-ionic iodinated contrast medium administered from the left upper limb was observed to reflux from the left venous angle into the thoracic duct. Since the thoracic duct is not normally visualised on contrast-enhanced CT in healthy individuals, this suggests that the valve of the thoracic duct may be incompetent. Therefore, lymphatic abnormalities were suspected in this patient, as in other individuals with Noonan syndrome. Reference Sleutjes, Kleimeier, Leenders, Klein and Draaisma6 Subsequently, the drainage volume decreased to approximately 5 mL/kg/day, so the right chest tube was clamped on day 61 and removed on day 68. However, X-ray imaging showed a gradual increase in pleural effusion, and a right chest tube was reinserted on day 83. Because the drainage volume remained at 10–15 mL/kg/day, a second lymphangiographic embolisation and lower limb lymphatico-venous anastomosis were performed on day 103. Postoperatively, the drainage volume remained at 10–20 mL/kg/day, with no improvement. The drug regimen was considered ineffective; prednisolone was tapered from day 107, and octreotide was discontinued on day 120.
Etilefrine was started on day 120 at a dose of 0.5 µg/kg/h. The dose was increased to 1.0 µg /kg/h on day 121 and maintained at 2.0 µg/kg/h from day 122. Although the drainage volume did not immediately decrease after starting etilefrine, it decreased to approximately 0–5mL/kg/day from day 129, and etilefrine was discontinued on day 131 (Fig 2). The chest tube was removed on day 132, prednisolone was gradually tapered to 0.3 mg/kg/day on day 134, and the patient was discharged on day 142. No pleural effusion was observed upon radiographic imaging at 1 month after discharge (Fig 1b).

Figure 2. Treatment interventions and changes in pleural fluid drainage volume (black bar) and body weight (grey line) over time. Following insertion of the first chest tube, the drainage volume gradually decreased, but it started to increase at approximately day 22. Lymphangiographic embolisation and lower limb lymphatico-venous anastomosis were performed on day 40. The drainage volume subsequently decreased, and the drain was clamped on day 61 and removed on day 68. However, X-ray imaging showed the reaccumulation of pleural fluid, and the drain was reinserted on day 83. The drainage volume remained unchanged, despite the performance of a second lymphangiographic embolisation and lower limb lymphatico-venous anastomosis on day 103. Etilefrine was initiated on day 120 at a dose of 0.5 µg/kg/h. The dose was increased to 1.0 µg/kg/h on day 121, maintained at 2.0 µg/kg/h from day 122, and discontinued on day 131. The drainage volume decreased significantly shortly thereafter, and the drain was removed on day 132. LG = lymphangiography; LVA = lymphatico-venous anastomosis; PSL = prednisolone.
Discussion
We reported a case where etilefrine was effective in the treatment of non-traumatic chylothorax in a 2-year-old boy with Noonan syndrome in whom dietary therapy, prednisolone, octreotide, lymphangiographic embolisation, and lymphatico-venous anastomosis were ineffective. This is the first report demonstrating the effectiveness of etilefrine alone for treating non-traumatic chylothorax.
Etilefrine is a sympathomimetic drug to treat orthostatic hypotension with positive alpha- and beta-adrenergic effects. The sympathomimetic effect of etilefrine causes the smooth muscle of lymphatic vessels to contract, leading to narrowing of the lumen, which reduces lymphatic drainage (i.e., chylothorax). Reference Guillem, Billeret, Houcke and Triboulet2 While several reports have documented the use of etilefrine in traumatic chylothorax, its application in non-traumatic chylothorax has been limited to combination therapies, such as with pleurodesis (reported by Tomobe et al.) and octreotide (reported by Kinoshita et al.). Reference Tomobe, Mizuguchi, Shimotakahara, Shimojima and Okazaki4,Reference Kinoshita, Shoya, Shimotakahara, Hataya and Saito5 The main side effects are palpitations, headache, nausea, and tremor, with a low incidence rate (0.1–1%) 7 However, its use is contraindicated during the first trimester of pregnancy due to reproductive toxicity observed in preclinical studies. Etilefrine is also relatively inexpensive, comparable in cost to commonly used drugs like adrenaline. Its use in the treatment of chylothorax offers both safety and cost advantages. Therefore, etilefrine may potentially become the standard care for refractory non-traumatic chylothorax, regardless of the cause. The pathogenesis of non-traumatic chylothorax is unknown. However, Resch et al. reported that 29% of patients with congenital chylothorax had associated congenital anomalies (congenital pulmonary lymphangiectasia, pulmonary hypoplasia, lymphatic malformations, and CHD including arteriovenous malformations), Reference Resch, Sever Yildiz and Reiterer1 suggesting the presence of lymphatic system structural abnormalities in patients with non-traumatic chylothorax. Although the relationship between structural abnormalities of lymphatic vessels and smooth muscle function in non-traumatic chylothorax is unknown, functional and structural factors may be involved in non-traumatic chylothorax development.
In our case, the volume of chylothorax decreased 10 days after etilefrine initiation. However, it is possible that the various treatments discontinued or completed before starting etilefrine may have had a delayed effect. In detail, octreotide did not reduce the drainage volume after 114 days of treatment, which is much longer than the average duration of 22 days for congenital chylothorax, Reference Resch, Sever Yildiz and Reiterer1 suggesting that this drug did not contribute to our patient’s improvement. Regarding prednisolone, although there are no reports investigating the time between the start of prednisolone administration and improvement, the use of prednisolone for non-traumatic chylothorax in an 18-month-old child with Noonan syndrome resulted in significant improvement 2 days after treatment initiation, Reference Goens, Campbell and Wiggins8 which was much shorter than the 106 days in our case. As for lymphangiographic embolisation, Hur et al. performed this procedure in 27 cases of postoperative lymphatic leakage (including 3 cases of chylothorax), reporting an improvement in 85% of cases and a median recovery time of 5 days. Reference Hur, Shin and Lee9 Additionally, Weissler et al. reported that the effects of lymphatic venous anastomosis were typically observed 1–2 weeks after the procedure. Reference Weissler, Cho and Koltz10 In our present case, these procedures were performed on days 40 and 103 of admission, and the pleural effusion resolved 26 days after the second procedure. Because the standard period for evaluating the efficacy of these treatments had passed, it is unlikely that lymphangiographic embolisation and lower limb lymphatic venous anastomosis contributed to the chylothorax improvement. This suggests that etilefrine was effective in our case.
This report describes a single case and does not provide definitive evidence of a causal relationship between etilefrine administration and the resolution of chylothorax. However, the clinical course in this case suggests the potential efficacy of etilefrine, and we hope that further case accumulation and future studies will help establish its effectiveness.
Conclusion
Etilefrine may be a treatment option for paediatric chylothorax regardless of the cause.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
The author(s) declare none.





