Chronic pain in older people
Pain processing is one of the most vital bodily functions and is biologically required for survival. However, chronic pain – typically defined as pain that persists beyond the expected period of recovery (approximately 3 months) and may or may not be related to a specific cause or tissue damage 1 – is a phenomenological experience resulting from complex interactions among biological, psychological and social factors. Reference Gatchel2 Chronic pain is highly prevalent in older people, with the literature revealing considerable variations ranging between 27 and 86%. Reference Larsson, Hansson, Sundquist and Jakobsson3 Chronic pain is associated with significant distress, disability, lower quality of life and social isolation for older people, and also increased expenses and strain on healthcare systems. Reference Domenichiello and Ramsden4 Compared with younger people with chronic pain, older people are more prone to high-impact chronic pain, i.e. chronic pain accompanied by activity/life participation limitations. Reference Pitcher, Von Korff, Bushnell and Porter5 High-impact chronic pain is associated with an increased risk of depression; therefore, there is a high comorbidity of chronic pain and depression in older people, and a 2-year longitudinal study among older adults estimated that it affects 13% of the older adult population. Reference Mossey and Gallagher6 The coexistence of chronic pain and depression also tends to aggravate the severity of both disorders further, leading to a higher disease burden. Reference Cohen, Vase and Hooten7
Researchers have proposed several theories for the high comorbidity of chronic pain and depression. From a biological perspective, it has been suggested that there are considerable overlaps between the neural mechanisms in processing and responding to pain and depression in the brain. Reference Sheng, Liu, Wang, Cui and Zhang8 For example, the decreased availability of monoamine neurotransmitters, including serotonin, dopamine and norepinephrine, plays a vital role in the development of depression and is also important for the occurrence and development of pain. Reference Ossipov, Dussor and Porreca9 So far, pharmacological treatment of pain has predominantly focused on suppressing physiological responses by using opioids. However, despite its effectiveness in managing acute pain when used appropriately, long-term opioid use for chronic pain may harm both individuals and society. Reference Dowell, Haegerich and Chou10 In addition, some opioids may increase the risk of serotonin toxicity when combined with antidepressants, causing complications in treating comorbid chronic pain and depression. Reference Perananthan and Buckley11 Therefore, treatment for chronic pain is often approached from multidisciplinary and biopsychosocial perspectives, particularly for older adults, and non-pharmacological treatments focusing on the intricate link between chronic pain and depression have been gaining increased recognition. Reference Moisset, Bouhassira, Couturier, Alchaar, Conradi and Delmotte12
Evidence-based non-pharmacological interventions
Exercise and psychosocial interventions are the two main non-pharmacological interventions that have shown effectiveness in managing chronic pain. Reference Hoffman, Papas, Chatkoff and Kerns13 Various types of exercise, such as resistance training, balance and aerobics, effectively prevent falls and improve physical limitations imposed by pain. Reference El-Khoury, Cassou, Charles and Dargent-Molina14 Considering the biopsychosocial aspects of well-being, combining physical activity and mental health strategies to manage pain has been advised. Reference Hoffman, Papas, Chatkoff and Kerns13,Reference Reid, Eccleston and Pillemer15
The most commonly used mental health strategy for chronic pain is cognitive–behavioural therapy (CBT). The primary objective of CBT is to mitigate pain and distress by regulating and altering maladaptive thoughts, behaviours and physical sensations associated with pain. Reference Vlaeyen and Morley16 A systematic review and meta-analysis reported modest advantages of CBT in reducing pain and catastrophising beliefs, as well as enhancing self-efficacy in pain management among the older adult population. Reference Niknejad, Bolier, Henderson, Delgado, Kozlov and Löckenhoff17 However, the paradox lies in the fact that the intent to control thoughts and pain may inadvertently escalate the severity of pain. Reference Masedo and Esteve18 Moreover, CBT does not yield benefits for all individuals experiencing chronic pain; for instance, older adults are less likely to report a decrease in pain interference than their younger counterparts post-CBT. Reference Vlaeyen and Morley16
Other approaches gaining momentum are ‘third-wave’ interventions, such as mindfulness-based cognitive therapy, mindfulness-based stress reduction, and acceptance and commitment therapy. Reference Veehof, Trompetter, Bohlmeijer and Schreurs19,Reference Rosenzweig, Greeson, Reibel, Green, Jasser and Beasley20 Mindfulness, a multifaceted construct encompassing observation, description, acting with awareness, non-judgement and non-reaction, is strongly tied to acceptance, particularly in the latter two facets. Reference Rosenzweig, Greeson, Reibel, Green, Jasser and Beasley20 A meta-analytic review of the effects of mindfulness- and acceptance-based therapies on mental health and pain interference outcomes suggested that these approaches had small to moderate effect size at post-treatment, and from small to large effect size at follow-up, demonstrating them as a good alternative to CBT. Reference Veehof, Trompetter, Bohlmeijer and Schreurs19
Despite the promising effects of evidence-based non-pharmacological interventions, several obstacles exist in conducting such interventions in older Chinese, particularly tied to depression. The stigma of mental health and face-saving culture may hinder older Chinese people from seeking help related to depression and chronic pain. Preservation, maintenance and protection of the ‘face’ are crucial Confucian principles that many Chinese practice. Reference Yang, Chen, Sia, Lam, Lam and Ngo21 Face, according to Confucian philosophy, represents a person’s status, including social, wealth, power and moral status. Reference Yang, Chen, Sia, Lam, Lam and Ngo21 Chinese people, particularly older Chinese people, would rather hide than disclose any mental illness status to save face, leading to greater stigmatisation in Chinese society as well as internalised stigma. Reference Shi, Shen, Wang and Hall22 Although older people frequently seek help for their chronic pain, when the intervention targets comorbid chronic pain and depression, their rate of help-seeking is low. Reference Shi, Shen, Wang and Hall22
Creative arts-based interventions
Over the past few decades, creative arts have been increasingly used for mental and physical health and have been shown to be beneficial for mental well-being, Reference Jensen and Bonde23 although arts specifically for chronic pain is a relatively nascent area. A review discussed how creative arts therapies might treat the biopsychosocial dimensions of chronic pain through lower pain perception, by directing the mental focus away from the pain sensation and focusing on here-and-now activities and sensory awareness interacting with art materials. Reference Angheluta and Lee24 It is worth noting that art therapy and participatory art are not equivalent: the former is typically practised by trained art therapists and regulated by professional bodies, whereas the latter is usually community-based, facilitated by artists and other mental health professionals. Reference Stickley, Wright and Slade25 Nevertheless, both art therapies and participatory arts utilise various art forms, and the therapeutic effects can be embedded in the art-making process. Reference Pamelia26 Creating artwork functions not only as a distraction, but also as an experiential way of teaching people how to regain control over their lives by selecting art materials and creating something unique, offering a potent medium for self-expression and a creative outlet. Reference Shukla, Choudhari, Gaidhane, Syed and Gaidhane27
The intersection of neuroscience and the arts has opened up fascinating insights into how engaging in creative artwork can potentially ‘rewire’ pain experiences and narratives. This process is rooted in the brain’s remarkable plasticity its ability to reorganise and form new neural connections throughout life. Reference Vaisvaser28 Moreover, arts are also deemed enjoyable and stigma-free, and have already been adopted by many care services for older people, including in Chinese communities. Reference Liu, Chan, Yeung, Lee, Chan and Welton29 In short, there is enormous potential for applying arts to ameliorate chronic pain and depression in older adults.
Research gap
Given the increasing interest in non-pharmacological modalities and the expanding number of studies in utilising creative means in care over the past decade, we used a participatory approach to co-design an intervention using creative arts and crafts. We tested its feasibility and effects through a pilot study. The aims of this paper are to (a) describe the participatory co-design process of the cultural arts programme for older adults at risk of depression; (b) report on a pilot test of the intervention examining its feasibility and post-intervention effects on increasing empowerment, reducing self-stigma about depression and ageing, and reducing depressive symptoms among older adults in Hong Kong; and (c) describe the final intervention programme.
Method
This study used a mixed-methods design and drew on participants in a community-based holistic mental health programme for older adults at risk of or with subthreshold depressive symptoms in Hong Kong (JC JoyAge). Reference Liu, Leung, Lu, Kwok, Sze and Tse30 All study participants were recruited from district-based community care centres for older people, through JC JoyAge. The arts-based intervention for older adults with chronic pain and depression is part of a randomised controlled trial (ClinicalTrials.gov identifier: NCT05528536); other than arts and crafts, participants also receive physical exercise, and details of the exercise protocol are described elsewhere. Reference Leung, Fong, Kwok, Shum, Liu and Chan31
Phase 1: co-development of the protocol
Sample
The protocol’s co-development was led by an expert panel comprising two researchers, four professionals (one registered art therapist recognised by the Art Therapy Credentials Board, one counsellor, one social worker and one clinical psychologist, all of whom had extensive experience working with older adults), and three older adult volunteers (potential patients aged 60 years or over). They all provided written consent before participating in the co-development workshops.
Procedure
The co-development process was conducted mostly online because of public health considerations caused by the COVID-19 pandemic. First, two researchers undertook a literature review on chronic pain, depression, effective interventions for older adults with these two conditions and the utility of arts for chronic pain management. They summarised and shared the results with all professionals and older adult volunteers. Second, the researchers facilitated two workshops (each of 3 h duration) with participants to co-design the protocol, and conducted follow-up telephone calls and Zoom meetings for clarification. Third, the researchers consolidated the materials from the two workshops and participant feedback, drafted a protocol and shared it with all participants for review. Fourth, the researchers arranged a Zoom meeting with two professionals and three additional older adult volunteers not involved in the design process, to try out one arts-based activity (origami). Participant feedback on the feasibility of the activity was collected, and more details on the rundown and group contract were discussed with the professionals. Finally, the researchers and one art therapist refined the intervention protocol based on feedback from the online trial, and there were several iterations before the protocol was finalised. The co-design process lasted from October 2021 to March 2022. During this process, all participants were empowered to feel that they were the experts of their experiences and contributed to the creativity design process with their domain of expertise. The empowerment was realised through knowledge transfer and mutual learning. All participants, researchers, professionals and older adults worked collaboratively without a power hierarchy. In this process, participants were encouraged to ‘power within’, i.e. unlock and mobilise knowledge and resources they had access to, and ‘power with’, i.e. connect and gain capacity with one another in the group towards the same objective.
Phase 2: pilot study of acceptability and feasibility of the protocol
Sample
A convenience sample was recruited from two partnered community care centres for older adults in the JoyAge project. Reference Liu, Leung, Lu, Kwok, Sze and Tse30 The JoyAge project serves community older adults aged 60 years and above who are at risk of or with mild to moderately severe depressive symptoms, and the recruitment is done through non-governmental organisations. The inclusion criteria of this pilot study were as follows: (a) aged 60 years or above, (b) mild to moderately severe depressive symptoms (operationalised as a total score between 5 and 19 for the Patient Health Questionnaire-9 (PHQ-9)), Reference Kroenke, Spitzer and Williams32 (c) chronic pain for over 3 months and (d) able to give informed consent to participate. Exclusion criteria were as follows: (a) a known history of autism, intellectual disability, schizophrenia spectrum disorder, bipolar disorders, Parkinson’s disease or dementia; (b) imminent suicide risk; (c) difficulty in communication; (d) a stroke, fracture, cardiovascular disease, cardiovascular surgery, artery disease, surgery on vertebrae or knee replacement in the past 6 months, for the principle of ‘do no harm’, as this group may be at higher risk for adverse outcomes; and (e) prohibited from physical activity on the advice of a medical professional.
Procedure
All participants provided written consent before participating in the pilot study. They completed a questionnaire and performed a fitness test before the intervention (T0), after the intervention (T1) and 3-month follow-up (T2). The intervention includes 8 weeks of arts and crafts (2 h each week) and guided exercise (1.5 h each week). In the pilot phase, the arts and crafts component was conducted by a provisional registered art therapist with an assistant trained in psychology, and the exercise component was led by a physiotherapist. At the post-intervention assessment, participants were also invited to a 90-min focus group facilitated by two trained research assistants who were not involved in delivering the intervention. The focus groups were conducted in Cantonese, recorded and transcribed verbatim for analysis.
Measures
Primary outcomes
Pain severity and pain interference were assessed with the 11-item Brief Pain Inventory. Reference Ger, Ho, Sun, Wang and Cleeland33 Pain experience and its impact on daily activities were measured from 0 (no interference) to 10 (interferes completely). Separate means were calculated for severity and interference items (Cronbach’s alpha for severity 0.81; Cronbach’s alpha for interference 0.89).
Depressive symptoms were assessed with the Chinese version of the PHQ-9. Reference Chen, Chiu, Xu, Ma, Jin and Wu34 The assessment combines depression diagnostic criteria with other leading major depressive symptoms, and the frequency of the symptoms is rated from 0 (not at all) to 3 (nearly every day). The total score ranges between 0 and 27, and it is divided into the following categories of increasing severity of depressive symptoms: 0–4 none, 5–9 mild, 10–14 moderate, 15–19 moderately severe and ≥20 severe (Cronbach’s alpha 0.91).
Secondary outcomes
Anxiety symptoms were assessed with the validated Chinese version of the two-item Generalised Anxiety Disorder (GAD-2) questionnaire, Reference Luo, Li, Hou, Zhang, Liu and Qian35 a screening tool for generalised anxiety disorder, using the two core questions from the GAD-7: feeling nervous/anxious and control worrying. Scores range from 0 (not at all) to 3 (nearly every day) for each question.
Health-related quality-of-life was assessed with the 12-item Short Form Survey (SF-12), Reference Ware, Kosinski and Keller36 comprising 12 questions measuring eight health domains to assess physical and mental health. Item scores range from 1 (all the time) to 6 (none of the time); the higher the score, the higher the health-related quality of life. Separate means were calculated for physical health and mental health items (Cronbach’s alpha 0.91).
Other secondary outcomes of exercise include gait speed and mobility, balance, lower and upper body strength, and aerobic capacity. Supplementary Table 1 includes details of the measures for these outcomes.
Descriptive measures
Participants’ demographic characteristics were collected, including age (in years), gender, level of education, marital status (married versus single, divorced or widowed), mobility (ambulatory versus non-ambulatory), hearing status (normal versus impaired), body mass index and methods used for pain relief.
Focus group interview
The purpose of the focus group was to understand the experiences of the intervention group participants, including their perceptions of the usefulness of arts and crafts for pain and depression and the potential mechanisms. Eight open-ended questions guided the focus group on two dimensions: (a) comments on the group activities and (b) perceived influence on themselves. Details of the questions are included in Supplementary Table 2 available at https://doi.org/10.1192/bjo.2025.10062.
Observational notes
After every session, two research assistants and two facilitators recorded observational notes. A framework was used for recording the observations, and the following aspects were included: (a) subjective participants’ subjective sharing about pain experience, and feelings during and after art-making; (b) objective observation of participants’ behaviour and arts created during the session; and (c) personal assessment and reflection participants’ personal assessment as how art making affects their pain experience/interference, and reflection of what works for them. In total, 16 notes were collected: half from the research assistants and half from the facilitators.
Analysis
Quantitative data analysis
Participants’ characteristics were analysed by using descriptive statistics. Participants who withdrew from the intervention and their reasons for withdrawal were also documented. Primary and secondary outcomes and treatment process measures were analysed by Wilcoxon signed-rank test, because it is suitable for data from a small sample that do not fulfil normal distribution assumption required for the paired t-test. All quantitative analyses were conducted with SPSS software (version 29.0 for Windows).
Qualitative data analysis
Two independent researchers with a significant background in mental health studies who were not involved in the pilot study transcribed the recordings from the focus groups. Then, they conducted a thematic analysis of the transcription and observational notes. This analysis involved an iterative method that included getting acquainted with the data, creating codes, identifying and outlining themes, and refining those themes. First, a sample of focus group transcription and two observational notes were analysed jointly (H.S.K., J.K.Q.L.) to create a list of initial codes, which were then merged, refined and sorted into a hierarchy of overarching themes. Second, coders independently coded another focus group transcription and two more observational notes with the codes developed in the first step, then they met to review and compare their coded passages. Deviant cases were discussed with two senior researchers (T.L., D.K.Y.L.), to arrive at a consensus, and themes were refined based on the coded data. This process of researcher corroboration is designed to maximise the trustworthiness of results and minimise bias within the analysis process. Reference Nowell, Norris, White and Moules37 Finally, researchers coded the remaining transcriptions and observational notes with the refined codebook. Microsoft Excel 2021 for Windows was utilised for the analyses.
Ethics statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human patients were approved by the Human Research Ethics Committee of the University of Hong Kong (reference numbers: EA2003001A and EA200132).
Results
Phase 1: Rewire with Arts protocol
Objectives and guiding principles
Volunteers, art therapists, social workers and counsellors agreed on the programme’s objectives, including reducing pain interference and depressive mood and increasing empowerment. Five fundamental principles were derived from these objectives to guide the design of the protocol to (a) balance between novelty and familiarity in the choice of art materials; (b) allow different levels of participation, ranging from appreciation to modelling and creation; (c) bring awareness to self-control over the perception of pain when creating artworks; (d) reinforce positive feedback within and between members in groups and (e) generate a sense of fulfilment through making and sharing art products.
Arts and crafts chosen for the programme
The importance of materials
In creating artwork, art material has a pivotal role in enabling or constraining the experience and expression of participants. Art materials can be used as an object of transference for clients, projecting their internal feelings, emotions and memories. Reference Taylor and Statler38 Compared with traditional psychotherapy, using art materials could enhance participants’ self-exploration, encouraging them to externalise their feelings and emotions. 39 The expressive therapies continuum (ETC) is a theoretical model for assessing and applying media in art therapy. 39 Although this study focused on developing a participatory arts and crafts programme that differs from art therapy in the degree of using art as a psychotherapy element, we referenced the ETC model in choosing art materials. According to the ETC, artistic creation consists of four dimensions: (a) kinaesthetic/sensory (K/S level), expressing feelings through body movements; (b) perceptual/affective (P/A level), converting feelings into images to release suppressed emotions; (c) cognitive/symbolic (C/S level), identifying the meanings of symbols, and (d) creativity, performing creative functions using the other three dimensions. 39 Guided by the principles agreed by the expert panel and the ETC theory of art therapy, four arts and crafts modalities were chosen, and the choice was balanced between familiarity and novelty, which were origami (paper folding), decoupage (cut out and collage), mosaic and collective collage. The descriptions of the art materials, the rationale of choice, their relation to Hong Kong older adults and ETC levels are summarised in Supplementary Table 3.
Prototype and structure of each session
The prototype consisted of eight 2-h weekly sessions, covering the four arts activities as aforementioned; details of each session are summarised in Table 1. Art therapists suggested a higher level of structure within each session, i.e. routine, because it can lower the cognitive requirement and provide a relative sense of familiarity and a non-threatening environment for expression. In addition, warm-up activities with arts, such as pain drawing sketches and mindfulness-based interaction with art materials, may enable participants to focus on their pain in the here and now. The routine was co-developed by professionals and older people and is summarised in Supplementary Table 4.
Table 1 Outline of the 8-week Rewire with Arts programme
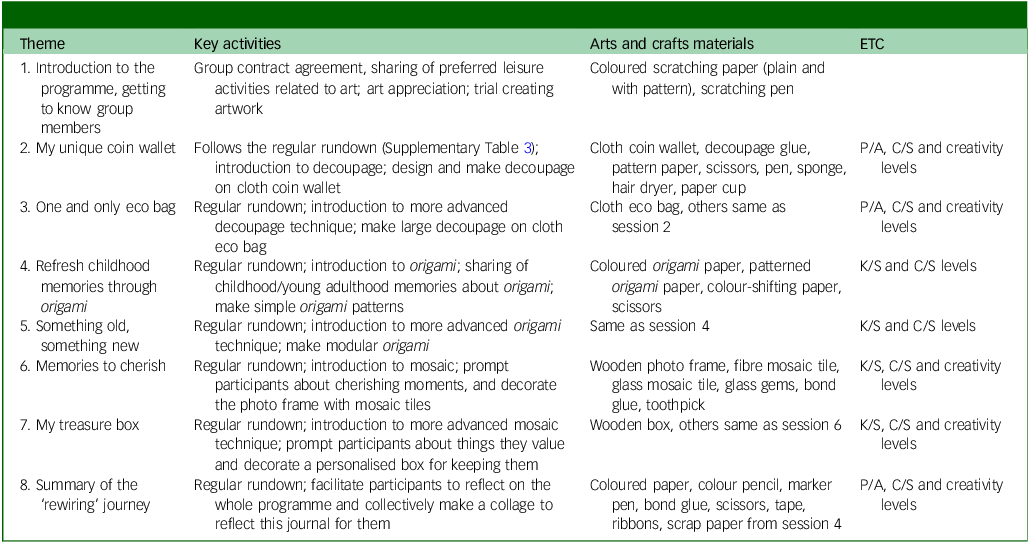
ETC, expressive therapies continuum; P/A, perceptual/affective level; C/S, cognitive/symbolic level; K/S, kinaesthetic/sensory level.
Phase 2: pilot study findings
Quantitative data results
Twelve participants, all female, with a mean age of 71.4 years (s.d. = 7.9), were enrolled in the pilot group. Just under two-thirds (58.5%) completed their education at secondary school or higher. All participants completed the intervention with over 80% attendance. Other demographic information is summarised in Table 2. All of them self-reported to have chronic pain for over 3 months, and none of them had a diagnosis of depression or were on antidepressants. Participants used various methods for pain relief, including paracetamol (n = 9), pain relief patches/tapes (n = 9), dit da jow (a traditional Chinese medicine for external use only, n = 8), acupuncture (n = 6) and massage (n = 5).
Table 2 Pilot group participants’ demographic characteristics and pain relief methods (n = 12)
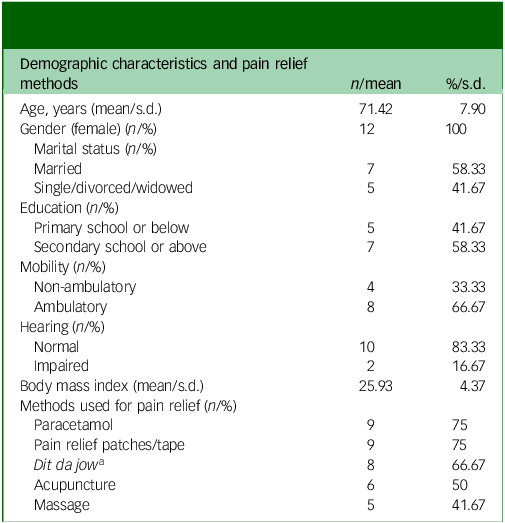
a Dit da jow is a common Chinese liniment used as traditional medicine for reducing pain through external use.
Table 3 summarises the clinical measures at three time points. No significant change was observed between T0 and T1, presumably due to the small sample size; although there could be a delayed effect, because significant improvements were found in mental health as indicated by reduced PHQ-9 total scores (Z = −2.60, P < 0.01) and PHQ-9 cut-offs for depressive symptom severity (Z = −2.53, P < 0.01), and increased SF-12 mental health scores (Z = −2.67, P < 0.01) between T0 and T2. In terms of pain interference, there was no significant change between T0 and T1; however, on the individual items, the interference of pain on enjoyment of life decreased from T0 to T2 (Z = −2.02, P < 0.05). Similarly, in physical domains, no significant difference was found between T0 and T1. Participants showed significant improvements at T2 over T0 in the 30-s sit to stand test (Z = −2.57, P < 0.05), grip strength in both right (Z = −2.94, P < 0.01) and left (Z = −2.05, P < 0.05), and 2-min step test (Z = −2.54, P < 0.05).
Table 3 Outcome measures in pilot testing (n = 12)
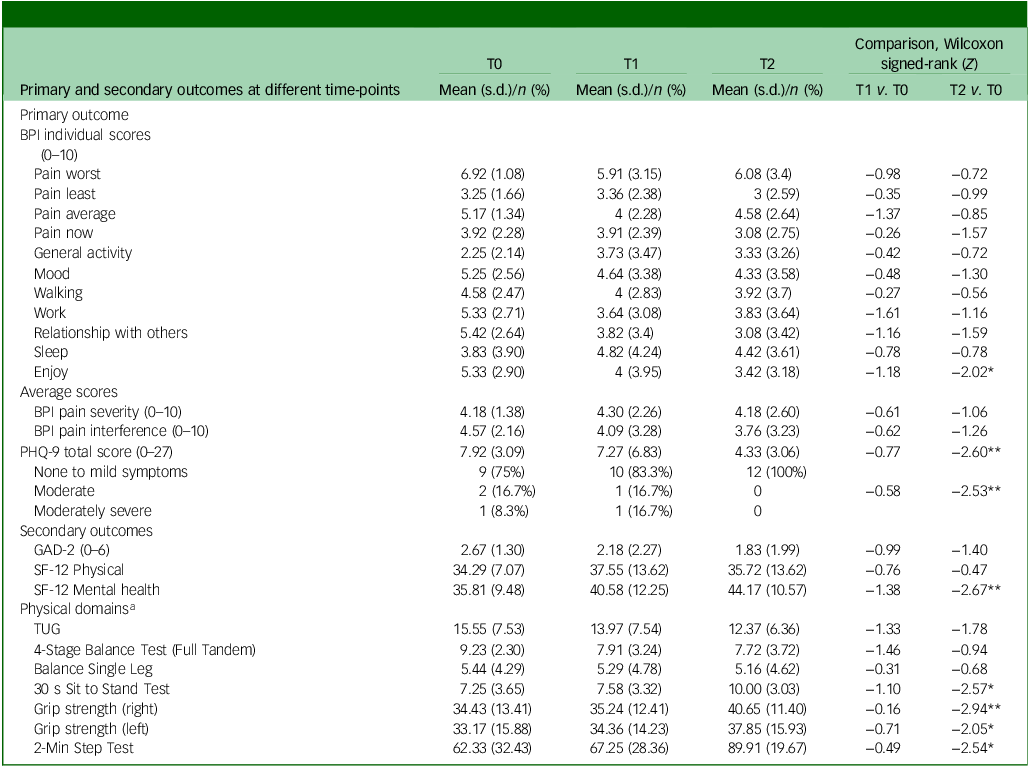
T0, baseline; T1, post-intervention; T2, 3-month follow-up; BPI, Brief Pain Inventory; PHQ-9, Patient Health Questionnaire-9 item; GAD-2, Generalised Anxiety Disorder-2 item; SF-12, Health-related quality-of-life Short Form; TUG, Timed Up and Go.
*P < 0.05, **P < 0.01.
a The descriptions and details of physical domain outcomes are summarised in Supplementary Table 1.
Qualitative data results
Six of the 12 pilot study participants participated in the focus group; others did not because of time clashes. Supplementary Table 5 presents an organised summary of the themes and codes from the focus group discussion and observational notes, featuring illustrative examples from participants’ statements.
Acceptability and feasibility of the programme
All participants commented on the programme’s acceptability and feasibility for various reasons. Four mentioned it was a new and novel experience, and all agreed that the activities were fun and pleasing. One mentioned that the programme could be integrated into the regular activities offered in the care centres.
Perceived changes related to pain coping
Participants mentioned insights they gained from this programme and how that influenced their coping with pain. They highlighted the implication of the pain drawing sketch activity (Fig. 1, description of activity in Supplementary Table 2) for increasing their awareness of bodily sensations and acceptance of pain. All expressed how participating in creating artwork enabled them to achieve a better locus of control and made them realise that they could perform tasks without feeling pain: ‘Time went so fast when we created artwork. I realised that I did not feel the pain while creating artwork’.
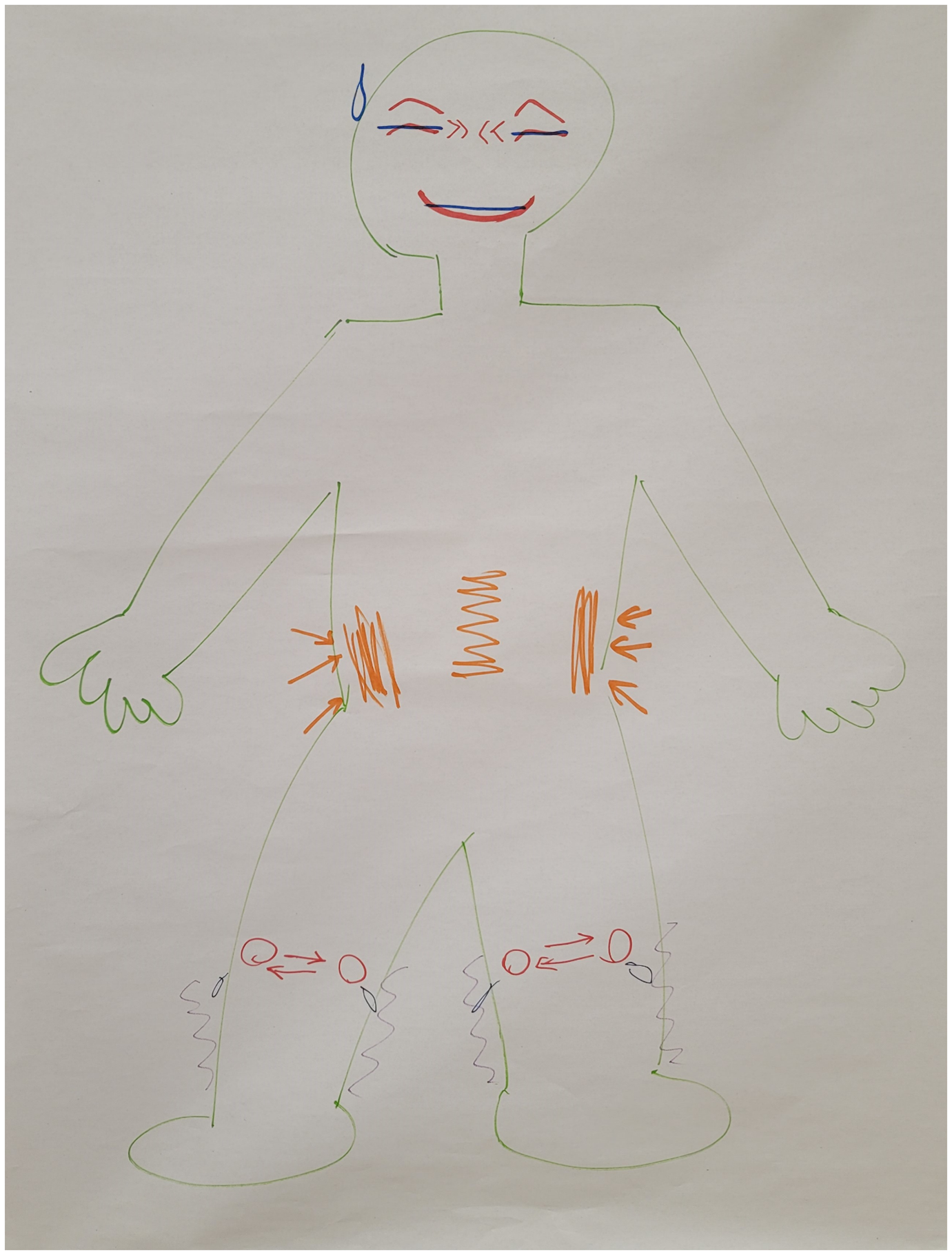
Fig. 1 Example of pain drawing sketch. Areas of pain in the body are marked with different shapes and colours; the facial expression changed from ‘helpless’ before the session started (blue marker) to ‘happy’ (red marker) at the end of the session.
Effects of arts and crafts
Participants mentioned the effects of arts and crafts on their mental wellness, both the process of creating artwork and the final products. They shared that creating artwork gave them a sense of achievement; they appreciated the aesthetic values of art products; they felt empowered to learn and try new things in their free time; and the art products made them seen and appreciated by their friends and families. Two participants mentioned giving their artwork as gifts to their friends: ‘I showed my friends the coin bag we made, and they appreciated it so much and praised me for my skills. The artwork made me seen by other people’. One participant video-called her grandson, who was in London, showcased her work to him and said she would tailor one for him when he next returned home.
Effects of group and peers
All participants mentioned the effects of group and peers, and they attributed the changes they experienced to the therapeutic alliance with the facilitators, the non-judgemental and safe environment in the group for them to share, the camaraderie among group members so that they felt understood and accepted, the resource sharing and the overall harmonic atmosphere. One participant shared her feelings when making the collective hand drawing (Fig. 2; description of activity in Supplementary Tables 3 and 4) and said: ‘I enjoyed the collective artwork the most; we bonded, and our hand drawings formed a “blooming garden”’.
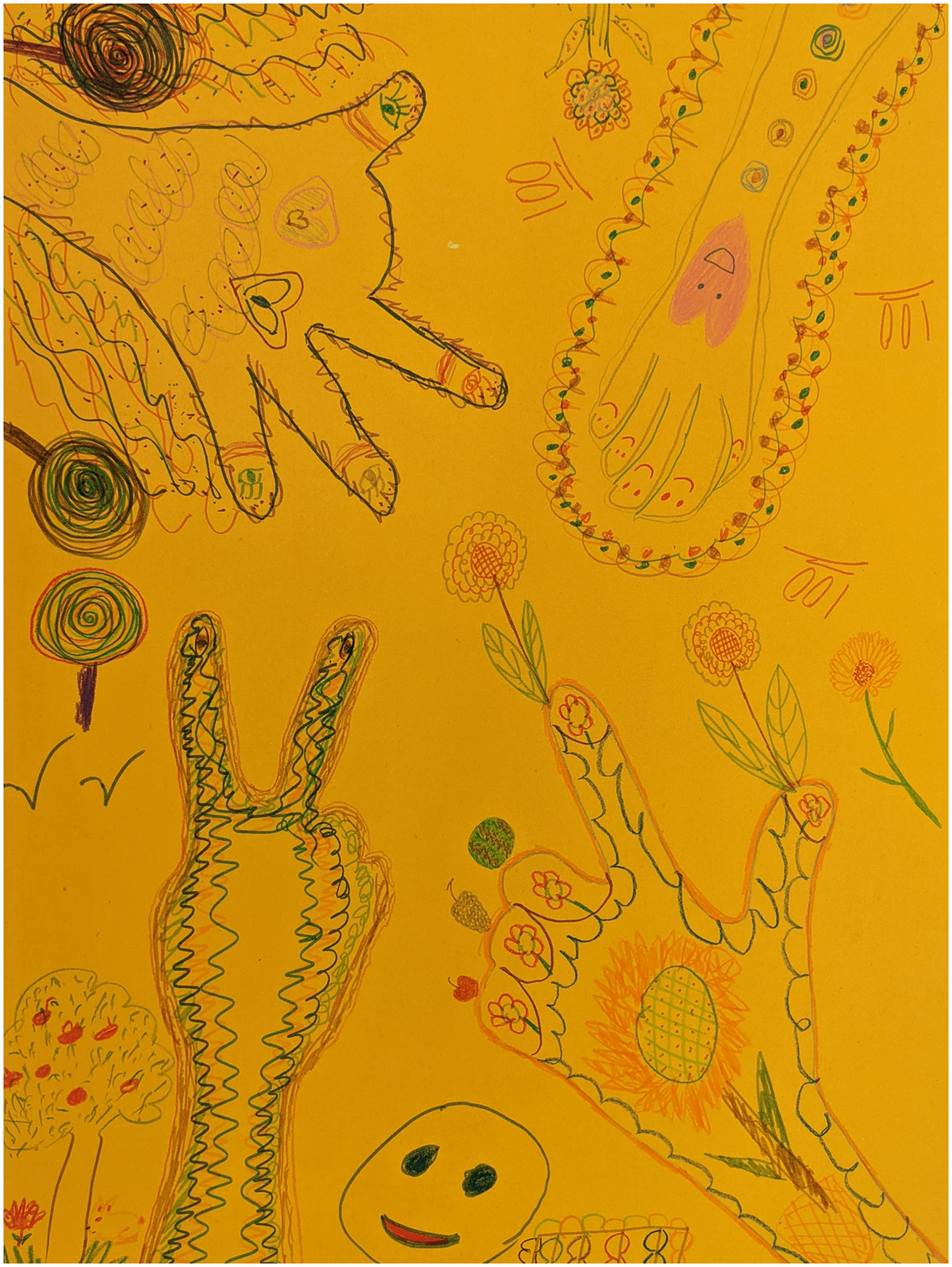
Fig. 2 Example of group hand drawing.
Challenges
Participants also mentioned the challenges they faced in and outside the programme, including comparison with others, high demand for dexterity in some activities and difficulty finding the same art materials outside the programme. One objective of the programme was to reinforce positive feedback within and between members of groups. To address the potential inferior feeling derived from comparison, the facilitator stressed the subjective qualities of aesthetics throughout the sessions, and that there is no absolute standard for comparison.
Discussion
Utilising an iterative and collaborative approach, participants designed the Rewire with Arts programme, which used arts and crafts for older adults with chronic pain and depressive symptoms. Our two-phase research highlighted the significance of involving key stakeholders in the creation of an innovative programme for this population, and provided early evidence of how creating artwork can contribute to the improvement of mental health and coping with chronic pain. These results can potentially encourage the development of more groundbreaking programmes to benefit the mental wellness of this population, by incorporating arts and other creative aspects in the process and inform a more comprehensive programme evaluation in the future.
Our study shows that this creative arts-informed programme was feasible and well-accepted by older adults with chronic pain and depressive symptoms. It has the potential to be integrated into the regular programmes offered in care centres for older people and, therefore, scaled up in community settings. The outline of each session and descriptions of arts-based mindfulness activities may serve as training materials for professionals or paraprofessionals in care centres for older people. The enjoyable and stigma-free nature of art appreciation and creating artwork may further attract older adults with mental health risks who are unknown to the existing services.
Moreover, the engaging nature of the creative arts process and the tangible art product, which others can see and appreciate, may offer benefits compared with other psychotherapies. During the sessions, participants recounted that they forgot or got distracted from their perception of chronic pain, which is partly because the immersive nature of creative artwork can serve as a distraction, drawing attention away from pain and toward the creative process. This may reflect them entering a mindful or flow state, characterised by being absorbed in the activity, losing a sense of time, and intense and focused concentration, which is an intrinsically rewarding experience. Reference Dietrich40 Several neurobiological mechanisms may explain the flow state and positive outcomes. First, engaging in creating artwork activates the brain’s reward pathways, releasing neurotransmitters like dopamine. Reference Magsamen and Ross41 This creates a sense of pleasure and satisfaction and modulates pain by shifting attention away from pain signals, thereby altering the individual’s experience of pain. Second, creating artwork has also been shown to lower cortisol levels, a stress hormone, in the body. Reference Kaimal, Ray and Muniz42 Since stress can exacerbate pain perception, reducing stress through art can indirectly mitigate pain experiences. Third, engaging in the arts can stimulate neuroplastic changes in the brain, enhancing its ability to reorganise and adapt. Reference Bolwerk, Mack-Andrick, Lang, Dörfler and Maihöfner43 This includes the potential to alter the way pain is processed and perceived. Finally, creating artwork allows for cognitive reappraisal or the reinterpretation of experiences, Reference Bolwerk, Mack-Andrick, Lang, Dörfler and Maihöfner43 thus enabling individuals to construct new narratives around their pain that may be more positive or empowering.
Participation in group settings can foster a sense of community and support, and creative arts activities can provide a safe environment for older adults to process life experiences and promote personal growth. Social support is known to be a crucial factor in coping with chronic pain; Reference López-Martínez, Esteve-Zarazaga and Ramírez-Maestre44 the shared experience of chronic pain and creating artwork can strengthen feelings of connection and reduce feelings of isolation associated with pain. Empirical studies show that group intervention is more effective in reducing loneliness and improving health and cognition for older people. Reference Pitkala, Routasalo, Kautiainen and Tilvis45 Researchers also point out that in group-based and goal-oriented interventions, the participants themselves can influence the structure and the outcome of the group rather than just being group followers, leading to empowerment and improved well-being for participants. Reference Cattan, White, Bond and Learmouth46 However, it is also worth noting that some participants mentioned that the nature of the group may induce stress as a result of comparing their own and others’ artwork. Facilitators of arts-based groups must be mindful of this potential side-effect, and remind the participants that there is no objective standard in arts.
Limitations
The study has several limitations. First, the pilot sample size was limited and lacking a comparison group, which made it difficult to rule out the possibility of regression toward the mean in the improvements. A more robust study design is necessary to confirm the programme’s efficacy, such as a quasi-experimental study or, where feasible, a randomised controlled trial. Second, the arts and crafts programmes were administered in a group setting, making it hard to discern the effects of social activities from engaging in arts. A comparison group with participants engaged in individual art-making is needed in future research. Third, the findings may not apply to the broader population of older adults experiencing chronic pain and depression. The pilot study’s participants may not represent the entire demographic because they were voluntarily recruited from community centres, all female, already engaged in community activities and showed a preference for art-related activities. Subsequent research should use more purposive sampling to include individuals from the community who are less active, experience chronic pain and are more susceptible to depression. Fourth, the quantitative assessments did not capture many of the changes reported by participants, suggesting the influence of the small sample size. In addition, the ‘rewiring’ of pain experience cannot be captured by behavioural measures; a trial with neurological measures, such as functional magnetic resonance imaging, is needed to elicit neurological evidence. Nevertheless, our study provides preliminary information on the benefits of the arts-based programme, particularly on depressive symptoms and mental health-related quality of life. Future studies should strive to build on our work and capture significant personal experiences and quantifiable outcomes with a more representative sample. The artwork produced by participants in the pilot study has not been thoroughly examined in conjunction with quantitative data and focus group feedback. Given that the programme is centred on art, it is imperative to incorporate art-based research and evaluation methods to uncover its impact, which the current methods of analysis may have overlooked.
In summary, a co-designed, culturally appropriate arts and crafts programme can effectively improve mental health-related quality of life in older Chinese people with chronic pain and depressive symptoms. The engaging and enjoyable process of creating artwork, the tangible nature of art products and the collegiality among group members may contribute to the effects of this programme. These factors may alter pain perception and empower individuals to reshape their narratives around pain, leading to improved coping and well-being. Creative arts-based interventions have great potential and may act as an alternative to pharmacological and CBT-based interventions, particularly in community settings; a definitive trial is needed to reveal the effectiveness of creative arts and crafts in pain management.
Supplementary material
The supplementary material can be found online at https://doi.org/10.1192/bjo.2025.10062
Data availability
The data supporting this study’s findings are available from the corresponding author, T.L., upon reasonable request.
Acknowledgements
We would like to thank all the participants for participating in the pilot study and giving us feedback. We would also like to thank the collaborating aged care centres for their assistance in recruiting participants. We are also grateful to research assistants R. Chan, C. Yeung and C. Lee for their assistance in the co-design process and data collection and analysis.
Author contributions
T.L., G.H.Y.W. and T.Y.S.L. were responsible for the study’s conception and supervision. T.L., H.S.K. and W.-w.K. led the co-design process in phase 1. H.S.K., J.K.Q.L. and D.K.Y.L. undertook data management. T.L., H.S.K. and J.K.Q.L. conducted the data analysis and evaluation. T.L., H.S.K. and J.K.Q.L. wrote the manuscript, with revisions made by D.K.Y.L. and S.M.Y.W. All co-authors reviewed, updated and approved the final manuscript for publication.
Funding
This work is supported by the Hong Kong Jockey Club Charities Trust for The University of Hong Kong for the Project JC JoyAge: Jockey Club Holistic Support Project for Elderly Mental Wellness (HKU Project Codes: AR160026 and AR190017). The funder had no role in the preparation of data or the manuscript.
Declaration of interest
None.









eLetters
No eLetters have been published for this article.