Refine search
Actions for selected content:
65 results
Twenty-five year trend in antipsychotic medication prescribing in England: challenges and opportunities
-
- Journal:
- BJPsych Open / Volume 11 / Issue 4 / July 2025
- Published online by Cambridge University Press:
- 16 July 2025, e151
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Clinicians’ perspectives on a primary healthcare intervention to reduce antibiotic prescription for acute lower respiratory tract infections in Barcelona (Spain): a qualitative study
-
- Journal:
- Primary Health Care Research & Development / Volume 26 / 2025
- Published online by Cambridge University Press:
- 04 July 2025, e54
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Chapter 7 - General Aspects of Psychopharmacology
-
-
- Book:
- Fundamentals of Clinical Psychiatry
- Published online:
- 02 January 2025
- Print publication:
- 16 January 2025, pp 50-63
-
- Chapter
- Export citation
Chapter 2 - Prescribing Practice
-
-
- Book:
- The Frith Prescribing Guidelines for People with Intellectual Disability
- Published online:
- 07 November 2024
- Print publication:
- 21 November 2024, pp 13-30
-
- Chapter
- Export citation
Chapter 1 - Intellectual Disability
-
-
- Book:
- The Frith Prescribing Guidelines for People with Intellectual Disability
- Published online:
- 07 November 2024
- Print publication:
- 21 November 2024, pp 1-12
-
- Chapter
-
- You have access
- HTML
- Export citation
The Frith Prescribing Guidelines for People with Intellectual Disability
-
- Published online:
- 07 November 2024
- Print publication:
- 21 November 2024
Can Medical Licensing Boards Swing the Pendulum Towards Judicious Opioid Prescribing Practices?
-
- Journal:
- Journal of Law, Medicine & Ethics / Volume 52 / Issue 3 / Fall 2024
- Published online by Cambridge University Press:
- 16 December 2024, pp. 690-692
- Print publication:
- Fall 2024
-
- Article
- Export citation
Chapter 58 - Public Health and Pandemic Preparedness
- from Section 5 - Patient Management
-
- Book:
- Clinical and Diagnostic Virology
- Published online:
- 11 April 2024
- Print publication:
- 18 April 2024, pp 292-295
-
- Chapter
- Export citation
2 - Prescribing essentials
-
- Book:
- Handbook of Dental Therapeutics
- Published online:
- 23 February 2024
- Print publication:
- 14 March 2024, pp 25-43
-
- Chapter
- Export citation
Medication Use in the Seniors Population: Optimization of Physician Prescribing as a Means of Preventing Drug-related Illness
-
- Journal:
- Canadian Journal on Aging / La Revue canadienne du vieillissement / Volume 16 / Issue S1 / Spring Printemps 1997
- Published online by Cambridge University Press:
- 08 November 2023, pp. 147-161
-
- Article
- Export citation
Evaluation of a new Perinatal Mental Health Service in a University Maternity Hospital
-
- Journal:
- Irish Journal of Psychological Medicine / Volume 40 / Issue 4 / December 2023
- Published online by Cambridge University Press:
- 26 May 2023, pp. 588-591
- Print publication:
- December 2023
-
- Article
- Export citation
Chapter 6 - Use of Medication and Electroconvulsive Therapy in the Management of Violence
- from Section 2 - Medical and Psychological Intervention
-
-
- Book:
- The Prevention and Management of Violence
- Published online:
- 09 May 2023
- Print publication:
- 11 May 2023, pp 76-106
-
- Chapter
- Export citation
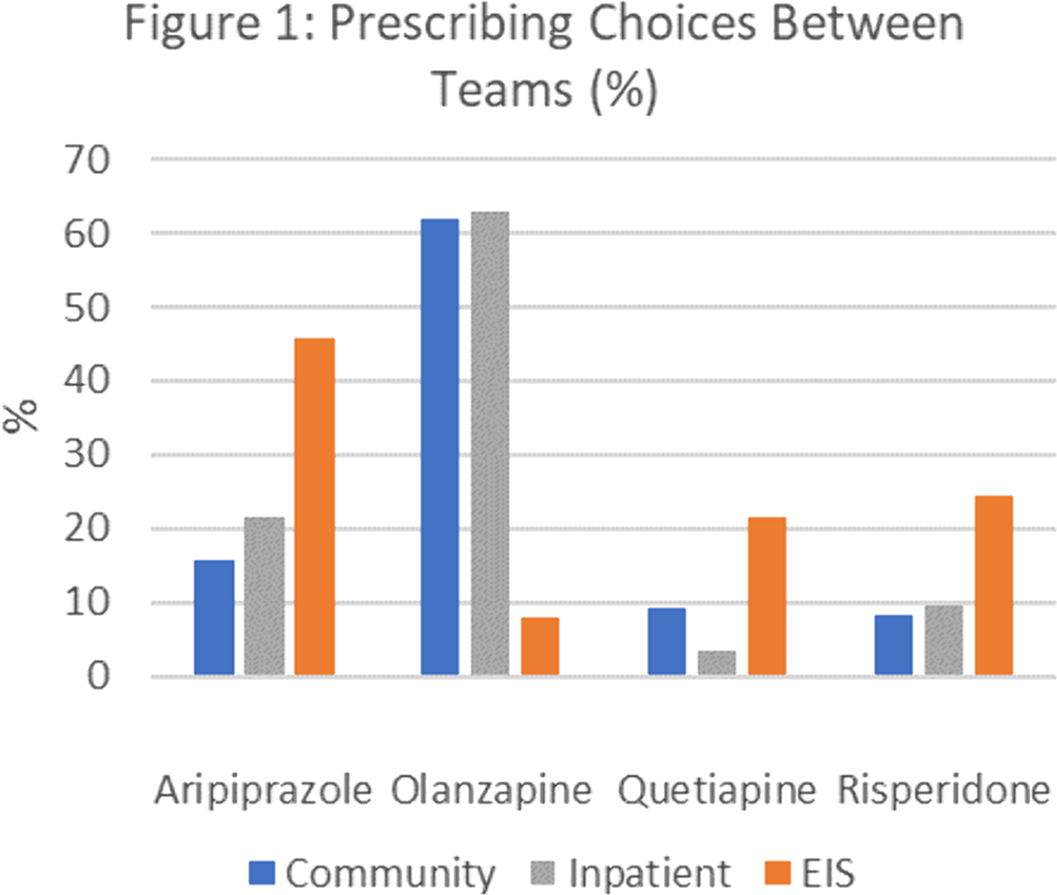
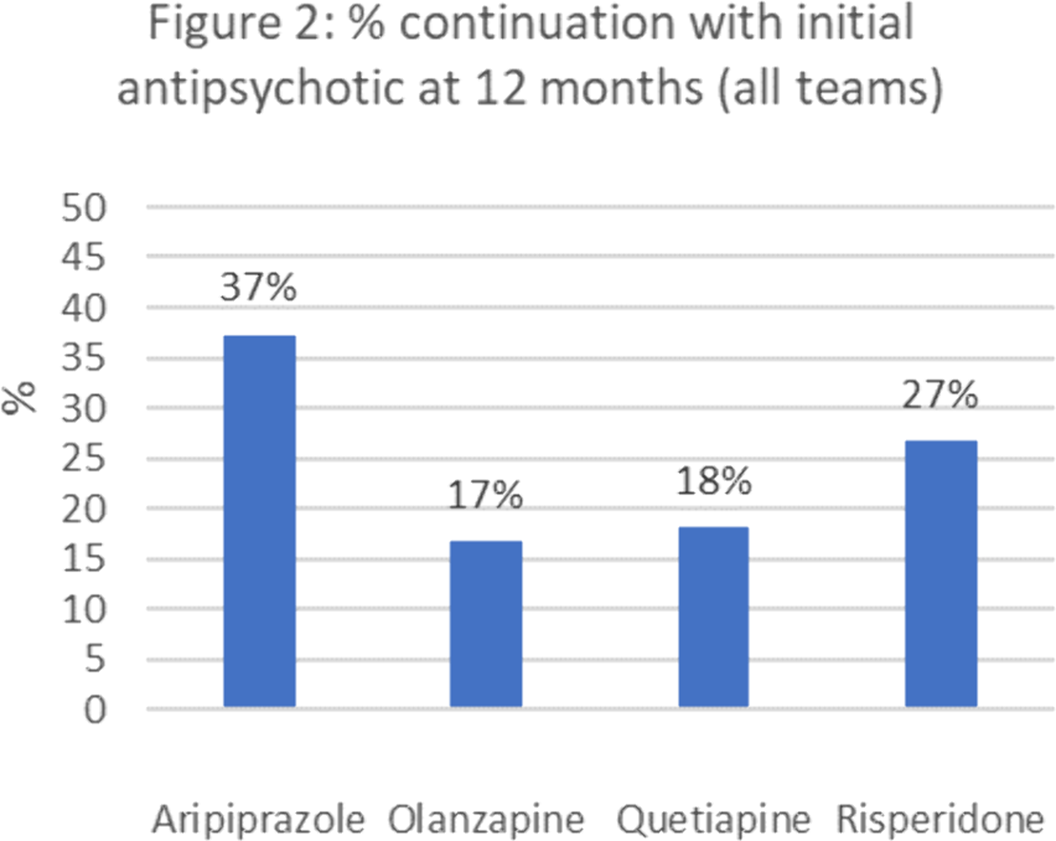
Antipsychotic prescribing choices in patients with First Episode Psychosis
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S285
-
- Article
-
- You have access
- Open access
- Export citation
Case series: propranolol liquid in the treatment of tachyarrhythmias in neonates and infants: potential for errors
-
- Journal:
- Cardiology in the Young / Volume 33 / Issue 3 / March 2023
- Published online by Cambridge University Press:
- 29 June 2022, pp. 482-484
-
- Article
- Export citation
Will this tablet make me happy again? The contribution of relational prescribing in providing a pragmatic and psychodynamic framework for prescribers
-
- Journal:
- BJPsych Advances / Volume 29 / Issue 4 / July 2023
- Published online by Cambridge University Press:
- 17 June 2022, pp. 265-273
- Print publication:
- July 2023
-
- Article
-
- You have access
- HTML
- Export citation
16 - Antimicrobial Prescribing
-
-
- Book:
- Independent and Supplementary Prescribing
- Published online:
- 23 December 2021
- Print publication:
- 13 January 2022, pp 308-320
-
- Chapter
- Export citation
2 - Non-Medical Prescribing in a Multidisciplinary Team Context
-
-
- Book:
- Independent and Supplementary Prescribing
- Published online:
- 23 December 2021
- Print publication:
- 13 January 2022, pp 8-17
-
- Chapter
- Export citation
10 - Evidence-Based Prescribing
-
-
- Book:
- Independent and Supplementary Prescribing
- Published online:
- 23 December 2021
- Print publication:
- 13 January 2022, pp 172-199
-
- Chapter
- Export citation
COVID-19 pandemic impact on psychotropic prescribing for adults with intellectual disability: an observational study in English specialist community services
-
- Journal:
- BJPsych Open / Volume 8 / Issue 1 / January 2022
- Published online by Cambridge University Press:
- 06 December 2021, e7
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Comparison of paracetamol and diclofenac prescribing preferences for adults in primary care
-
- Journal:
- Primary Health Care Research & Development / Volume 22 / 2021
- Published online by Cambridge University Press:
- 02 December 2021, e78
-
- Article
-
- You have access
- Open access
- HTML
- Export citation