Introduction
The practice of mindfulness is described as paying attention to the present moment. Reference Kabat-Zinn1 Mindful awareness is meant to help transition from a state where thoughts and actions are in automatic mode to a state where situations are observed, acknowledged, and accepted. Reference Weick, Sutcliffe, Obstfeld and A2 A recent systematic review identified that brief mindfulness interventions aimed at healthcare workers (HCWs) improved a myriad of clinical outcomes. Reference Gilmartin, Goyal and Hamati3 Mindfulness practices may help HCWs experience defined as “brief periods of time in which people experience a deep interconnectedness” linked with care of with patients. Reference Pargament, Lomax, McGee and Fang4,Reference Quinn, Fowler and Harrod5
Limited data are available on the impact of mindfulness training on infection prevention (IP) practices. The role modeling of mindful hand hygiene within a clinical setting may have a cascading effect on improving peers adherence to IP practices. Reference Gilmartin6 Further, adoption of mindful practice, may have other benefits including enhanced attention, situational awareness, provider well-being, and reduction of medical errors by addressing cognitive biases. Reference Brown and Ryan7,Reference Sibinga and Wu8 We report the design, execution, and analysis of a quasi-experimental study that evaluated the association of mindfulness training on change in IP practices in 4 intensive care units (ICUs) and the self-reported changes in wellness by participants.
Methods
A quasi-experimental study was conducted to evaluate the impact of mindfulness training in 2 surgical and 2 medical ICUs at Thammasat University Hospital (TUH); all HCWs consented to participation. The study periods consisted of the six-month pre-implementation period (Period 1) from 12/1/2023–5/31/2023 and the six-month post-implementation period (Period 2) from 6/01/2024–11/30/2024. Mindfulness training was conducted by a multidisciplinary team of study investigators and leadership representatives from The Mind Development in Honor of His Majesty the King.
During Period 1, baseline data collection included age, gender, type of unit, occupation, religion, previous mindfulness training, level of faith in religion, stress, anxiety, feeling light and relieved, peace in daily life, and happiness in daily life. The study outcomes included IP practices, report of medical errors, and HCWs self-reported wellness measures. The IP outcomes were compliance with the observed 5-moments hand hygiene (5MHH), compliance to personal protective equipment (PPE) use as a composite score (Appendix 1), and medical errors defined as total errors reported to hospital administration per month (e.g., forgot to discontinue medication, discontinue the wrong medication). The 5MHH observations were performed by Infection Control nurses per the World Health Organization recommendations, Reference Sax, Allegranzi, Chraïti, Boyce, Larson and Pittet9 with at least 50 5MHH observations required monthly for each unit. The five self-reported wellness metrics were level of stress, anxiety, feeling light and relieved, peace in daily life, and happiness in daily life. These wellness metrics were assessed on a 5-point Likert scale and dichotomized with responses of 4 (agree) or 5 (strongly agree) coded as 1 and 0 otherwise and collected at the start of Period 1 and end of Period 2.
During Period 2, participants registered on-line before attending each mindfulness practice session and the sessions began with a 5-minute introduction on how to apply mindfulness in the ICU settings. The trice-weekly 12-minute mindfulness trainings were guided by A.A., P.E., P.H. using 2 video clips developed by The Mind Development in Honor of His Majesty the King (https://www.youtube.com/watch?v=AbAfdJHgKss; https://www.youtube.com/watch?v=DVZTBk6mG84) followed by discussion on mindfulness practice and IP, if questions arise. All mindfulness teachers had a sustained mindful awareness practice of at least three years after initial training with The Mind Development in Honor of His Majesty the King; educational content included mindfulness concepts and integration of the mindfulness training into clinical IP practices to improve 5MHH. Enrolled HCW participants were required to attend at least 1 educational session per week to meet inclusion criteria for the final data analysis. The study was approved by the TUH Institution Review Board.
All analyses were performed using SPSS, version 26 (Armonk, NY). χ 2tests were used to compare categorical variables. Independent t-tests were used for continuous data. All P values were 2-tailed, and P < 0.05 was considered statistically significant. A multivariate analysis was conducted to evaluate factors associated with HCWs self-report of wellness for each study period. Adjusted odd ratios (aORs) and 95% confidence intervals (CIs) were calculated.
Results
Overall, 284 (86.3%) of 329 eligible HCWs in 4 ICUs consented to study participation; 272 HCWs (95.8%) completed full training and met the inclusion criteria for data analysis. The study cohort’s mean age (S.D.) was 31.2 (SD, 8.9) years; the most common self-reported religion was Buddhism and half of participants reported strong faith in their religion. Demographic and baseline characteristics of the study populations are summarized in Table 1.
Table 1. Baseline characteristics of 272 intensive care unit healthcare workers who participated in mindful awareness training
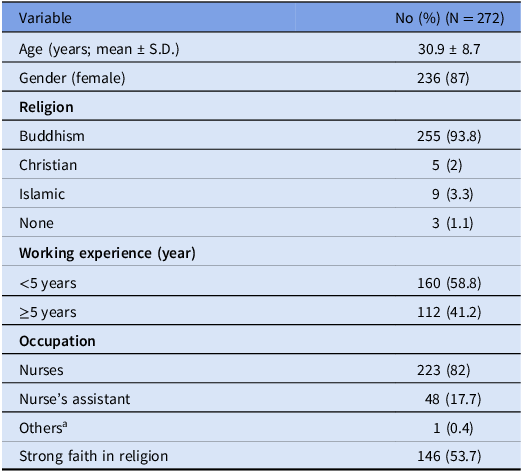
a Housekeeper and ward clerk.
During Period 2, there were significant improvements in the observed IP outcomes and reduction of medical errors (Table 2). There was an increase in the 1st and 4th moments of the 5MHH, improvement in the composite score for full PPE compliance (14.1 (SD, 0.3) vs 13.7 (SD,0.6) points; P = 0.01) and reduction in medical errors (7.9% vs 10.9%; P = 0.04) (Table 2). For the self-reported wellness outcomes, there was a significant reduction in stress (79.8% vs. 67.3%; P = 0.001), reduction in anxiety (76.8% vs. 65.1%; P = 0.003), increased feeling of light and relief (47.1% vs. 58.5%; P = 0.01), increased report of peace in daily life (52.2% vs 62.1%; P = 0.02), and increased report of happiness in daily life (51.5% vs. 61.8%; P = 0.01) (Table 2). In the multivariable analysis, work experience ≥5 years (aOR = 3.21; 1.53–6.71) and strong faith in religion (aOR = 2.64; 95% CI = 1.21–5.76) were associated with improvement in all five self-reported outcomes during Period 2.
Table 2. Comparison of infection prevention practices, medical errors, and wellness outcomes among 272 intensive care unit healthcare workers during the pre- and post-intervention periods
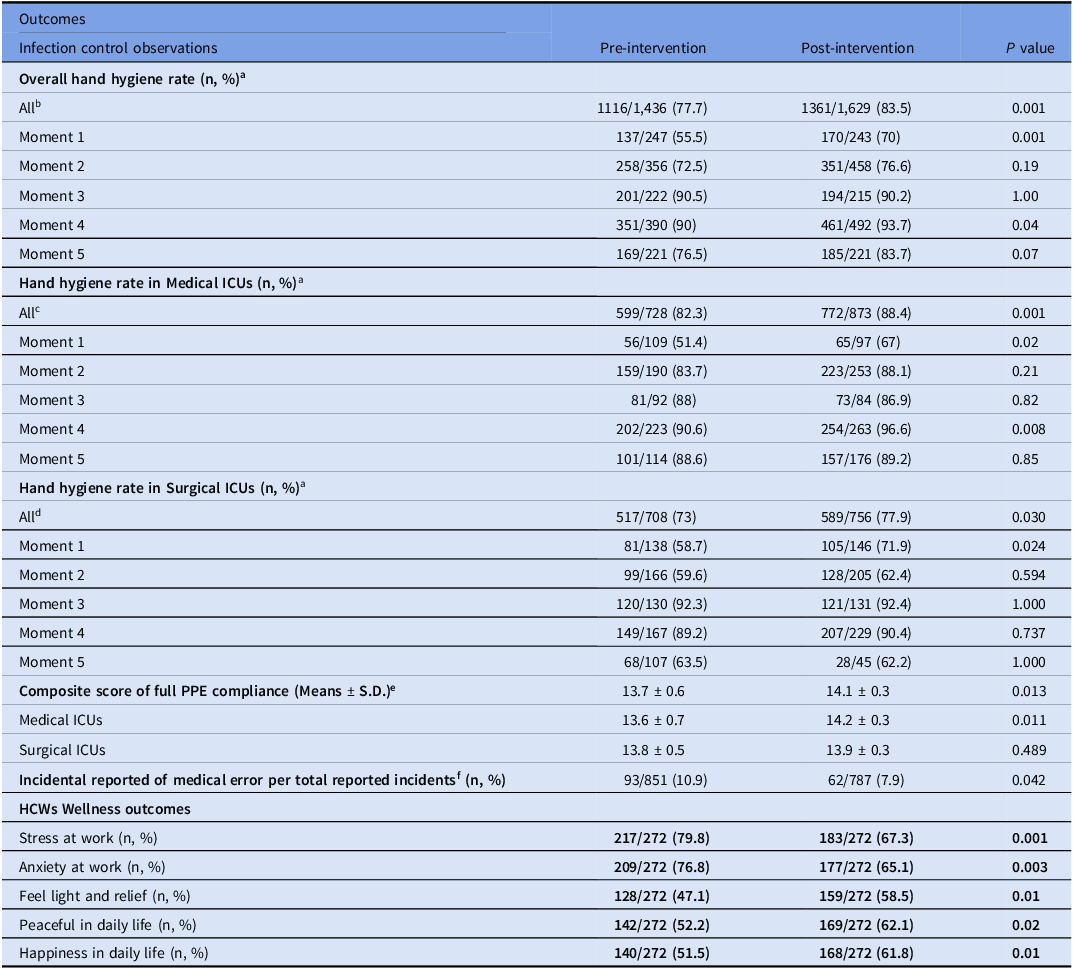
Note: S.D.; standard deviation, ICU; Intensive Care Unit; HCWs = Healthcare workers;
a Hand hygiene performed per total hand hygiene opportunities observed; at least 50 opportunities of observations of overall 5 moments hand hygiene per unit per month are required. The most common type of hand hygiene in ICUs in this hospital using alcohol hand rub.
b OR (0.69 [95% CI, 0.57-0.83], Power = 99.4%), effect size = 0.2.
c OR (0.61 [95% CI, 0.45-0.81], Power = 93.3%), effect size = 0.2.
d OR (0.77 [95% CI, 0.60-0.98], Power = 58.7%), effect size = 0.1.
e Power 98%, effect size 1.2.
f Per total reports, per month.
Discussion
The major finding of this study was the association of mindful awareness training with improvement in three of the 5MHH, use of PPE, reduction in reported medical errors, and an increase in five self-reported wellness measures in a cohort of predominantly ICU nurses. The mindfulness training emphasized being fully aware in the present moment and the measured changes occurred over a six-month interval. Notably, these study findings are consistent with and contribute to the evidence reported in prior ICU HCW studies. Reference Brown and Ryan7,Reference Sibinga and Wu8,Reference Gilmartin, Saint, Rogers, Winter, Snyder, Quinn and Chopra10 Furthermore, our study findings suggest potential differential growth in mindful awareness for HCWs with longer (>5 years) working experiences and self-reported strong faith, adding to an earlier report of improved wellness in HCWs who acknowledged a strong religious faith. Reference Apisarnthanarak, Greene, Collier, Kasatpibal, Fowler and Saint11
Study limitations include the inherent biases associated with quasi-experimental studies for potential Hawthorne effect and temporal changes over the 12-month period. Second, generalizability may be limited given that the study is from a single study site, targeted primarily ICU nurses, and the majority of participants (90%) reported Buddhism as their religious faith. Lastly, the nature of self-report outcomes (e.g., wellness matrix) may subject to reporting biases.
In conclusion, the mindful awareness training was associated with observed increases in IP practices, reduction in medical errors, and higher measures of HCWs’ wellness. The intervention was feasible to implement and to integrate into routine ICU healthcare delivery. Future multi-center randomized-control studies on mindful awareness education and training in different settings will inform on sustained HCW healthy IP behaviors and practices.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ash.2025.174
Financial support
None.
Competing interests
All authors have no conflict of interest to declare.




