Refine search
Actions for selected content:
79 results
The contaminated blood scandal in England: exploring the social harms experienced by infected and affected individuals
-
- Journal:
- Health Economics, Policy and Law / Volume 20 / Issue 4 / October 2025
- Published online by Cambridge University Press:
- 19 August 2025, pp. 381-396
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
A scoping review on the community dividend resulting from testing and treating hepatitis C infection in people living in detention
-
- Journal:
- Epidemiology & Infection / Volume 152 / 2024
- Published online by Cambridge University Press:
- 05 December 2024, e159
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Primary healthcare as a strategy for eliminating hepatitis C: the METRIC toolkit
-
- Journal:
- Primary Health Care Research & Development / Volume 25 / 2024
- Published online by Cambridge University Press:
- 07 November 2024, e61
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Chapter 7 - MicroRNAs Become Medicines
-
- Book:
- Fine-Tuning Life
- Published online:
- 14 June 2024
- Print publication:
- 27 June 2024, pp 175-210
-
- Chapter
- Export citation
Time-to-hepatitis C treatment initiation among people who inject drugs in Melbourne, Australia
-
- Journal:
- Epidemiology & Infection / Volume 151 / 2023
- Published online by Cambridge University Press:
- 09 May 2023, e84
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Chapter 21 - Sexually Transmitted Infections and Pregnancy
- from Section 2 - Specific Issues
-
-
- Book:
- Sex and Pregnancy
- Published online:
- 09 November 2022
- Print publication:
- 27 October 2022, pp 149-164
-
- Chapter
- Export citation
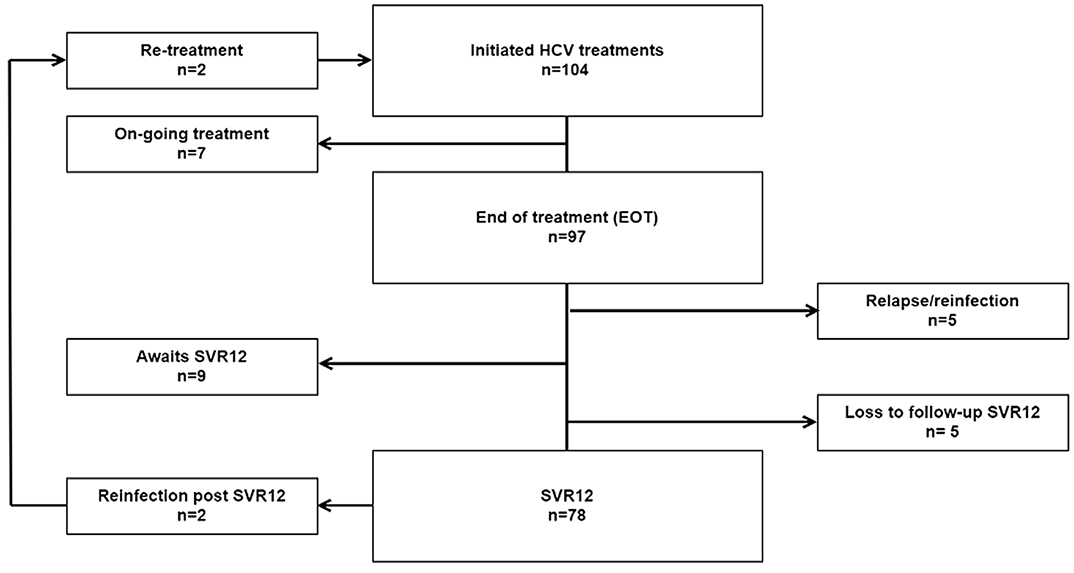
Psychiatrist-led treatment of hepatitis C (HCV) at an opioid agonist treatment (OAT) clinic in Stockholm - enhancing the HCV treatment care cascade
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, pp. S176-S177
-
- Article
-
- You have access
- Open access
- Export citation
Liver function tests in primary care provide a key opportunity to diagnose and engage patients with hepatitis C
-
- Journal:
- Epidemiology & Infection / Volume 150 / 2022
- Published online by Cambridge University Press:
- 27 June 2022, e133
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Real-world monitoring progress towards the elimination of hepatitis C virus in Australia using sentinel surveillance of primary care clinics; an ecological study of hepatitis C virus antibody tests from 2009 to 2019
-
- Journal:
- Epidemiology & Infection / Volume 150 / 2022
- Published online by Cambridge University Press:
- 06 December 2021, e7
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Hepatitis C virus prevalence in Belgium
-
- Journal:
- Experimental Results / Volume 2 / 2021
- Published online by Cambridge University Press:
- 04 October 2021, e29
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Screening for hepatitis C in psychiatric population
-
- Journal:
- European Psychiatry / Volume 64 / Issue S1 / April 2021
- Published online by Cambridge University Press:
- 13 August 2021, pp. S90-S91
-
- Article
-
- You have access
- Open access
- Export citation
Chapter 10 - The Legacies of Belgian Tropical Medicine
-
- Book:
- The Origins of AIDS
- Published online:
- 05 January 2021
- Print publication:
- 21 January 2021, pp 200-232
-
- Chapter
- Export citation
Chapter 9 - The Legacies of French Colonial Medicine
-
- Book:
- The Origins of AIDS
- Published online:
- 05 January 2021
- Print publication:
- 21 January 2021, pp 170-199
-
- Chapter
- Export citation
Chapter 8 - Injections and the Transmission of Viruses
-
- Book:
- The Origins of AIDS
- Published online:
- 05 January 2021
- Print publication:
- 21 January 2021, pp 153-169
-
- Chapter
- Export citation
Maternal hepatitis B or C carrier status and long-term risk for offspring neurological morbidity: a population-based cohort study
-
- Journal:
- Journal of Developmental Origins of Health and Disease / Volume 13 / Issue 1 / February 2022
- Published online by Cambridge University Press:
- 21 January 2021, pp. 115-119
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The transmissibility of hepatitis C virus: a modelling study in Xiamen City, China
-
- Journal:
- Epidemiology & Infection / Volume 148 / 2020
- Published online by Cambridge University Press:
- 25 November 2020, e291
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Numerous outbreaks amongst homeless and injection drug-using populations raise concerns of an evolving syndemic in London, Canada
-
- Journal:
- Epidemiology & Infection / Volume 148 / 2020
- Published online by Cambridge University Press:
- 16 June 2020, e160
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
LO44: Birth cohort hepatitis C screening in an academic emergency department in Canada: preliminary results
-
- Journal:
- Canadian Journal of Emergency Medicine / Volume 22 / Issue S1 / May 2020
- Published online by Cambridge University Press:
- 13 May 2020, p. S23
- Print publication:
- May 2020
-
- Article
-
- You have access
- Export citation
Association of seasonality and serum albumin concentration with vitamin D deficiency in subjects with chronic hepatitis C infection living in a sunny country
-
- Journal:
- Public Health Nutrition / Volume 23 / Issue 7 / May 2020
- Published online by Cambridge University Press:
- 09 March 2020, pp. 1247-1253
-
- Article
-
- You have access
- HTML
- Export citation
Clustering of hepatitis C virus antibody positivity within households and communities in Punjab, India
-
- Journal:
- Epidemiology & Infection / Volume 147 / 2019
- Published online by Cambridge University Press:
- 07 October 2019, e283
-
- Article
-
- You have access
- Open access
- HTML
- Export citation