Alice in Wonderland syndrome (AIWS) is a rare neurological condition characterized by distortions in vision, body perception and time perception, sometimes accompanied by depersonalization and derealization. Reference Todd1 It is most frequently observed in children, where Epstein–Barr virus encephalitis is the predominant cause, while in adults, AIWS is most frequently linked to migraine. Reference Blom2 To our knowledge, no prior cases caused by astrocytoma have been reported to date. Since brain lesions are a known cause of AIWS, it is not unexpected that an astrocytoma could result in this condition.
Here, we describe a patient who experienced transient visual distortions, including prosopometamorphopsia and metamorphopsia, consistent with AIWS. These symptoms resolved spontaneously but ultimately led to the diagnosis of a grade 3 astrocytoma.
A 24-year-old man initially presented to a walk-in clinic after experiencing a new headache for two days. The headache was continuous, sometimes waking him from sleep, and was accompanied by nausea, photophobia and flashing lights confined to his left visual field. While the headache evolved into episodic attacks, the flashing lights persisted independently, occurring approximately four times per day, lasting 1–3 minutes per episode and no longer coinciding with headaches. He was diagnosed with migraine with aura and prescribed eletriptan and diclofenac, but these medications provided no relief. A subsequent eye exam was unremarkable.
Four days later, his symptoms progressed. In addition to the flashing lights, he noticed that objects in his left visual field appeared “twisted and cartoonish.” He presented to the emergency department for the first time on day 7 after his initial presentation, at which point we evaluated him. He then reported that reflections of vehicles in his side mirrors appeared disproportionately large (hemimacropsia), creating significant distress while driving. His wife’s eyes seemed exaggeratedly large and distorted when viewed through his left visual field (hemiprosopometamorphopsia), and his left hand appeared so cartoonishly altered that it no longer resembled a human hand but rather a “werewolf hand” (hemimetamorphopsia) (Figure 1), which he drew. These disturbances, all restricted to his left visual field, caused considerable anxiety. The patient had no personal or family history of migraine or epilepsy. Neurological examination was normal aside from his descriptions of left visual field distortions.
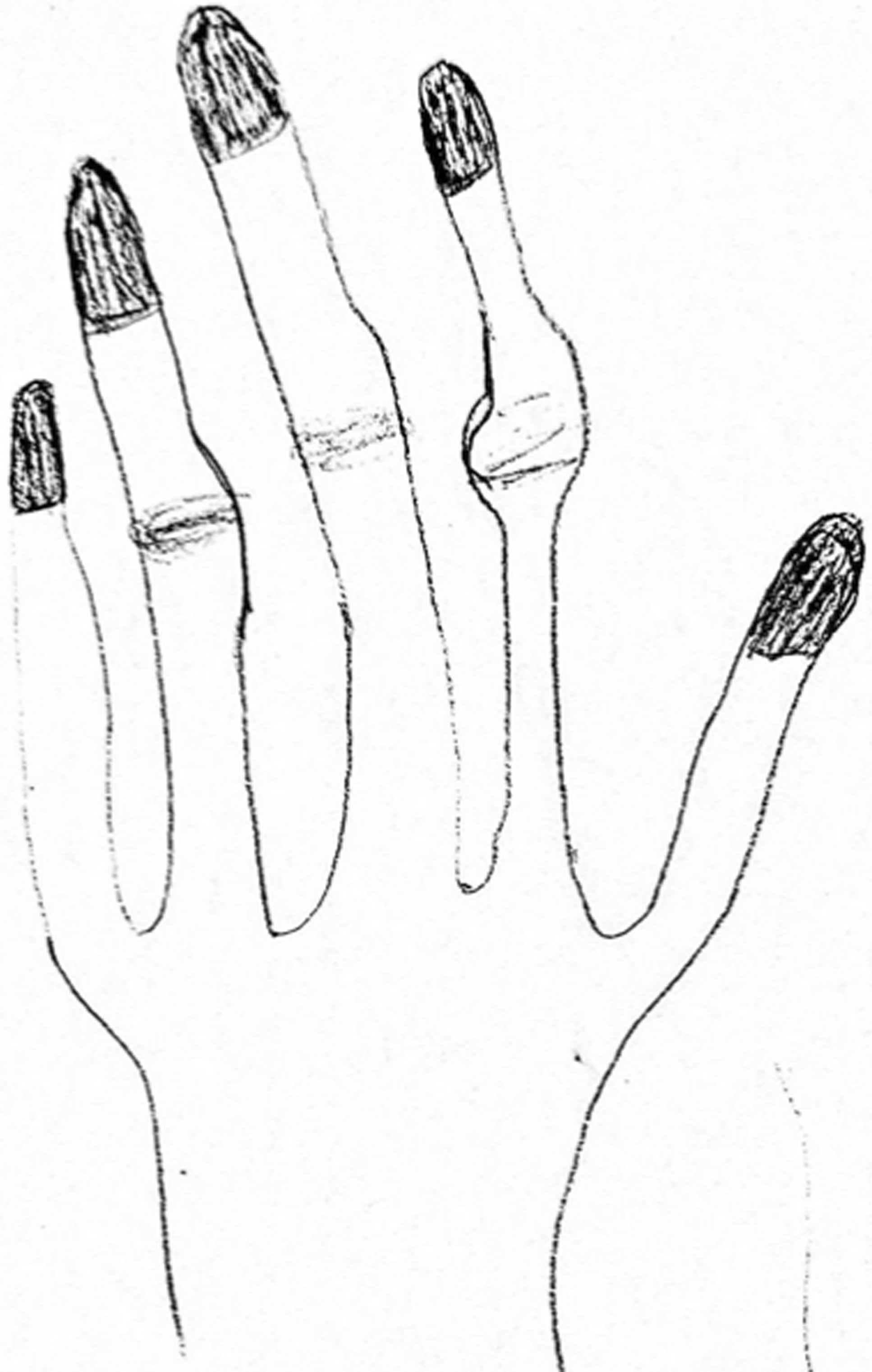
Figure 1. The patient’s drawing of his left hand. The patient’s drawing of his left hand, which appeared distorted and cartoonish (hemimetamorphopsia), so much so that it no longer resembled a human hand but rather a “werewolf hand”.
A head CT scan revealed vasogenic edema in the right occipital lobe with local mass effect. Given the structural abnormality, he was admitted for further evaluation. An Electroencephlogram (EEG) performed during active AIWS symptoms showed focal slowing in the delta and theta ranges but no epileptiform discharges or seizures. By day 10 (the third day of admission), his AIWS symptoms resolved spontaneously.
CSF analysis, including opening pressure, was normal, with no pleocytosis or oligoclonal bands. Tests for John Cunningham virus, varicella zoster virus and herpes simplex virus were all negative. Routine bloodwork was normal. The patient tested negative for fungal cultures, toxoplasmosis and acid-fast bacilli. Additionally, tests for aquaporin-4 (AQP4)-IgG and myelin oligodendrocyte glycoprotein-IgG were negative. A CT scan of the thorax, abdomen and pelvis revealed no evidence of malignancy.
Brain MRI demonstrated a T2-fluid-attenuated inversion recovery (T2-FLAIR) and T2 hyperintense lesion in the right posterior temporoparietal and anterior occipital region (Figure 2A–B). Post-gadolinium imaging showed a non-enhancing, hypointense lesion on T1-weighted sequences (Figure 2C). Additionally, there was a T2-FLAIR mismatch sign and a small area of subcortical restricted diffusion (not shown).
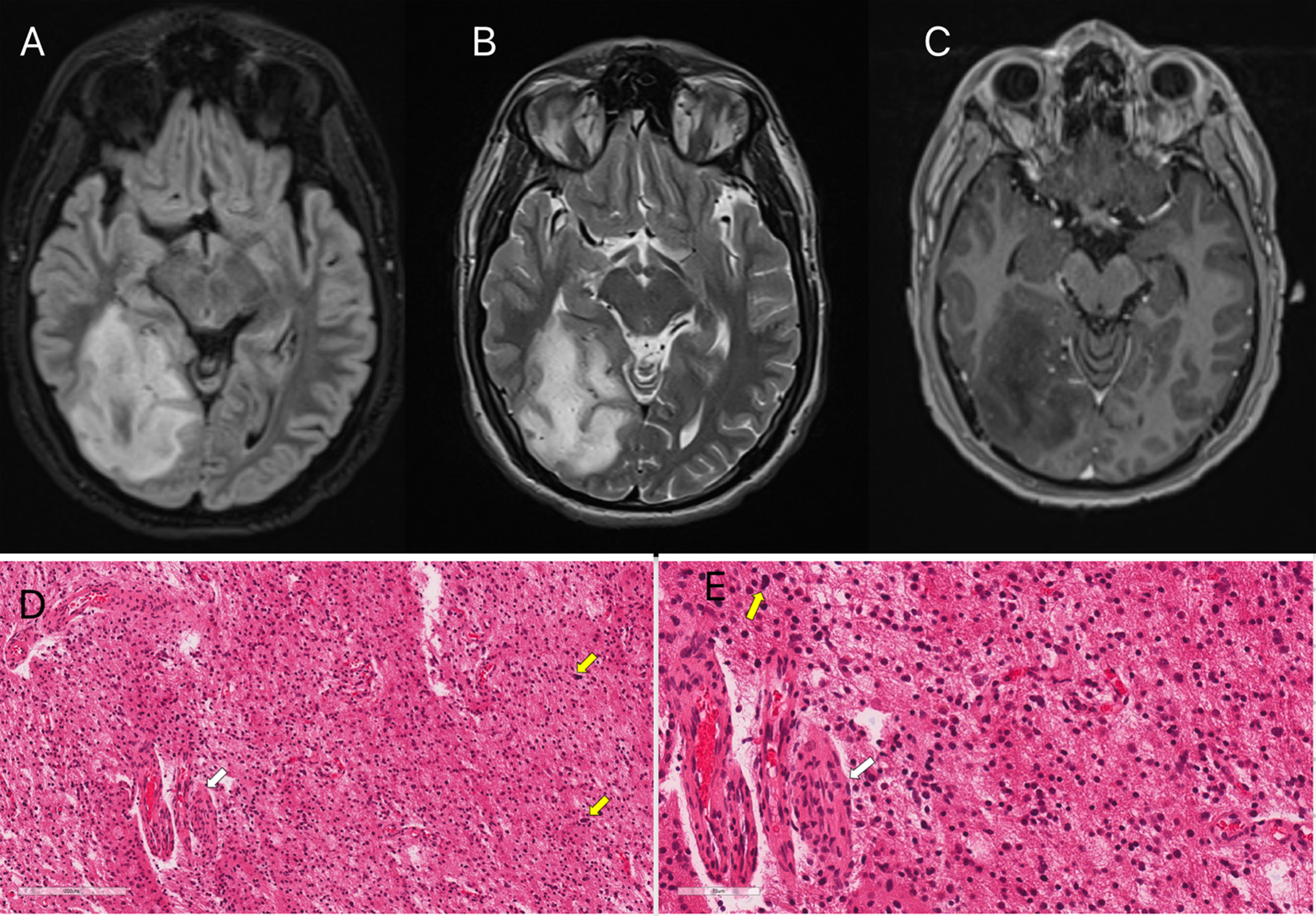
Figure 2. Brain MRI and histopathology slides. (A, B and C) MRI brain showing right posterior parieto-occipital lesion (A = axial T2-fluid-attenuated inversion recovery; B = axial T2; C = axial T1 post-gadolinium). (D and E) Histologic features of the stereotactic biopsy from the parietal lobe lesion: Tumor shows increased cellularity in a fibrillary background. Moderately atypical tumor cells with enlarged, irregular nuclei (yellow arrows) (D and E) and prominent vasculature with endothelial hyperplasia (white arrows) (D and E) are noted. Scattered mitotic figures and karyorrhectic cells are present (not shown).
A stereotactic brain biopsy identified a glial tumor in a fibrillary background (Figure 2D–E). Molecular analyses revealed mutations in ATRX and IDH genes, and cytogenetic studies showed no homozygous deletion of CDKN2A and no 1p/19q codeletion. These findings confirmed a diagnosis of WHO grade 3 astrocytoma. The patient subsequently underwent a subtotal tumor resection, followed by concomitant chemoradiotherapy, and then received adjuvant temozolomide. He is currently stable and continues to be followed up by neuro-oncology. There has been no recurrence of AIWS since its resolution, including after the surgical resection and subsequent chemotherapy of the astrocytoma.
A key region implicated in the development of AIWS is the intersection of the temporo-occipital, parieto-occipital and temporoparietal junctions, where visual and somatosensory information are integrated on either hemisphere. Reference Brumm, Walenski and Haist3 The thalamus regulates information flow between high-level associative cortices, and a lesion, whether structural or functional, disrupting these connections could also contribute to AIWS. Reference Saj, Wilcke, Gschwind, Emond and Assal4
Apart from migraine, AIWS in adults has been commonly associated with epilepsy, medication-induced effects, psychiatric disorders Reference Blom2 and various central nervous system pathologies, including strokes and rarely glioblastoma, Reference Mastria, Mancini and Viganò5 and Creutzfeldt–Jakob disease. Reference Pandey, Keerthiraj, Garg and Chakraborty6
Our patient presented with headache, photophobia and flashing lights, prompting a broad differential diagnosis including migraine with aura, retinal migraine, occipital lobe seizures, structural brain lesions, intracranial hypertension, infections/inflammatory conditions, optic neuritis or other ocular pathologies. The subsequent development of AIWS did not narrow the differential, as migraine aura can present similarly. However, his continuous AIWS symptoms lasting several days were atypical, as migraine-related AIWS tend to be brief and episodic. Occipital lobe focal seizures can also cause AIWS, with focal occipital lobe status epilepticus having been reported. Reference Lawson, Triner and Kluge7 His EEG during AIWS symptoms showed focal slowing but no epileptiform discharges, albeit electrographic correlates in AIWS are infrequently documented. Reference Shah, Magaña and E. Youssef8 Normal CSF opening pressure and an unremarkable eye exam excluded pressure-related and ocular causes, while extensive testing ruled out infectious, inflammatory and demyelinating causes.
The spontaneous resolution of AIWS in his case could be explained by several mechanisms. One possibility is the resolution of perilesional edema, as vasogenic edema in the right occipital lobe likely disrupted visual processing, and as the edema subsided, these perceptual disturbances may have improved. Additionally, while the tumor itself was the primary pathology, transient metabolic, vascular or inflammatory changes surrounding the lesion may have contributed to AIWS symptoms, and their stabilization could have led to symptom resolution. The absence of recurrence, including after surgical resection and chemotherapy, suggests that AIWS was more likely due to a temporary functional disturbance rather than a lasting structural effect of the astrocytoma.
This case illustrates the need to consider a wide range of potential causes for AIWS and demonstrates how a detailed history was crucial in distinguishing it from migraine or epilepsy. The patient’s persistent AIWS symptoms over several days challenge the notion that AIWS is strictly episodic. The lack of epileptiform discharges on EEG suggests that AIWS can result from direct cortical dysfunction rather than seizure activity. Additionally, this case emphasizes the need for neuroimaging in patients with prolonged or atypical AIWS symptoms. The non-enhancing astrocytoma with localized edema at the temporoparietal-occipital junction illustrates how significant subcortical involvement, even with minimal cortical disruption, can impair visual integration, contributing to AIWS. The patient’s description of his distorted hand as a “werewolf hand” highlights the diverse and vivid perceptual distortions seen in AIWS.
Author contributions
-
1. JA: Drafting and revising the article, including medical writing; major role in data acquisition; study conception and design; and analysis and interpretation of data.
-
2. SA: Drafting and revising the article, including medical writing; major role in data acquisition; study conception and design; and analysis and interpretation of data.
-
3. SP: Drafting and revising the article, including medical writing; major role in data acquisition; study conception and design; and analysis and interpretation of data.
-
4. SC: Drafting and revising the article, including medical writing; major role in data acquisition; study conception and design; and analysis and interpretation of data.
-
5. TC: Study supervision; Drafting and revising the article, including medical writing; major role in data acquisition; study conception and design; and analysis and interpretation of data.
Funding statement
This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests
Dr Chan has received honoraria from Pfizer, Teva, AbbVie, Lilly, Miravo, Lundbeck and Novartis.




