Historical Background
Public health cannot be understood or fully appreciated without some knowledge of its history. Conventionally, this begins with the large body of work associated with Hippocrates (c. 460–370 BC). In these writings, health was viewed as resulting from a sound balance of the humours. Therapy included diet, exercise and other interventions tailored to the individual – akin to today’s emphasis on healthy living and lifestyle. The Hippocratics were, in addition, early exponents of environmentalism. In ‘Airs, Waters, Places’, the occurrence of disease was linked to such factors as climate, soil and water quality. Proposals for disease prevention were related to specific social and economic circumstances.
Until recently, it was a commonly held view that improvements in health were the result of scientific medicine. This view was based on experience of the modern management of sickness by dedicated health workers able to draw on an ever-growing range of diagnostics, medicines and surgical interventions. The demise of epidemics and infectious disease (until the manifestation of AIDS), the dramatic decline in maternal and infant mortality rates and the progressive increase in the proportion of the population living into old age coincided in Britain with the development of the National Health Service (NHS, established in 1948). Henceforth, good-quality medical care was available to most people when they needed it at no immediate cost. Clearly, there have been advances in scientific medicine with enormous benefit to humankind, but have they alone or even mainly been responsible for the dramatic improvements in mortality rates evident in developed countries in the last 150 years? What lessons can we learn from how these improvements have been brought about?
Public health has been defined as ‘the science and art of preventing disease, prolonging life and promoting health through the organised efforts of society’ [1]. In Europe and North America, four distinct phases of activity in relation to public health over the last 200 years can be identified. The first phase began in the industrialised cities of Northern Europe in response to the appalling toll of death and disease among working-class people who were living in abject poverty. Large numbers of people had been displaced from the land by landlords seeking to take advantage of the agricultural revolution. They had been attracted to growing cities as a result of the industrial revolution and produced massive changes in population patterns and the physical environment in which people lived [Reference Hamlin, Detels, Beaglehole, Lansang and Gulliford2].
The first Medical Officer of Health in the UK, William Duncan (1805–1863), was appointed in Liverpool. Duncan surveyed housing conditions in the 1830s and discovered that one-third of the population was living in the cellars of back-to-back houses with earth floors, no ventilation or sanitation and as many as 16 people to a room. It was no surprise to him that fevers were rampant. The response to similar situations in large industrial towns was the development of a public health movement based on the activities of medical officers of health and sanitary inspectors, and supported by legislation.
The public health movement, with its emphasis on environmental change, was eclipsed in the 1870s by an approach at the level of the individual, ushered in by the development of the ‘germ theory’ of disease and the possibilities offered by immunisation and vaccination. Action to improve the health of the population moved on first to preventive services targeted at individuals, such as immunisation and family planning, and later to a range of other initiatives, including the development of community and school nursing services. The introduction of school meals was part of a package of measures to address the poor nutrition among working-class people, which had been brought to public notice by the poor physical condition of recruits to the army during the Boer War at the turn of the twentieth century.
This second phase also marked the increasing involvement of the state in medical and social welfare through the provision of hospital and clinic services [Reference Hamlin, Detels, Beaglehole, Lansang and Gulliford2]. It was in turn superseded by a ‘therapeutic era’ dating from the 1930s, with the advent of insulin and sulphonamides. Until that time, there was little that was effective in doctors’ therapeutic arsenal. The beginning of this era coincided with the apparent demise of infectious diseases on the one hand and the development of ideas about the welfare state in many developed countries on the other. Historically, it marked a weakening of departments of public health and a shift of power and resources to hospital-based services.
By the early 1970s, the therapeutic era was itself being challenged by those such as Ivan Illich (1926–2002), who viewed the activities of the medical profession as part of the problem rather than the solution. Illich was a Catholic priest who had come to view the medical establishment as a major threat to health. His radical critique of industrialised medicine is simply summarised [Reference Illich3]. Death, pain and sickness are part of human experience and all cultures have developed means to help people cope with them. Modern medicine has destroyed these cultural and individual capacities, through its misguided attempts to deplete death, pain and sickness. Such ‘social and cultural iatrogenesis’ has shaped the way that people decipher reality. People are conditioned to ‘get’ things rather than do them. ‘Well-being’ has become a passive state rather than an activity.
The most influential body of work belonged to Thomas McKeown (1911–1988). He demonstrated that dramatic increases in the British population could only be accounted for by a reduction in death rates, especially in childhood. He estimated that 80–90% of the total reduction in death rates from the beginning of the eighteenth century to the present day had been caused by a reduction in those deaths due to infection – especially tuberculosis, chest infections and water- and food-borne diarrhoeal disease [Reference McKeown4].
Most strikingly, with the exception of vaccination against smallpox (which was associated with nearly 2% of the decline in the death rate from 1848 to 1971), immunisation and therapy had an insignificant effect on mortality from infectious diseases until well into the twentieth century. Most of the reduction in mortality from TB, bronchitis, pneumonia, influenza, whooping cough and food- and water-borne diseases had already occurred before effective immunisation and treatment became available. McKeown placed particular emphasis on raised nutritional standards as a consequence of rising living standards. This thesis was challenged in turn by those who stress the importance of public health measures [Reference Szereter, Davey, Gray and Seale5].
The birth of a ‘new public health’ movement dated from the 1970s [Reference Ashton6]. This approach brought together environmental change and personal preventive measures with appropriate therapeutic interventions, especially for older and disabled people. Educational approaches to health promotion have proved disappointingly ineffective. Contemporary health problems are therefore seen as being societal rather than solely individual in their origins, thereby avoiding the trap of ‘blaming the victim’.
The intriguing truth is that the role of knowledge as a determinant of health is as yet ill defined. Scientific advances in our understanding of how to improve health are embodied in the evolving panoply of medical interventions – new drugs, vaccines, diagnostics, etc. These new insights are, in turn, assimilated more informally by health professionals and the general public. How to harness new knowledge more effectively, for example, through the exploitation of new information technologies and marketing techniques, is a topic of growing interest to students of public health [7].
In the early twentieth century, the decline of childhood mortality was powerfully determined by the propagation to parents of new bacteriological knowledge [Reference Ewbank, Preston, Caldwell, Findley and Caldwell8]. Over the last three decades, increased access to knowledge and technology has accounted for as much as two-thirds of the annual decline in under-5 mortality rates in low- and middle-income countries [Reference Jamison, Jamison, Breman and Measham9]. Knowledge – or rather wilful ignorance – was an important determinant of political responses to the COVID-19 pandemic. The practices of isolation, quarantine and personal protection evolved in the Middle Ages in response to the Black Death. Delays in ‘locking down’ and ineffective systems for tracing disease fatally hampered early control in the UK [Reference Scaly, Jacobson and Abbasi10]. Yet the pandemic also showcased extraordinary technical advances in drug and vaccine development and evidenced remarkable societal compliance with restrictions on individual freedom and risk-reduction measures.
In any event, what is needed to address society’s health problems are rational health-promoting public policies with a sound basis in epidemiology: the study of the distribution and determinants of disease in human populations.
Health-Care’s Contribution in Context
Health professionals have long lived with the ambiguities of their portrayal in literature and the media: on the one hand as compassionate modern miracle-workers, on the other as self-interested charlatans. The implications of McKeown and Illich’s work were largely ignored by clinicians. However, powerful counterarguments have been mounted in their defence.
Attempts have been made to estimate the actual contribution of medical care to life extension or quality of life [Reference Powles, Detels, Beaglehole, Lansang and Gulliford11]. Estimating the increased life expectancy attributable to the treatment of a particular condition involves a three-step procedure:
calculating increases in life expectancy resulting from a decline in disease-specific death rates;
estimating increases in life expectancy when therapy is provided under optimal conditions (using the results of clinical trials, using life tables); and
estimating how much of the decline in death rates can be attributed to medical care provided in routine practice.
Twenty years ago, Bunker credited 5 of the 30-year increase in life expectancy since 1900, and half the 7 years of increase since 1950, to clinical services (preventive as well as therapeutic) [Reference Bunker12]. In other words, compared with the large improvements in life expectancy gained from advancing public health, the contribution of medical care was relatively small, but is now a more significant determinant of life expectancy. The continuing inequalities in health point to further potential for improvement.
There are thus three main approaches to improving the health of the population as a whole and national policy must take into account their strengths and limitations.
Increasing investment in medical care may make the most predictable contribution to reducing death and suffering, but its impact is limited.
The benefits of health promotion and changing lifestyles are less predictable.
Redistribution of wealth and resources addresses determinants of glaring health inequalities, but is of still more uncertain benefit.
Domains of Public Health
Public health in the UK NHS has undergone dramatic changes in recent years. All health professionals require some generalist understanding in this field. Rather fewer will need more advanced skills in support of aspects of their jobs (e.g. health visitors, general practitioners, commissioning managers). This group also includes non-medical professions such as environmental health and allied agencies such as charities and voluntary groups. A small number of individuals will specialise in public health, but this group is expanding. Specialists in public health increasingly hail from non-medical backgrounds.
Nowadays, public health is seen as having three core domains: health improvement, health protection and improving services, with three functions of public health intelligence, academic public health and workforce development underpinning each domain (Figure 1) [13]. All these domains are covered within this book. Each has its own chapter and examples from all three are used to demonstrate how the skills underpinning public health are put into practice.

Figure 1 Domains of public health practice [13].
The disciplines that underpin public health include medicine and other clinical fields, epidemiology, demography, statistics, economics, sociology, psychology, ethics, leadership, policy and management. Public health specialists typically work with many other disciplines whose activities impact on the population’s health. These might, for example, include health-service managers, environmental health officers or local political representatives.
The science of public health is concerned with using these disciplines to make a diagnosis of a population’s, rather than an individual’s, health problems, establishing the causes and effects of those problems, and determining effective interventions. The art of public health is to create and use opportunities to implement effective solutions to population health and health-care problems. This book intends to capture both the art and the science.
Throughout their careers, health-care and allied professionals are presented with opportunities to help prevent disease and promote health. Doctors and nurses, for example, need to look beyond their individual patients to improve the health of the population and later in their careers, many will be involved in health-service management. Health professionals with a clear understanding of their role within the wider context of health and social care can influence the planning and organisation of services. They can help to ensure that the development of health services really benefits patients.
This book seeks to develop for its readers a ‘public health perspective’, asking such questions as:
What are the basic causes of this disease and can it be prevented?
What are the most cost-effective approaches to its clinical management?
Can health and other services be better organised to deliver the best models of practice, such as health-care delivery?
What strategies could be adopted at a population level to ameliorate the burden of this disease?
As we have seen, population approaches to health improvement can be portrayed as in opposition to clinical care. This dichotomy is overstated and, in many respects, clinical and epidemiological skills serve complementary functions. There are parallels between the activities of health professionals caring for individuals and public health workers tending populations (Table 1).
Table 1 Individual and population health – parallels in practice
| Individual | Population |
|---|---|
| Examination of a patient | Community health surveys |
| Drawing up diagnostic possibilities | Assessing health-care needs: setting priorities |
| Treatment of a patient | Preventive programmes, service organisation |
| Continuing observation | Continuing monitoring and surveillance |
| Evaluation of treatment | Evaluation of programmes/services |
Public Health and Today’s NHS
In 2012, Directors of Public Health and their teams moved from within the health sector to the local authorities from whence they originally evolved. (The first Medical Officers of Health began discharging their responsibilities from municipalities in the middle of the nineteenth century.) This placed them closer to those responsible for upstream influences on health (e.g. in housing, transport, leisure and the environment).
The NHS has been the focus for frequent reorganisation, but public health teams continue to play a significant role in the commissioning and management of health-care services. Under the Health and Care Act 2022, 42 Integrated Care Boards were set up as statutory organisations responsible for arranging the provision of local health services and managing the local NHS budget.
In response to the COVID-19 pandemic, the health improvement, prevention and health-care functions of Public Health England moved into the new Office for Health Improvement and Disparities. Health protection functions moved to a new UK Health Security Agency established to strengthen emergency preparedness and protect people from infectious diseases and other health threats (see Chapter 10). The rationale for recent reforms is described further in Chapter 15.
As well as specialised public health practitioners within these settings, the roles of many other professionals involve elements of public health within their role, including, for example (although not limited to):
Environmental health officers – tackling food safety, communicable disease control, healthy environments.
Health visitors and school nurses – child health-care includes important public health work such as encouraging breastfeeding and promoting smoking cessation.
District nurses – care of the elderly includes areas such as ensuring adequate heating and safety in the home.
Voluntary organisations – for example, mental health charities carry out mental health promotion.
Information analysts, epidemiologists, researchers and librarians – these people are key to the ability of public health specialists to use information and evidence to measure and improve health.
Occupational health officers – essential to manipulating the risks to health from our working environments and making individual and structural changes to minimise these.
This book is aimed at all who engage in public health practice, be they a public health practitioner, manager or registrar. Health professionals from medicine, nursing and allied professions, colleagues in local government and those in the voluntary sector will also find useful material applicable to their practice. This book is for anyone who wishes to promote health and well-being, understand wider determinants and societal influences on health, tackle inequalities and improve the quality, coordination and communication of services.
The Structure of This Book
The first section focuses on core skills in public health as outlined in Figure 2. For each step in this process, a chapter offers insight into key concepts and skills required for these disciplines or topics.
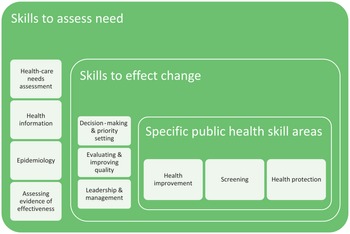
Figure 2 Core skills described in Part 1 of the book.
Chapter 1 focuses on how to assess needs and this is built on in Chapter 2, which outlines sources of health information to inform this. Chapter 3 provides an introduction to the discipline of epidemiology (also the subject of a companion book in this series), and Chapter 4 describes how to use evidence in practice.
The next three chapters build on these fundamental skills and translate them into action: Chapter 5 considers the processes and considerations involved in decision-making and priority setting; Chapter 6 describes methods for evaluation and improving quality of care; and Chapter 7 considers the role of public health practitioners as leaders and managers, and how to widen their influence and deployment of expertise to best effect.
Some specific areas of care are seen as coming under the remit of public health, so the final three chapters in Part 1 offer an introduction to improving population health (Chapter 8), screening (Chapter 9) and health protection (Chapter 10). The toolkit of public health skills a practitioner needs to acquire are added to at each stage and are rarely useful in isolation.
The second half of the book considers the main challenges that public health practitioners are facing and the contexts within which they work. A life-course approach is adopted in Chapters 11, 12 and 13, considering first the specific challenges of child public health before moving on to the health of adults and then older people.
Chapter 14 considers the impact of working in public health on the narrowing of health inequalities; and Chapter 15 covers the role and impact of policy development. Finally, Chapter 16 focuses on international development and Chapter 17 on the crucial role of sustainability and ‘planetary health’.
Figure 3 demonstrates how these public health challenges are connected.

Figure 3 How contexts for and challenges of public health can affect individuals across their whole life course.
Throughout the book, there are questions in the margin to engage the reader, prompt reflection on core material and to encourage you to consider how this knowledge and these skills might be applied to different situations in your own practice. Alongside this book, there is also an Internet Companion (www.cambridge.org/9781107601765), where you will find suggestions for further reading, additional material, interactive exercises and self-assessment questions.