Introduction
I took up running in mid-life, having always preferred tennis and squash. But when my father passed away from cancer shortly after his diagnosis, I began to run routinely to clear my head, perhaps subconsciously to manage my grief. Initially, running 2–3 km (under 2 miles) felt like a marathon. Over time, I built up enough stamina to participate in races, starting with 10 km (6.2 miles) and graduated to half-marathons (21.1 km or 13.1 miles). During a recent race, the idea of documenting the lessons I have learned from running that are transferrable to my work in antimicrobial stewardship (AMS) began to formulate. Below are the top five lessons that I hope will resonate with fellow runners and clinicians. See Table 1 for an illustrative example connecting each lesson with implementing or leading an AMS initiative. Let’s lace up our running shoes and get started!
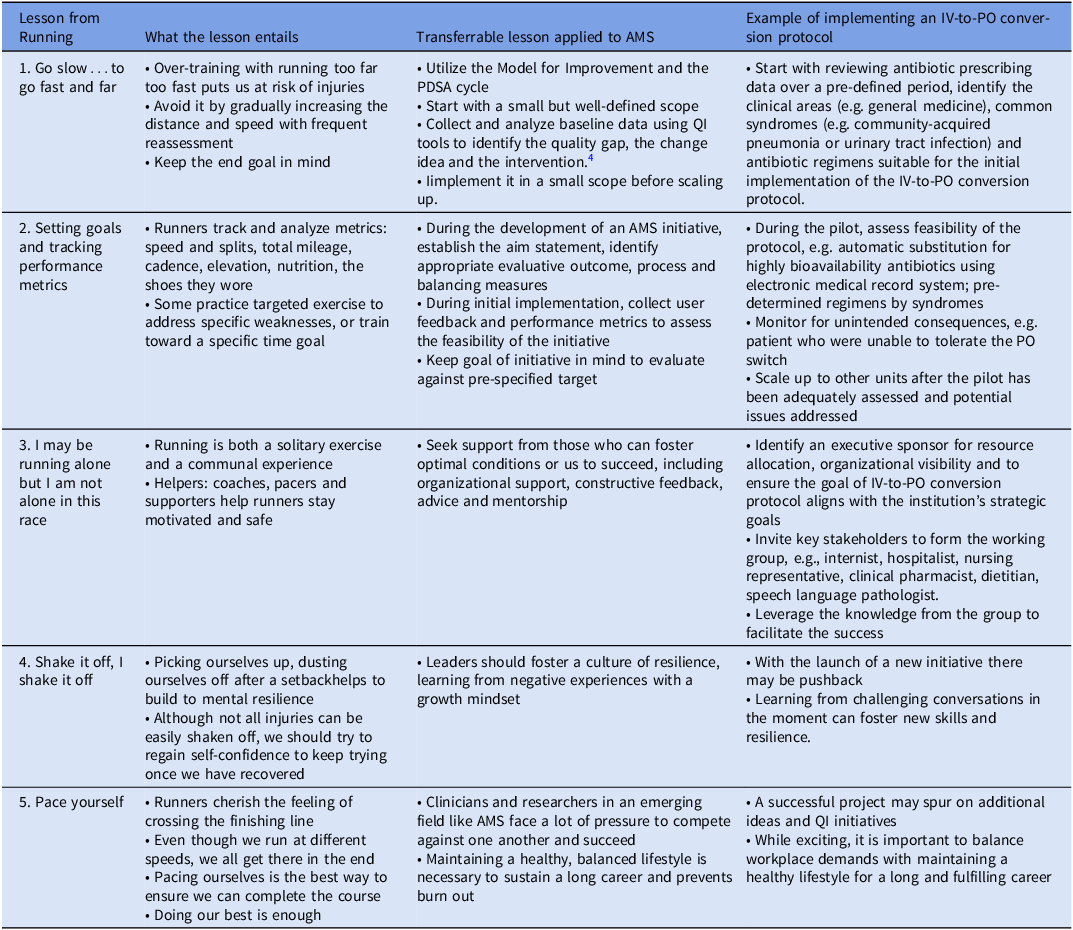
Table 1. Applying the essential lessons I learned from running to leading in antimicrobial stewardship using an illustrative example of implementing an institution-wide antibiotic intravenous-to-oral (IV-to-PO) conversion protocol
Lesson 1: Go slow…to go fast and far
One of the most common mistakes made by enthusiastic but inexperienced runners is running too fast too soon and increasing their mileage too quickly, assuming it will get them ready for a race sooner. But this approach can be counterproductive. Without a plan to condition the body to adapt to the biomechanics of running, overuse injuries such as plantar fasciitis, iliotibial band inflammation (“IT band syndrome”), knee pain and shin splints not only hamper the runner’s progress but also take the joy out of running. Rather, it is more conducive to start at a slower pace and run a shorter distance at first, then gradually increase the speed and distance with the end goal in mind.
This lesson is transferrable to the practice of AMS, which is founded under the auspices of healthcare quality improvement (QI). Reference McGregor, Fitzpatrick and Suda1 As a patient safety initiative, AMS aims to minimize the harms from antimicrobials, promote appropriate use, and mitigate against the emergence of antimicrobial resistance. Reference McGregor, Fitzpatrick and Suda1–Reference Tamma, Miller and Dullabh3 The goal is to maintain the effectiveness of antimicrobials through sustainable improvements in prescribing practices. Under the Model for Improvement, the plan-do-study-act (PDSA) cycle encourages us to first invest the time to gather baseline data, analyze and identify the quality gap, before formulating the change idea and implementing the intervention. 4 The concept of starting with a small but well-defined scope, identifying appropriate evaluative measures a priori, and assessing them adequately before scaling up for widespread impact is applicable to AMS. It also aligns with best practices in project management. 5 Starting with the end point in mind, breaking down a large project (e.g. a new AMS intervention) into manageable steps, each appropriately resourced and monitored by frequent check-ins, help to ensure we are meeting the project milestones. Once an intervention has been refined and finalized, we can apply change management steps to facilitate implementation and adoption. 6 In contrast, launching an initiative at full scale without any planned evaluation cycles may overwhelm key stakeholders such as prescribers, clinicians, patients, caregivers, and the AMS team. Potential consequences include delays, interruptions, missed opportunities, or unintended negative impact on patients and caregivers.
Lesson 2: Setting goals and tracking performance metrics for continuous improvement
Initially, running a short distance felt physically and mentally challenging. To encourage myself, I continuously set small goals with small celebrations: “I will take a walking break after I reach that stop sign” or “I will have a drink of water after running up this hill.” Although trivial, these mini goals were achievable and celebrating those small wins buoyed me. As my endurance increased, the distance between those little goals grew longer. It was the culmination of achieving numerous small goals that got me through my first 10 km race. Additionally, setting a stretch goal – one that is on the cusp of attainability but requires dedicated effort, strategic training, and appropriate nutrition – serves as a long-term motivation for runners. To facilitate continuous improvement, runners are known for meticulously tracking their metrics, hence the burgeoning market of wearable devices and applications to log and analyze our runs. My current stretch goal is to complete a full marathon in a couple of years, having gained more experience with shorter distances. I will be following a training program with varying distance and speed, complemented by strength training and appropriate nutritional support for endurance.
Relating those experiences to leading an AMS program, under the Model for Improvement, establishing a program goal for the team and setting aims are essential to QI initiatives. 4,7 The aim statement may be iterated through each PDSA cycle, but the fundamental domains remain consistent: 1) what is to be improved; 2) by when, i.e. time-bound; 3) by how much, i.e., measurable; 4) valid, i.e. how will one know an improvement has been made; and 5) where one can expect to see the improvement. 7 Therefore, frequently evaluating performance metrics, i.e. outcome, process, and balancing measures appropriate for the AMS interventions facilitates success. 8 Distinct from an aim, the program’s stretch goal should align with the strategic vision of the healthcare institution, yet sufficiently challenging such that the team is encouraged to seek novel change ideas or co-design interventions with stakeholders. 7,Reference Sitkin, See, Miller, Lawless and Carton9,Reference See, Miller and Sitkin10 Akin to appropriate nutritional support, the initiative should be adequately resourced.
Lesson 3: I may be running alone but I am not alone in this race
For many, running is a solitary exercise to unclutter the mind. As I focus on putting one foot ahead of the other, I often come up with solutions to solve problems that have been swirling in my head. Running is also a communal experience. The comraderies from running groups and race participation improve our well-being beyond cardiovascular fitness. At a recent race, I came to appreciate the value of seeking out helpers and supporters, and connected this concept to my role as a leader in AMS. Who are the helpers and supporters? Some runners engage coaches to design strategic, targeted training exercises to improve their performance. At races, pacers are runners who complete the course at a steady pace and finish within a pre-designated time. 11 Pacers are highly visible as they run with a sign that displays their speeds (e.g. “goal time: 4:40; pace: 10:40”) to guide runners at the pre-specified pace. As a group, pacers accommodate participants of different levels. Pacers are my “North Star” in a long-distance race because they help me gauge if I am running too fast or too slow for my capability. First responders are another group of helpers who are vital to the safety of all participants and spectators. Furthermore, I am always thankful for the volunteers handing out thousands of cups of water and energy bars to runners at the aid stations. Finally, spectators who cheer on the side are the biggest morale boosters, crucial in the last few miles of a long race when most runners are fatigued and will appreciate the motivation.
Leading in AMS, be it implementing a specific intervention or heading a full-fledged program, can at times feel like a pressurized, yet lonely endeavor. Seeking helpers and supporters (while avoiding detractors) can have a huge impact on the success of the AMS intervention and the program. It should be emphasized that this does not mean we only surround ourselves with individuals who are uncritical of our decisions or work. Rather, they are individuals who foster optimal conditions to help us succeed, which range from offering organizational support, constructive feedback, advice and mentorship. Reference Gregor, Mulholland and Brydges12 Additionally, as the leader of an AMS program, I consider it my responsibility to be a helper and supporter for team members, providing guidance, accountability and advocacy on their behalf for resources at the organizational level. Reference Bearman13
Lesson 4: “Shake it off, I shake it off!”
During a run last summer, I tripped and fell at the curb as I dashed across an intersection in the remaining seconds of the traffic light. Despite the pain and embarrassment, I quickly got up and moved off the road for safety. As I rinsed off my wounds, Taylor Swift’s popular “Shake It Off” sprang to mind: I must not let it affect my confidence in the upcoming race! Indeed, not all injuries can be shaken off easily, but my mishap prompted me to reflect on how I handled failures and rejections as a clinician, researcher and leader. There is much pressure in today’s culture to project and amplify personal successes, particularly on social media platforms. Surely, one should always celebrate one’s (and each other’s) achievements. But this quote from the American education scholar John Dewey “Failure is instructive. The person who really thinks learns quite as much from his failures as from his successes” encourages us to consider all experiences an opportunity for growth.
Putting this concept into practice, I often recount my early attempts to publish on the impact of AMS audit-and-feedback interventions in patients with acute leukemia to research learners. My manuscript was repeatedly rejected by academic journals, which was devastating as it is a topic I am passionate about, and I poured so much effort into the project. In hindsight, I realized that with each subsequent revision, I gained new knowledge and improved the manuscript for its eventual publication. Resilience, defined as the maintenance or quick recovery of mental health during or after a stressor exposure, emerged as a potential self-protective mechanism for healthcare workers against burnout during the pandemic. Reference Kunzler, Helmreich and Chmitorz14,Reference Grimes, Matlow, Tholl, Dickson, Taylor and Chan15 Healthcare leaders are well-positioned to inculcate resilience among themselves, team members, and promote organizational practices that support resilience within the healthcare system. Reference Gregor, Mulholland and Brydges12,Reference Grimes, Matlow, Tholl, Dickson, Taylor and Chan15,Reference Förster, Duchek, Geithner and Krägler16 Overcoming setbacks, learning from the experience and sharing it with others will help to advance us collectively.
Lesson 5: Pace yourself
All runners at a race share a common goal: to experience the exhilaration of crossing the finish line! Individually, we may be running at different speeds, but we will all get there in the end. As each of us strives to achieve our “PB,” personal best time, it is essential to pace ourselves so that we do not run out of steam before the race is finished or get injured on the course. Furthermore, while runners are competing against one another, the emphasis of “personal best” reminds me that if I have done my utmost, it is sufficient. Relating this concept to leading in an emerging area such as AMS, as clinicians and researchers, we face constant pressure to compete and succeed. Maintaining an openness to learn, keeping a healthy, balanced lifestyle with strong social connections, and developing a positive attitude with self-efficacy will go a long way to sustain a long and impactful career. Reference Förster, Duchek, Geithner and Krägler16
As a clinician, researcher and leader in AMS, there are many demands for my time. To strive for a work-life balance, I prioritize running by scheduling it into my weekly routine. Even running a short distance gives me a fresh perspective and approach to the challenges at work. Conversely, I also use my run to gain new knowledge by listening to podcasts on AMS/infectious diseases (e.g., the ASHE podcast), epidemiology, study design, or topics purely out of interest (e.g., history). I am fortunate that my family understands how important physical activity is to our well-being. It especially hit home during the COVID-19 pandemic, which happened to coincide with my graduate training in public health. Juggling multiple domains that straddle work and life certainly sharpened my focus to guard against mental burnout.
In summary, I have described the five lessons I learned from running and connected them to leading and implementing AMS. I hope this will encourage fellow runners and non-runners alike to share their reflection and insight into what their favorite meditative exercise or hobby has taught them. To the reader, if this commentary prompted you to take up running, a new exercise or hobby, even better. Have fun, be there to support the community and enjoy the camaraderie as you would with fellow stewards. Life is a journey: don’t forget to wave “hello” to each other along the way!
Financial support
I did not receive funding support for the preparation of this manuscript.
Competing interests
I have no relevant conflict of interest to disclose.


