Highlights
-
• Identified barriers to accessing deep brain stimulation in Canada include geographical distribution of resources, centralization of services, referral pathways, and lack of education around DBS and its indications.
-
• Possible solutions include the use of virtual care, centralized referral pathways, and education programs.
-
• Future research should be directed to determining the true prevalence of candidates for DBS to target above interventions, and improve access to care.
Introduction
From its inception in 1984, the Canada Health Act has maintained the tenets that provincial and territorial health insurance plans must adhere to, including accessibility.1 The unique geography and population distribution of Canada create challenges when assessing the accessibility of health services. As the complexity of healthcare delivery has evolved, concerns have grown about accessibility to critical healthcare services, particularly those requiring significant technological investment.Reference Fezeu, Ramesh, Melmer, Moosa, Larson and Henderson2
One such area with advancing technology is functional neurosurgery, a subspecialty of neurosurgery that involves the use of neurostimulators, implanted devices and modulation of neurological circuits for the benefit of patients with neurological disease (i.e., deep brain stimulation [DBS] for movement disorders including Parkinson’s disease [PD], essential tremor [ET] and primary dystonia).Reference Chen, Tariq and Ashraf3,Reference Lozano, Lipsman and Bergman4 As the field of functional neurosurgery continues to evolve and the population of Canada ages, proper access to DBS is essential. Gaps remain in our understanding of the prevalence of disease, burden of disability and access to care.Reference Memon, Gelman and Melott5
Previously identified barriers to DBS for movement disorders include race,Reference Shirane, Nisson, Moran, Shanker and Palmese6–Reference Pooja, Yen, Miyasaki, Shetty, Sankar and Ba14 gender,Reference Cramer, Do and Palzer7,Reference Watanabe, Morden, Morita and Bruno9,Reference Gupta, Benesh and Sung12–Reference Jost, Strobel and Rizos15 socioeconomic status/insurance status,Reference Shirane, Nisson, Moran, Shanker and Palmese6,Reference Cramer, Do and Palzer7,Reference Watanabe, Morden, Morita and Bruno9,Reference Gupta, Benesh and Sung12,Reference Chan, McGovern, Sheehy and McKhann13,Reference Kim, Yun and Jeon16,Reference Lad, Kalanithi and Patil17 lack of referrals to tertiary centers/movement disorder clinicsReference Zhang, Ramirez-Zamora and Meng18,Reference Falconer, Gow, Whitney, Walters and Rogers19 and geographical distance from tertiary centers.Reference Fasano, Antonini and Katzenschlager20–Reference Okun, Tagliati and Pourfar23 The majority of studies have been conducted in the USA, aside from one retrospective study in EdmontonReference Pooja, Yen, Miyasaki, Shetty, Sankar and Ba14 and one retrospective cohort study utilizing ICES data in Ontario (ON).Reference Crispo, Lam and Le22 Honey et al. conducted the only Canada-wide study to date, a national snapshot of the geographic distribution of DBS services in Canada in 2018, revealing a clear disparity between provinces in terms of access (i.e., excellent access in Saskatchewan (SK) with extremely poor access in Newfoundland and Labrador [NL]).Reference Honey, Malhotra, Tamber, Prud’homme, Mendez and Honey24 What this study did not investigate was the patient’s need for these services to determine equitable access nor identify barriers to access.
There have been no previous attempts to comprehensively analyze access to DBS in Canada, through investigation of the need for these services, matched access and investigation of barriers for patients and practitioners. The literature primarily relies on retrospective surgical data to determine a patient’s ability to access functional neurosurgery; however, this method is limited, in that patients have already overcome existing barriers to receive surgical intervention in many of these studies.
The current study utilizes a mixed methods survey approach to barriers and facilitators to accessing DBS for patients with movement disorders from patient and healthcare provider perspectives. The objectives of this study include the identification of perceptions of stakeholders along the DBS care pathway regarding barriers to efficient access to functional neurosurgery among patients with movement disorders.
Methods
This is a population-based mixed methods survey study. The study was approved by the local university ethics committee, the Hamilton Integrated Research Ethics Board (HiREB #15262).
Survey development
Survey questionnaires were developed in English and French and adapted for each of the stakeholder groups of interest along the patient care pathway (patients, family physicians, neurologists and neurosurgeons). External individuals from each of these groups were consulted in the design of each questionnaire. Questions were based on previously identified barriers to accessing DBS (geography, access to subspecialty services, socioeconomic status, race and gender).
Survey validation
Surveys were piloted with two external individuals from each target group (neurosurgeons, neurologists, family physicians, patients/caregivers, advocacy groups) for clarity and comprehensiveness. These individuals were not included in our study sample. Neurosurgeons and neurologists reviewed all surveys for content validity, while individuals from each stakeholder group reviewed respective surveys for face validity.
Survey administration
Surveys were distributed electronically using an electronic link or QR code via email, newsletters and websites to patients and caregivers through advocacy groups across Canada (Parkinson NL, Parkinson NS, Parkinson QC, Parkinson Canada, International Essential Tremor Foundation and Dystonia Canada). Employees and volunteers of advocacy groups were asked to complete a designated survey as well. Family physicians, neurologists and neurosurgeons in Canada were provided a QR code to respective surveys through an electronic faxing service in Canada, utilizing publicly available physician contact information (Scott’s Info). Additionally, the Canadian Neurological Sciences Federation listed surveys for neurologists and neurosurgeons on their website and newsletter. Finally, publicly available institutional email addresses were used to distribute surveys to neurologists and neurosurgeons in Canada. A total of two faxes and two emails were sent to maximize responses. See Supplementary Material for survey forms and details regarding recruitment.
Statistical analyses
Descriptive statistics were utilized to summarize patient demographics, region, physician years in practice, estimated number of movement disorder patients in practice and estimated number of DBS candidates in the region. We hypothesized that geographic location may predict perceived lack of access to care among all practitioners and patients, in addition to financial barriers with the lack of available DBS implants among functional neurosurgeons. To test this hypothesis, a binary logistic regression analysis was planned to estimate the lack of access to care, adjusting for geographic location, financial barriers, availability of DBS implants and practitioners. In the event of a low response rate, descriptive interpretation was used.
Rurality was assumed for non-responses based on answers to other questions, and answers were amended if the described region did not match the criteria described by the respondent. For example, if the population of the municipality reported by the respondent had a population in keeping with an urban center, but the respondent reported the region as rural, the data was corrected as such.
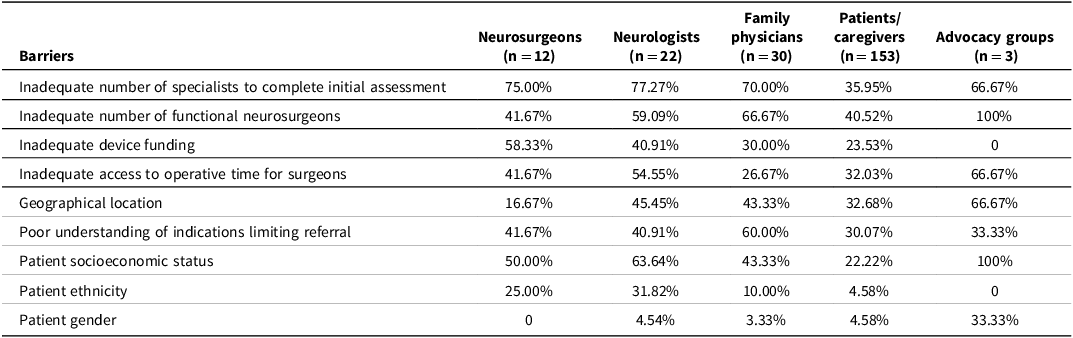
Access was converted to values on a Likert scale (1 = no problem with access; 2 = reasonable access; 3 = poor access; 4 = very poor access) and averaged for each province. Heat maps were produced with open-access software found at heatmapper.ca.
Qualitative themes were extracted from open-ended questions using open coding, utilizing in vivo coding, followed by axial coding and then selective coding to collate codes into potential themes. Themes were refined and named.
Results
A total of 220 responses were obtained from all stakeholder groups surveyed (12 neurosurgeons, 22 neurologists, 30 family physicians, 153 patients and caregivers and 3 directors of advocacy groups). Details of response rates are available in Table 1, with details regarding recruitment strategy and response rates in Figure 1.
Table 1. Response rates among respondent groups
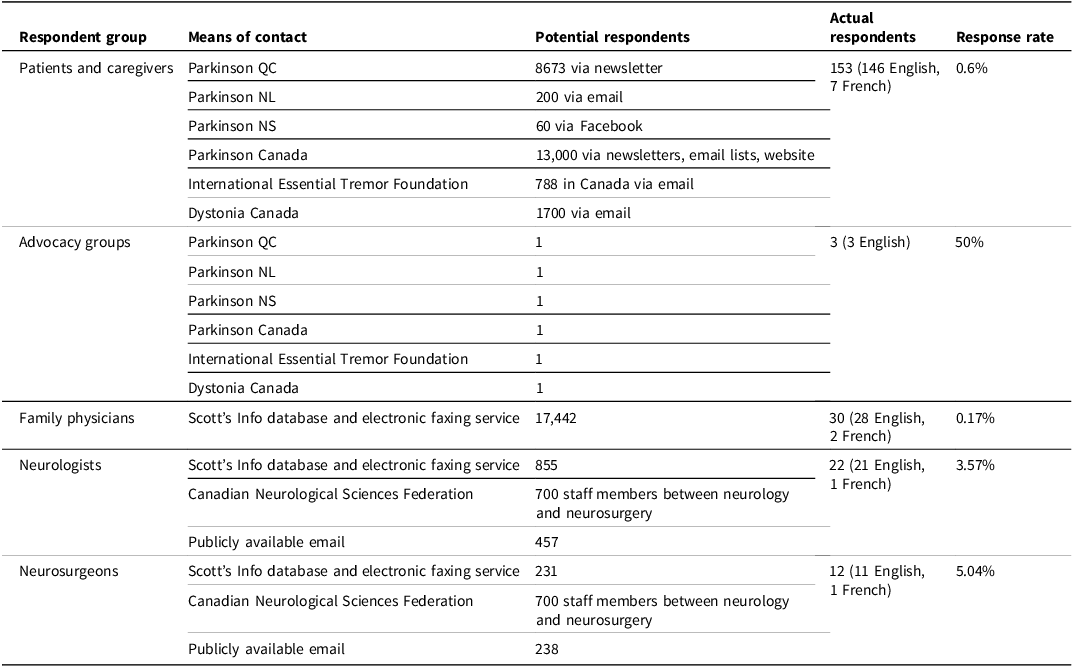
Note: QC = Quebec; NL = Newfoundland and Labrador; NS = Nova Scotia.
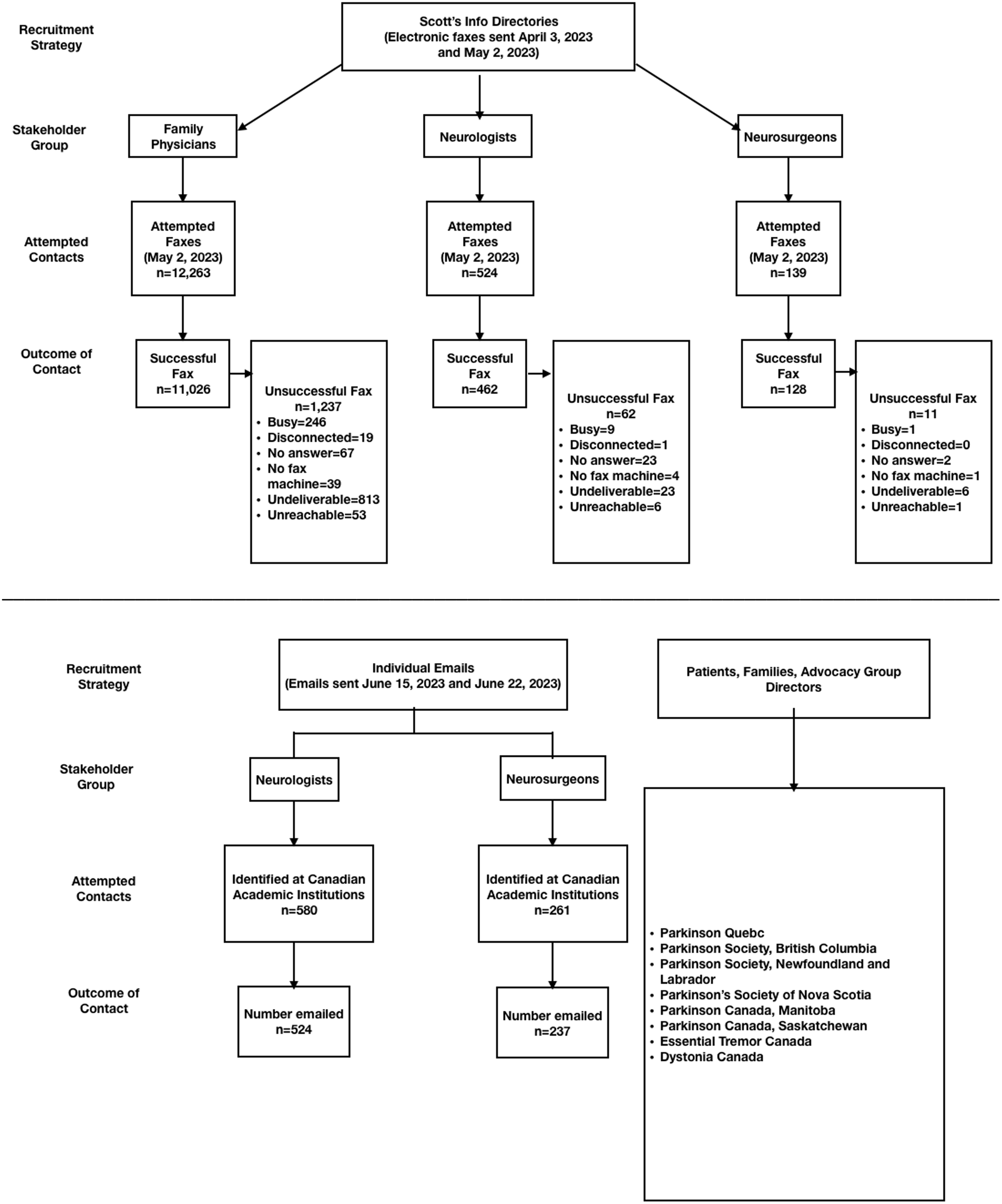
Figure 1. Details of recruitment strategy.
The majority of specialists surveyed practiced in urban areas of ON (n = 46, 71.9%). Of these specialists, three neurosurgeons report performing DBS as part of their practice, and 77.27% of neurologists report referring patients for DBS as part of their practice, with just over half reporting subspecialisation in movement disorders.
Family physicians surveyed commonly reported having a poor understanding of indications for DBS (n = 23, 76.7%). Of those reporting a good understanding of indications (n = 7), when asked to describe the ideal candidate for DBS, no respondents were able to accurately describe a good candidate for the therapy, with some examples including “Parkinson’s disease” and “motor disorders,” without further elaboration. See Table 2 for details of demographics for all surveyed physicians and surgeons.
Table 2. Demographics of physician respondent group

Among surveyed patients/caregivers, 12.42% (n = 15) had previously undergone DBS. These individuals were more frequently living in an urban region in ON (n = 7) or British Columbia (BC) (n = 4) than the rest of Canada. See Table 3 for demographics of included patients/caregivers. Additionally, see Figure 2 for the geographic distribution of patients who had previously undergone DBS in the study population.
Table 3. Demographics of patient and caregiver respondents
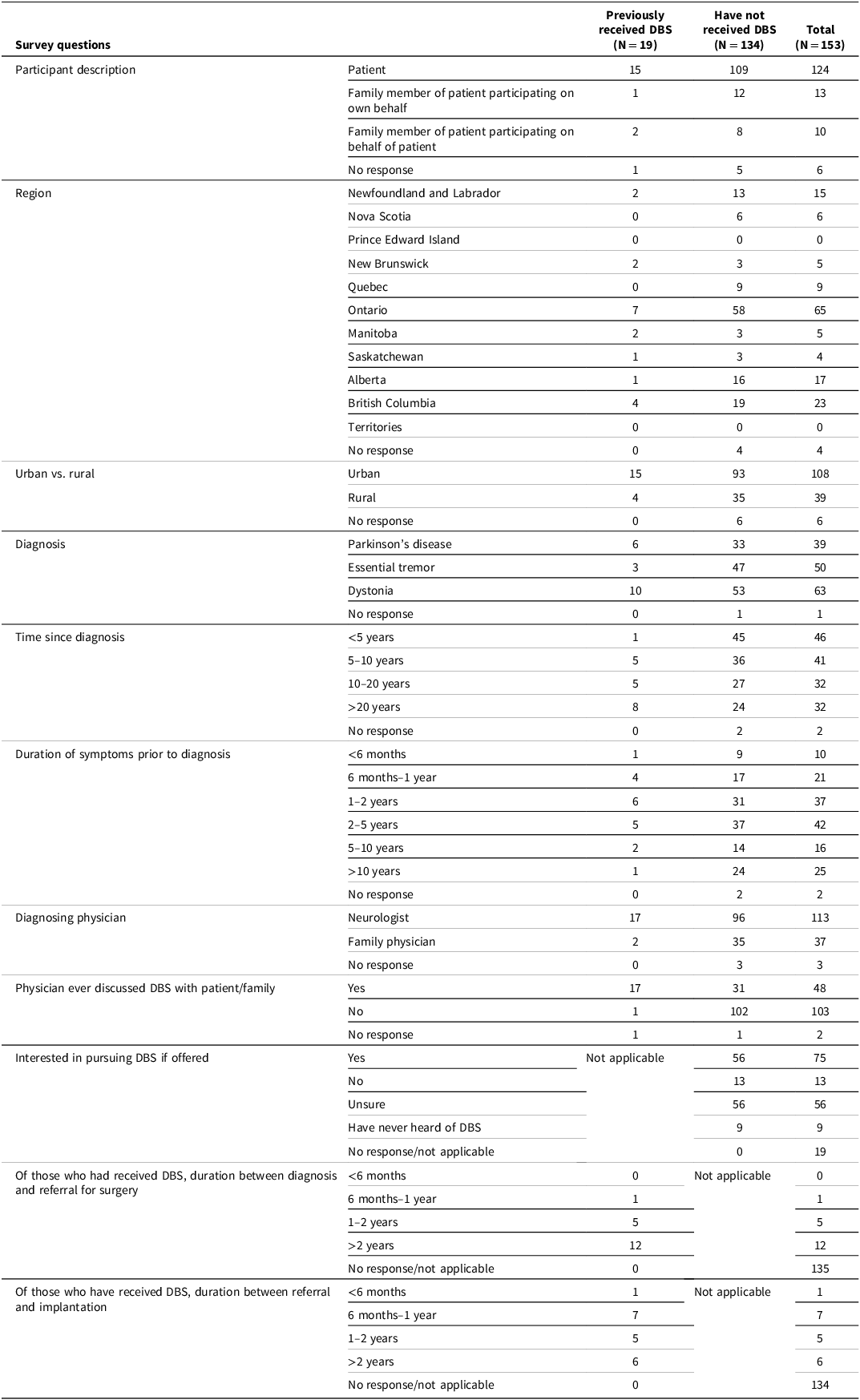
Note: DBS = deep brain stimulation.
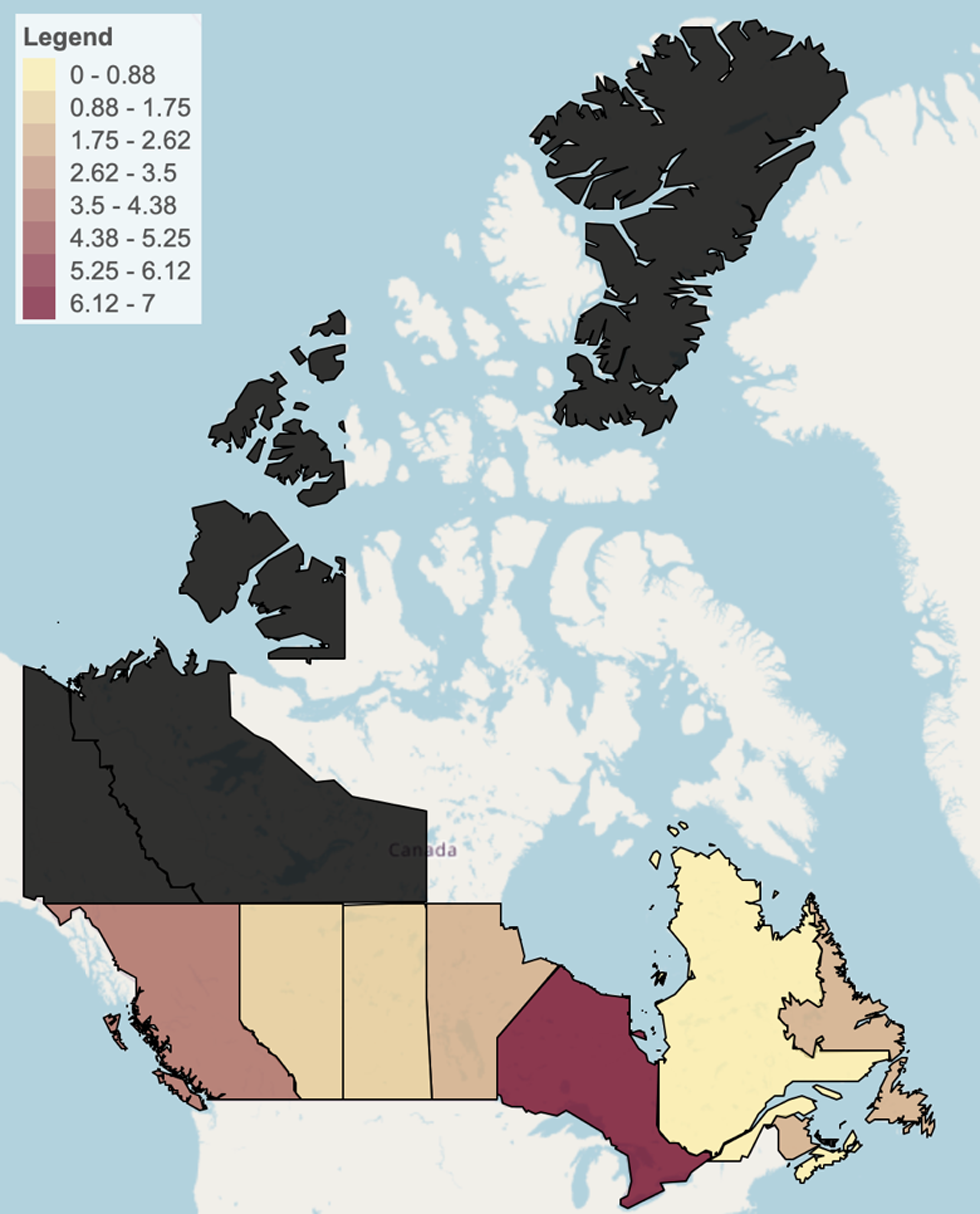
Figure 2. Geographical distribution of patients previously having undergone deep brain stimulation. Shaded black areas represent regions without stakeholder respondents.
The majority of participants in each physician stakeholder group reported either very poor or poor access to DBS in their region (n = 46, 71.9% of all physician respondents). Of included patients and caregivers, 35.29% (n = 54) reported very poor access to this service. See Figure 3 for details of perceived access by stakeholders.
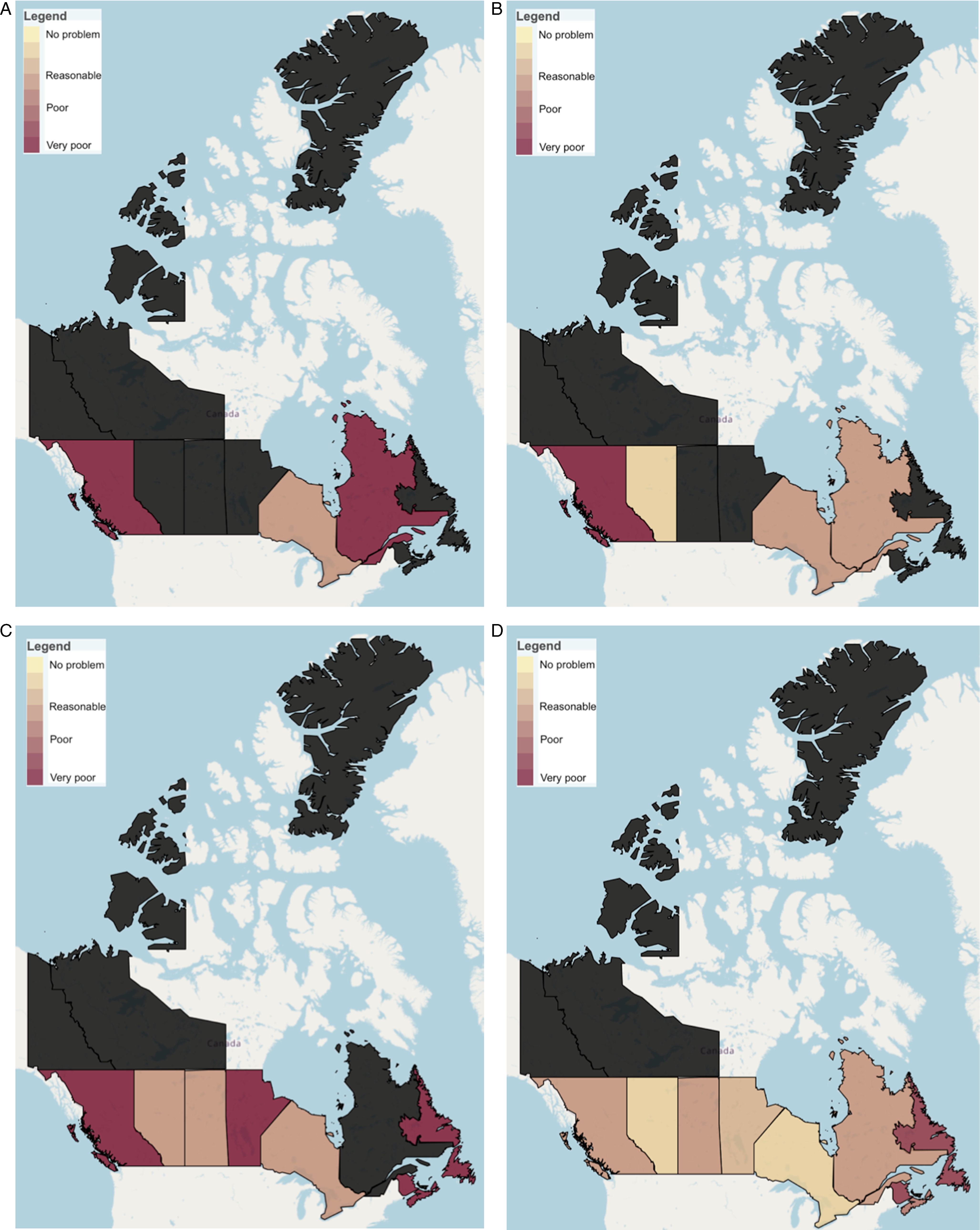
Figure 3. Perceived access to deep brain stimulation across Canada by respondent group. (A) Perceived access by neurosurgeon respondents; (B) perceived access by neurologist respondents; (C) perceived access by family physician respondents; (D) perceived access by patient and caregiver respondents. Shaded black areas represent those without stakeholder respondents for each group.
Perceived barriers to access
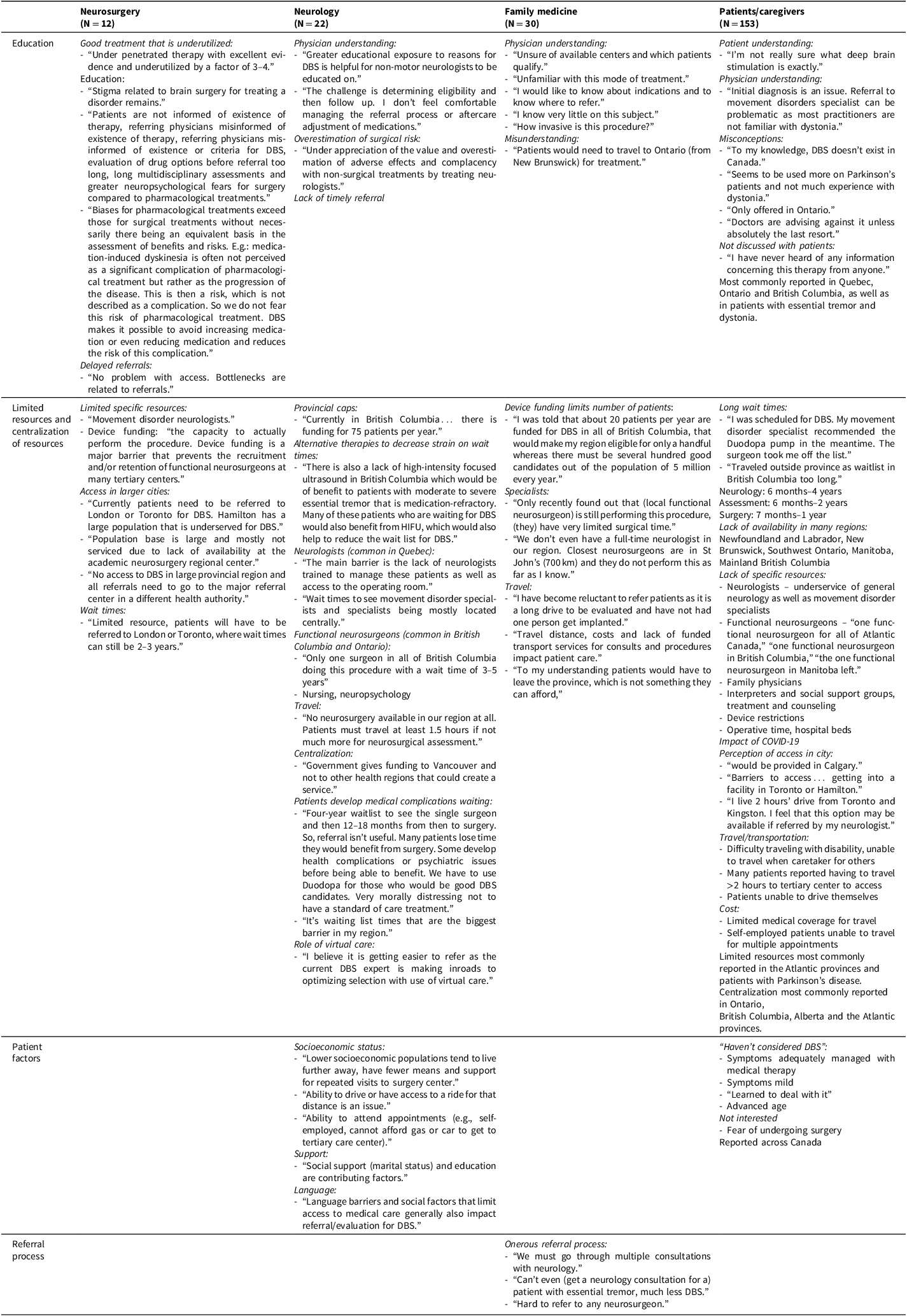
The most commonly reported perceived barrier across all physician groups was an inadequate number of specialists to complete initial assessments. This was a commonly reported perceived barrier among advocacy groups as well.
Another commonly reported perceived barrier among neurologists, family physicians and patients and caregivers was an inadequate number of functional neurosurgeons. Patients in ON and BC more frequently reported access to subspecialist care (both functional neurosurgery and movement disorder neurologists) as a perceived barrier than Atlantic Canadian patients and caregivers, who most commonly perceived geographic location as a barrier to access.
Geographical location was reported as a barrier by 43.33% of family physicians surveyed (n = 13). This differed by region, in that all family physicians in NL reported geographical location as a barrier. Geographical location was reported as a barrier by 45.45% of neurologists and only 16.67% of neurosurgeons. Again, all specialists surveyed reported practicing in urban areas.
Specialists did not commonly perceive poor understanding as a barrier to referral (40.90% of neurologists and 41.67% of neurosurgeons). However, family physicians frequently reported a lack of understanding of indications for DBS themselves, and 60% of family physicians surveyed did report a lack of understanding as a barrier to patient access to DBS. The majority of ON family physicians reported this factor as a barrier.
In terms of cultural and socioeconomic patient factors, socioeconomic status was the most commonly reported barrier among all groups surveyed (neurosurgery 50%; neurology 63.64%; family medicine 43.33%; patients/caregivers 22.22%; advocacy groups 100%).
Ethnicity and gender were far less commonly reported across all groups, except family physicians from urban areas, who commonly reported ethnicity as a barrier. Gender was uncommonly reported across all groups. See Table 4 for a summary of perceived barriers by stakeholder group.
Table 4. Summary of perceived barriers among respondent groups
Qualitative themes
Four themes emerged from all stakeholders surveyed, including Education, Limited Resources/Centralization of Resources, Patient Factors and Referral Process. Ideas from four of five surveyed groups fit into these themes. See Table 5 for a summary of themes and associated ideas for each group.
Table 5. Summary of qualitative themes among respondent groups
Note: DBS = deep brain stimulation.
An insufficient number of advocacy group responses were available to generate qualitative themes; however, ideas were expressed regarding poor understanding of dystonia as a barrier to accessing treatment, and limited resources and availability of DBS in some regions present physical and financial challenges to patients who require travel to access the service.
Education
All stakeholder groups for which qualitative analysis was possible reported ideas related to the concept of education. Ideas related to education from neurosurgeons include the concept that DBS is a good treatment that is underutilized due to a lack of understanding of the treatment, stigma related to undergoing brain surgery, biases for pharmacological therapy and delayed referrals due to a poor understanding of the existence of this therapy.
Neurologists noted the importance of education around indications and follow-up for these patients for non-movement disorder neurologists and there exists an overestimation of surgical risk, with underappreciation of the value of DBS. This lack of education prevents the timely referral of patients who may be good candidates for DBS.
Family physicians primarily focused on physicians’ understanding and misunderstandings about DBS. For example, many family physicians reported “know(ing) very little on this subject,” being unsure of available centers and indications and the invasiveness of DBS as a therapy. In terms of misunderstanding, family physicians echoed similar statements regarding the uncertainty of the availability of the service. For example, one physician reported that patients in their region (New Brunswick [NB]) would have to travel to ON for DBS; however, the treatment is available nearby in Nova Scotia (NS).
Patients and caregivers discussed patient understanding (i.e., a number of patients reported uncertainty about what DBS is), misconceptions (that DBS is not offered in Canada, or only in ON, and that it is only used as a “last resort”), physician understanding (including delayed diagnosis as a result of unfamiliarity on behalf of physicians) and the fact that DBS is not discussed with patients as a potential therapy. Themes around education were most commonly reported by patients in Quebec [QC], ON and BC, as well as in patients with ET and dystonia.
Limited resources and centralization of available resources
All stakeholder groups for which qualitative analysis was possible reported ideas related to limited resources and centralization of available resources as a barrier to accessing DBS. Neurosurgeons identified ideas related to specific resources, specifically scarcity of movement disorder neurologists and device funding, centralization of access to larger cities and presence of long wait times (reported as 2–3 years).
Ideas shared by neurologists related to this theme can be further broken down into limitations on number of patients/implants available annually, limited access to alternative therapies such as high-intensity focused ultrasound, limited access to specialists (neurologists, functional neurosurgeons), limited operating room availability, limited access to specialized nursing care and neuropsychology and the consequences of centralization of services, including travel, limited funding directed to regions outside of major centers, and long wait lists resulting in medical complications while patients wait for surgical assessment. Neurologists shared that access to DBS may be improved by increasing utilization of virtual care.
Family physicians reported frustration with the limited number of patients that may receive DBS annually per province, that they have referred patients who are not deemed eligible after significant delay and inconvenience to the patients to undergo formal assessment and that they are also reluctant to refer patients given the significant burden of travel required for the initial assessment.
Patients and caregivers reported long wait times, from six months to four years for specialist appointments, a lack of availability in some regions (NL, NB, Southwest ON, Manitoba [MB] and Mainland BC), lack of specific resources in regions (including neurologists, movement disorder specialists, functional neurosurgeons, family physicians, interpreters, social support groups, treatment and counseling, device restrictions, operative time and hospital beds). Additionally, patients and caregivers identified ideas about the impact of COVID-19 on the delivery of functional neurosurgery. Ideas related to the theme of limited resources among patients and caregivers were most commonly reported in the Atlantic provinces and in patients with PD.
In patients and caregivers, ideas relating to centralization of services include the perception of access in larger cities, whether access is truly available or not, the burden of travel and transportation on accessing functional neurosurgery and the cost associated with traveling for appointments. Ideas relating to centralization were most commonly reported in ON, BC, Alberta (AB) and the Atlantic provinces.
Patient factors
Neurologists described a number of patient factors that limit access to DBS on an individual level. Primarily, socioeconomic status in that patients may not be able to travel or obtain transportation for multiple appointments, even if they live close to a major center. This burden is greater in populations who live further away from major centers where DBS is offered. Additionally, social support and language barriers were reported to affect access to DBS for patients.
Patients also cited personal factors as reasons they had not previously considered DBS, including mild symptoms or adequate medical management, advanced age or havingi learned to cope with their disease. Some patients reported no interest in pursuing DBS as they have a fear of undergoing surgery.
Referral process
Family physicians described frustration with obtaining any specialty assessment for their patients, with onerous referral processes for patients living with movement disorders. This was not described for other stakeholder groups surveyed.
See Figure 4 for a summary of barriers across the referral pathway for DBS in patients with movement disorders.
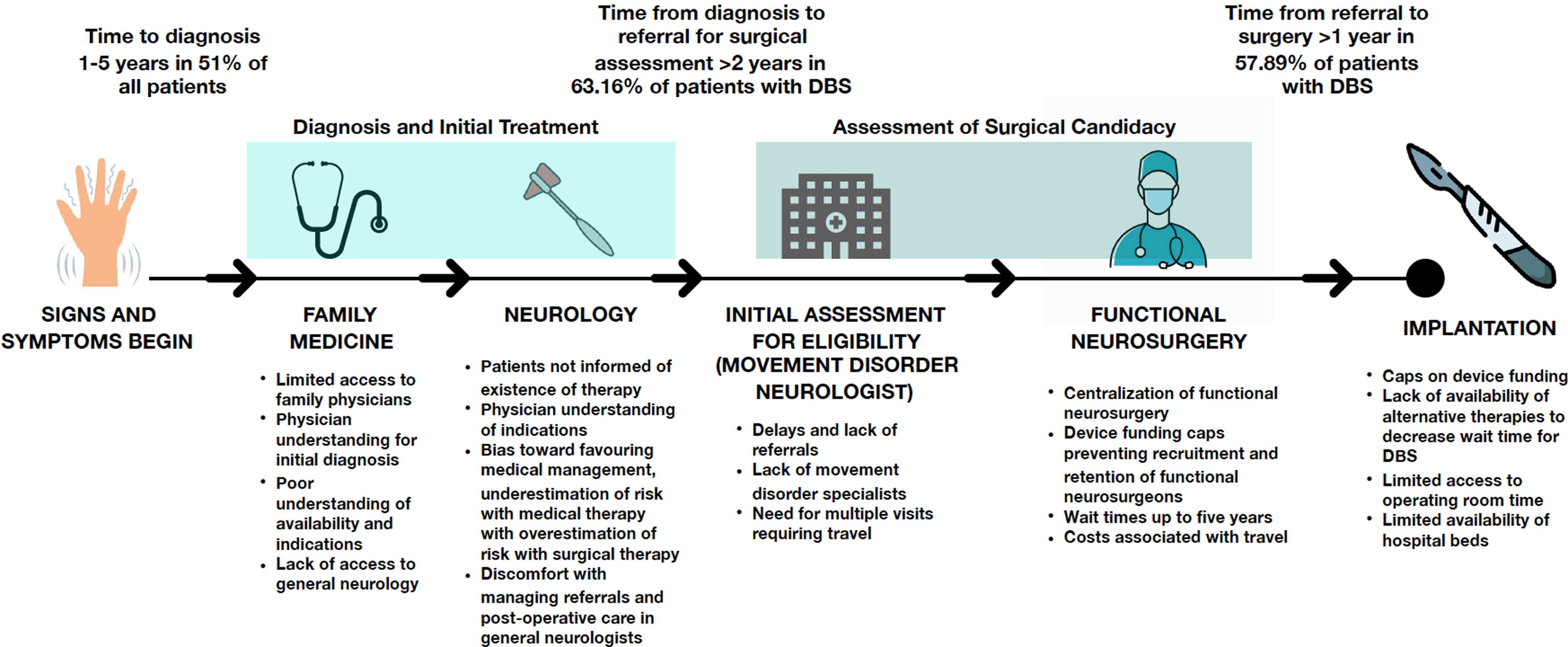
Figure 4. Summary of referral pathway for patients and associated barriers.
Discussion
Previous attempts have been made to describe access to DBS, utilizing retrospective data from patients who have received DBS and attempting to determine what facilitators exist in that population of patients that lead them to be successful in obtaining the service.Reference Shirane, Nisson, Moran, Shanker and Palmese6–Reference Watanabe, Morden, Morita and Bruno9, Reference Chan, McGovern, Sheehy and McKhann13, Reference Pooja, Yen, Miyasaki, Shetty, Sankar and Ba14, Reference Okun, Tagliati and Pourfar23, Reference Sarica, Conner and Yamamoto25 This approach has considerable limitations, as these patients have already overcome barriers to receiving DBS. This study attempts to understand barriers to accessing DBS from a population of primarily potential candidates for DBS and the healthcare providers treating these patients.
Many respondents across all provider groups estimated that less than 10% of referred patients ultimately undergo DBS. However, the four neurosurgeons surveyed who reported performing DBS themselves reported much higher estimations. Neurologists and family physicians more frequently reported lower proportions of referred patients undergoing DBS, but neurologists specializing in movement disorders did more often estimate a higher proportion of patients referred would ultimately undergo surgery. Those more likely to formally assess potential candidates for DBS or ultimately perform surgery are likely more able to estimate that referred patients are implanted. One previous American study found that approximately half of the referred patients for DBS were found to be good candidates for surgery,Reference Katz26 consistent with our findings.
While movement disorder neurologists and functional neurosurgeons were found to estimate the proportion of referred patients who go on to receive DBS more accurately, we proposed that even general neurologists would be better able to estimate this than family physicians or patients, given their patient population. Interestingly, neurologists from the most populous province in Canada (ON) estimated fewer referrals than other regions. Nearly all neurosurgeons surveyed were practicing in ON, with results consistent with those obtained from neurologists. It is therefore possible that there are a greater number of referrals in Western Canada for DBS, even though BC has been reported to have a lower DBS rate compared with the national average (80%), and AB has a similar rate to ON when compared with the national average (120% vs. 126%, respectively).Reference Honey, Malhotra, Tamber, Prud’homme, Mendez and Honey24 It is also possible that neurologists in less populous regions of the province work in a less subspecialized manner, and general neurologists practicing in more remote regions may therefore have a greater number of patients with movement disorders than a subspecialty neurologist in the Greater Toronto Area, who exclusively sees epilepsy patients, for example. This is an area for future work, as poor referral rate was mentioned across physician groups as a barrier to access; therefore, identification of regions with lower referral rates and improving referral patterns may improve access.
Qualitative themes
There was considerable overlap in ideas obtained from all groups. All groups endorsed limited resources and centralization of resources, regarding travel and its associated costs as a barrier to access for patients. Additionally, respondents from every group expressed concerns about long wait times and the impact of a limited number of movement disorder specialists and functional neurosurgeons. All respondent groups also shared similar concerns about the need for education of patients and care providers regarding diagnosis and treatment of movement disorders and the benefits and availability of DBS along with its indications.
In general, concerns regarding travel and lack of resources were more commonly expressed in respondents from Atlantic Canada and patients with PD, although the increased reporting of this concern in patients with PD may be due to the high number of PD patients/caregivers from NL in our study population. Therefore, it may be a reflection of a regional concern as opposed to disease-specific issues.
Concerns with education were more common in Central Canada and BC, as well as patients with ET and dystonia. It is possible that these regions have better access to DBS (or at least the perception of better access), and therefore, individuals are able to identify additional barriers beyond geographic and unavailability of services in their region. These themes may also be more common in ET and dystonia as these diagnoses may be more poorly understood than PD. This is supported by family physician responses, where fewer respondents provided estimates for the prevalence of these two conditions than PD and commonly responded with comments like “I have no idea” when asked about these two diagnoses. See Table 6 for a regional summary of barriers and facilitators to DBS access across Canada.
Table 6. Regional summary of barriers and facilitators to accessing deep brain stimulation
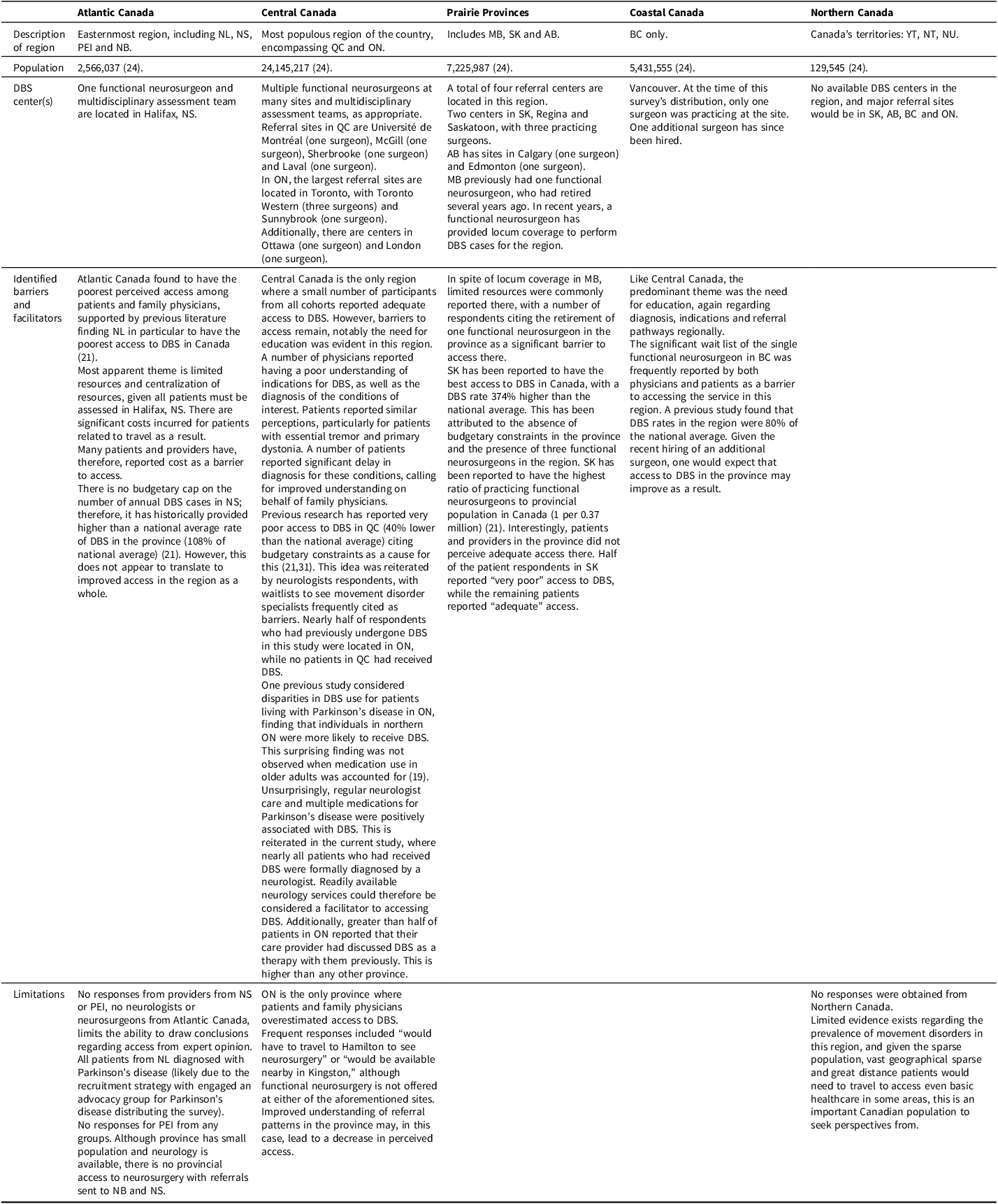
Note: NL = Newfoundland and Labrador; NS = Nova Scotia; PEI = Prince Edward Island; NB = New Brunswick; QC = Quebec; ON = Ontario; MB = Manitoba; SK = Saskatchewan; AB = Alberta; YT = Yukon; NT = Northwest Territories; NU = Nunavut; DBS = deep brain stimulation.
DBS patients surveyed
The included patients who have undergone DBS were not reflective of previously reported access to DBS. For example, 13% of patients receiving DBS in our study were residing in NL, the province that has historically had the poorest access to this service, with one previous retrospective study of all DBS patients in Canada over a two-year period reporting 0.006% of their cohort from NL.Reference Honey, Malhotra, Tamber, Prud’homme, Mendez and Honey24 This overrepresentation from NL may be a result of an enthusiastic PD advocacy group in the region that effectively recruited patients to the study.
Nearly all patients who had received DBS in this study received their formal diagnosis from a neurologist, as opposed to a family physician. It is likely that neurologists have a better understanding of indications and availability of DBS and are therefore more likely to refer appropriate candidates. Literature supports the notion that movement disorder specialists are more likely to refer good candidates for DBS than other providers,Reference Katz26 so access to neurology and specifically movement disorder neurologists is likely an important facilitator.
In terms of the timeline for diagnosis and treatment of these patients, nearly all patients reported being diagnosed more than five years ago, with most being diagnosed more than 20 years ago. Most patients report experiencing symptoms between 1 and 5 years prior to diagnosis. Once diagnosed, the majority of these patients were referred for surgery more than two years after diagnosis and underwent surgery more than six months after referral, with 40% of patients reporting a period greater than two years between patient referral and surgical implantation. Qualitative responses from all groups indicate waitlists of 2–5 years for DBS across Canada. It is unclear at what time patients who received DBS were implanted, so it is possible that delays associated with COVID-19, or any other number of factors, have increased wait list times since these patients underwent surgery. This is one area for future research to determine the duration of waitlists and solutions to decrease surgical wait times for DBS patients.
Proposed solutions
A number of policy changes are required to address access to DBS in Canada, with varying approaches between regions of the country. The first potential solution is increasing resources, including the number of movement disorder specialists and functional neurosurgeons. It should be noted that this could provide a long-term impact; however, time is required for the training of additional specialists that could improve access. This would ameliorate some of the burden of waitlists and, to some extent, travel for individual patients. However, beyond increasing the number of providers in population-dense regions, this would not decrease the burden of travel and expenses for Canadians living in isolated regions of our country, like Atlantic Canada, MB and Northern Canada, where patients must travel long distances for multiple appointments (assessments, surgical bookings, follow-up, reprogramming) and have limited access to emergency neurosurgical care should complications arise. In these cases, increased use of telemedicine may provide improved access to patients. The COVID-19 pandemic necessitated the use of telemedicine for many providers. Available literature suggests telemedicine provides an effective alternative to in-person care for patients living with movement disorders.Reference Falconer, Gow, Whitney, Walters and Rogers19,Reference Fasano, Antonini and Katzenschlager20 Patients were able to access care for surgical assessments and follow-ups and undergo re-programming, all without the inconvenience and costs incurred by traveling. Creation of telemedicine movement disorder clinics throughout the country may be an alternative to current healthcare allocation strategies, to ensure that access to care is improved for all Canadians. Increasing funding to provide travel stipends to patients may alleviate some of the financial burden reported as a barrier to accessing this service as well.
Provincial caps on the number of DBS implants available annually are a previously identified barrier.Reference Honey, Malhotra, Tamber, Prud’homme, Mendez and Honey24 By removing this restriction, SK has the best access in Canada.Reference Honey, Malhotra, Tamber, Prud’homme, Mendez and Honey24 Previous studies have shown that DBS is a cost-effective treatment strategy compared with best medical therapy alone, when considered over the lifetime of implanted patients. DBS has been shown to decrease medication costs, as well as hospitalizations and delay institutionalization of patients living with movement disorders, even accounting for costs of potential complications and hardware replacements.Reference Lannon, Duda and Mastrolonardo27 Therefore, providing increased access to operative time and implants at a provincial level may be a cost-effective approach that could further increase access to this beneficial therapy.
Improved education is required for patients and practitioners regarding the diagnosis of movement disorders, indications for DBS and referral patterns. Among family physicians, 76.7% reported not having a good understanding of indications for DBS, and among the seven family physicians reporting that they did have a good understanding, when asked to describe the ideal candidate for DBS, responses were vague (i.e., “someone with Parkinson’s”) or incorrect, with many family physicians believing that the ideal candidate would be a patient with medically refractory symptoms or that surgery is a “last resort.” These beliefs were reiterated by patient comments that they have been given similar information by physicians. Providing education both to patients and care providers about indications for DBS would help ensure more potential candidates for this efficacious therapy are screened and potentially assessed for DBS. Existing educational resources may improve understanding on behalf of these stakeholder groups. For example, the remote, patient-centered education platform, DBS Select,28 is an educational tool to inform patients and caregivers about DBS. It is continuously updated by a team of neurologists, neurosurgeons and neuroscientists from Belgium and provides an interactive, intuitive web platform to answer many questions patients and their loved ones have. Sharing resources like this with patients upon diagnosis may ameliorate some fear and misunderstanding regarding this treatment.
Previous literature has described the ideal candidate for DBS in PD as having a disease duration of at least five years, allowing atypical forms of parkinsonism to manifest, and they should have a positive response to levodopa (defined as a greater than 30% improvement in Unified PD rating scale motor score), fluctuations, dyskinesia or refractory tremor that remains disabling despite reasonable medical optimization and should not have pre-existing dementia, psychosis or severe depression. Additionally, patients should undergo MRI to rule out secondary diagnoses or structural concerns and should be medically optimized.29 Both patients and family physicians frequently cited age as an exclusion criterion for DBS; however, while evidence suggests younger patients may have improved outcomes, there is no formal age cutoff for the procedure.29 For ET and primary dystonia, patients should have one of these diagnoses with symptoms that interfere with the patient’s quality of life and functionality in spite of reasonable medical management, intact cognition and absence of severe psychiatric illness.Reference Katz26 For all diagnoses, patients should have realistic expectations about what symptoms can be improved by DBS and should have willingness to participate in surgery. With respect to willingness to participate in surgery, few patients reported fear of surgical intervention as a reason they would be unwilling to undergo DBS. The availability of “incisionless” lesioning procedures (i.e., MRI-guided high-intensity focused ultrasound) should also be explained, providing the understanding that these procedures are also invasive with potential complications and cause permanent brain lesions, compared with DBS, where stimulation can be switched off.
Combining the above approaches requires significant collaboration. Although the Canada Health Act stipulates that individual provincial/territorial governments are responsible for overseeing and carrying out the principles of the act in their respective region, national collaboration may be warranted to improve access across Canada. Providing educational resources and clear referral pathways in each region with a regional triage system would ensure that patients residing in provinces/territories without access to this service would have the ability to be referred to a centralized service for their region. For example, a patient living in NL could, in collaboration with their family physician, receive a referral to an expanded virtual movement disorder assessment clinic in Halifax, responsible for screening and triaging patients to determine if a more comprehensive assessment is warranted. Literature suggests that patients referred for DBS by movement disorder specialist neurologists were more likely to be good candidates for DBS than patients referred from other providers.Reference Katz26 Therefore, ensuring patients are first assessed by movement disorder specialists, both for diagnosis, therapeutic optimization and determination of candidacy, would ensure smooth referral pathway flow for patients.
Further investigation is required to better understand how the prevalence of DBS candidates varies across Canada. Currently, no national database exists to answer this question. Improved understanding of the distribution of prevalence of these conditions is critical. It is impossible to comprehensively assess access to a service without an in-depth understanding of the candidates for that service, defining the need for it to determine if that need is being met.
Limitations
A number of limitations exist for the current study. First, there are biases inherent to survey studies, including reporting bias and issues with response rate.
Although limited in number of responses, the representativeness of the Canadian population in patient responses is fair in terms of the proportion of responses by province/territory. There are both an overrepresentation of patients/caregivers from NL (9.8% of responses compared with 1.4% of Canadian population from NL30) and an underrepresentation of respondents from QC (5.9% of responses vs. 22.2% of the Canadian population30), in spite of the survey being offered in both French and English. Unfortunately, there were no responses from Prince Edward Island (PEI), Yukon (YT), Northwest Territories (NWT) or Nunavut (NT). It is important to consider these patient perspectives, given the likely poor access to care in these regions;31,32 however, low response rates may be expected, given the low populations in these areas (0.4% of the Canadian population for PEI and 0.1% of the national population in each of the territories30). All other regions were represented within 2% of the national proportion of the population residing in the respective provinces.
In terms of physician groups, family physicians from NL are again overrepresented (20% of respondents compared with the 2.1% of Canadian family physicians practicing in NL), QC is again underrepresented (3.3% of responses vs. 24.4% of Canadian family physicians33) and AB is underrepresented (6.6% of respondents vs. 13.0%33). All other regions are within 4% of the proportion of Canadian family physicians for each province and territory. Again, no responses were obtained from family physicians practicing in PEI (0.4% of Canadian family physicians33) or the territories, which collectively represent 0.3% of family physicians in Canada.33 The overrepresentation of physicians from NL may have resulted from an active PD society in the province, with advocates eager to promote improved access in the region, as indicated by their contact with us in the early stages of study design. Although we attempted to promote recruitment in QC through the inclusion of French language studies, this may not have been clear to potential participants, as English language information about the study was presented prior to French study information in all correspondence.
Both neurology and neurosurgery were limited in responses, with 22 neurologists responding from 4 provinces and 12 neurosurgeons responding from 3 provinces. This paucity of data from regions of Canada with probable limited access signifies an important missing voice in this narrative. While multiple attempts were made at recruiting participants from these groups, including two faxes and two separate emails, the low response rate may have resulted from recruitment strategies. Many physicians and surgeons receiving faxes would need to be provided the faxed information by administrative personnel. Previous research suggests that physicians are more responsive to mail surveys and that response rates to email are traditionally in the range of 25–30%, due to survey fatigue, competing demands and privacy concerns.Reference Fincham34 Additionally, nearly all responses from neurologists and neurosurgeons are from practitioners in urban settings. Barriers identified by these physicians and surgeons may be vastly different from those in rural settings elsewhere in the country. It is important to note, however, that of all groups surveyed, neurologists and neurosurgeons see patients who have already overcome many barriers to access specialist services, and the ability of these specialists to identify barriers to care may be skewed as a result. The ideas obtained from family physicians and patients/caregivers likely provide a more realistic picture of access.
In terms of estimations of the proportion of patients referred for DBS who go on to receive the treatment, the broad scope of practice of respondents likely hinders the estimations provided. Specifically, only half the neurologists responding were movement disorder specialists. Stroke neurologists, for example, would not be expected to understand the proportion of patients referred for DBS who go on to receive it. Similarly, half of the neurosurgeon respondents reported providing DBS as part of their practice. A spine surgeon would not be expected to understand the complexities of the referral pathway for DBS and therefore is unlikely to make an accurate estimate as to the proportion of referred patients who undergo DBS. Even functional neurosurgeons may not be able to predict the likelihood of a patient undergoing DBS, given that they are situated at the endpoint of this complex referral pathway, as discussed previously. Confidence in these estimations is therefore limited; responses from movement disorder neurologists are more in keeping with literature estimates, and we would expect the most reflective of true referral patterns.
Conclusion
This study surveyed stakeholders for DBS in Canada to identify barriers to accessing DBS. This was an attempt to address limitations of previous studies investigating access to DBS in Canada. A number of themes were generated, describing the beliefs of stakeholders for DBS in Canada regarding barriers, including limited resources/centralization of resources, education, individual patient factors and burdensome referral processes that were determined to be common barriers to accessing DBS. We propose improving education, centralized referral pathways and the use of virtual care to improve access to DBS across Canada and further research to determine the true prevalence of candidates for this therapy to better understand variability in the need for this service across the country.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cjn.2025.71.
Author contributions
ML conceived of the study idea, designed the study protocol and survey materials, completed data collection and analysis and prepared the manuscript with critical edits; AM designed the study protocol and survey materials and contributed to preparation and critical edits of the manuscript; MA assisted with data analysis; RH assisted with design of survey materials and data collection; DP assisted with design of survey materials; DH reviewed results to provide content expert appraisal; FF designed the study protocol and survey materials and contributed to preparation and critical edits of the manuscript; MB contributed to preparation and critical edits of the manuscript; SKK designed the study protocol and survey materials and contributed to preparation and critical edits of the manuscript; SS designed the study protocol and survey materials, contributed to preparation and critical edits of the manuscript and provided supervision for the project from conception to completion.
Funding statement
Funding for data collection tools in this study was obtained from the Regional Medical Associates Research Scholarship, Postgraduate Medical Education, McMaster University.
Competing interests
No potential conflict of interest was reported by the authors.












Target article
Mixed Methods Survey to Identify Barriers to Accessing Deep Brain Stimulation for Movement Disorders in Canada
Related commentaries (2)
Reviewer Comment on Lannon et al. “Mixed Methods Survey to Identify Barriers to Accessing Deep Brain Stimulation for Movement Disorders in Canada”
Reviewer Comment on Lannon et al. “Mixed Methods Survey to Identify Barriers to Accessing Deep Brain Stimulation for Movement Disorders in Canada”