Highlights
-
Minimally invasive surgery (MIS) is safe and effective for cervical meningioma resection in well-selected patients.
-
MIS achieves gross total resection with minimal complications, preserving spinal stability and reducing hospital stay.
-
First combined systematic review and case series to report tumour occupation ratios in MIS-treated cervical meningiomas, highlighting potential clinical relevance.
Introduction
Minimally invasive surgery (MIS) has gained significant importance in the treatment of various spinal pathologies in the last decades. In contrast to traditional open surgical techniques, MIS offers the added benefits of reduced soft tissue manipulation, decreased post-operative pain, lower surgical site infection rates and earlier ambulation. Reference Sharif, Shaikh and Peev1,Reference Hussain, Schmidt, Kirnaz, Wipplinger, Schwartz and Härtl2 The three most commonly employed minimally invasive spine surgery (MISS) techniques are mini-open, tubular (fixed or expandable) and endoscopic. Reference Sharif, Shaikh and Peev1 Each technique has its own advantages, yet all have significantly contributed to enhancing patient care and satisfaction, particularly in lumbar surgery. Reference Sharif, Shaikh and Peev1,Reference Patel, Canseco, Houlihan, Gabay, Grasso and Vaccaro3,Reference Yang, Yang and Zhang4
Tumours arising from the cervical spine present unique challenges in the field of neuro-oncology, due to the presence of vital neurovascular structures, including the vertebral arteries, cervical spinal cord and nerve roots. Reference Peeters, Dessesard Olijnyk, Janelle, Shedid, Bojanowski and Labidi5–Reference Ndongo Sonfack, Bojanowski, Tarabay, Gennari, Shédid and Yuh8 Among such tumours, meningiomas typically present as intradural extramedullary (IDEM) lesions arising from the spinal meninges. Reference Koeller and Shih9 Although benign, they commonly compress surrounding neurovascular structures, leading to significant neurological and vascular complications requiring surgical resection. Reference Frank, Harrop, Hanna and Ratliff10–Reference Almatrafi, Alomair and Alojan13
Given the anatomical challenges and risk of complications with cervical tumours, the objective of this study is to review the current practices regarding minimally invasive surgical management of cervical meningiomas and present a case series of eight patients.
Systematic Review Methods
Eligibility criteria
The methodology of this review adhered to the preferred reporting items for systematic reviews and meta-analysis statement (PRISMA) guidelines and checklist. Reference Page, McKenzie and Bossuyt14 To be included in this systematic review, studies are needed to describe a case of minimally invasive resection of cervical meningioma. Only intradural meningiomas located between the C1 and T2 vertebral levels were included. We included case reports, case series and observational cohort studies that met these criteria. For the purposes of this study, we considered procedures to be MIS if they were performed using open keyhole techniques, fixed tubular retractors, expandable tubular systems or endoscopic approaches, these being widely recognized as standard techniques in MISS. Reference Sharif, Shaikh and Peev1 No time restrictions were applied to the search. Grey literature was also reviewed. Specifically, the Grey literature search involved identifying relevant preprinted articles, even those not yet peer-reviewed, and exploring potential industry-sponsored research. However, we limited our screening to articles written in either English or French. We excluded from the full-text review meningiomas located outside of the cervical spine, conference abstracts, studies with brain tumours other than meningiomas, those that focused on pediatric populations (patients under 18 years old) and studies that did not present a case report or patient-level data (level of surgery, surgical operation, post-op complications, etc.). Patient-level data are further described in depth in the data management and risk of bias assessment of the current methods section. This review was not registered in PROSPERO.
Search strategy
We conducted a literature search across Medline Ovid, PubMed and Embase. This search was executed on June 24, 2024. Our strategy combined keywords and MESH terms pertinent to cervical vertebrae [MESH], nervous system neoplasms [MESH] and minimally invasive surgical procedures [MESH]. We linked these concepts using the Boolean operator AND. We also searched titles, abstracts and keyword sections for terms synonymous with the MESH keywords. Some of the terms we looked for include cervical spine, MIS, brain tumours and meningiomas. It is worth noting that we utilized two different search strategies for each database: one to include all tumours in the cervical region and another specifically targeting cervical meningioma. This approach allowed us to conduct a thorough search, ensuring that no relevant data was missed. Our search strategies were verified by a reference medical librarian. Details of the search strategies and outcomes from Medline, PubMed and Embase are provided in Appendices A, B and C respectively.
Data extraction and risk of bias assessment
All articles exported from each database were processed through the Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). 15 Two independent reviewers reviewed the results according to predefined inclusion and exclusion criteria. Articles that passed this preliminary screening were subjected to a full-text review to confirm their relevance. In cases of disagreement between the primary reviewers, a third independent reviewer was consulted to resolve the discrepancies.
For data extraction, we provided a codification guide, with two reviewers independently carrying out the extraction. For every qualifying article, we extracted the following details: primary author, year of study, number of patients with meningioma included in the study, age, sex, clinical presentation, duration of symptoms, tumour location, site of dural attachment, tumour occupation ratio (defined as the percentage of the spinal canal occupied by the tumour on axial MRI at the level of maximal compression), surgical approach, extent of tumour resection, Simpson grade of resection, meningioma pathology/World Health Organization (WHO) grade, post-operative complications, symptoms improvement, length of stay (LOS) and tumour recurrence. The main goal was to understand the chosen surgical approach by the original authors and to highlight the primary challenges and limitations they encountered during their case management.
We evaluated the risk of bias in individual studies using the Joanna Briggs Institute (JBI) Critical Appraisal tools for case series Reference Munn, Barker and Moola16 and case reports. Reference Moola, Tufanaru and Aromataris17 These checklists can be found in Appendices D and E respectively. As our primary outcome was qualitative in nature, we carried out a narrative synthesis of our findings.
Case Series Methods
These cases were written in accordance with the Preferred Reporting of Case Series in Surgery (PROCESS) guidelines. Reference Mathew, Sohrabi, Franchi, Nicola, Kerwan and Agha18
Patient population
A retrospective case series was conducted at our centre. Adult patients with cervical IDEM meningiomas who underwent treatment using MIS techniques between July 2020 and July 2024 were included. Patients with recurrent tumours or IDEM lesions other than meningiomas were excluded from this study. As the focus was on cervical and cervicothoracic tumours, those below T2 were excluded. We examined the safety and surgical profile of our MIS approach for cervical meningiomas in comparison to the existing literature. We identified key patient characteristics that made these patients suitable candidates for surgical resection using MIS. Additionally, the illustrative surgical management of one patient was presented. This project was a part of an internal quality assessment initiative.
Surgical technique
All patients were managed by the same microsurgical technique using a fixed tubular retractor as described below. After the patient was brought into the operative room (OR), a WHO timeout was performed. The patient received general anaesthesia via endotracheal intubation, and the patient’s positioning on the operating table was the standard prone positioning used for cervical laminectomy. An intravenous access used for fluid and medication administration, a urinary catheter, and intermittent compression leg sleeves were placed. The patient received cefazolin preoperatively and 10 mg dexamethasone. The patient’s head was secured with a Mayfield clamp, and all sensitive areas were well protected. Fluoroscopy was brought into the OR and used to identify the midline and target cervical level. The skin was cleaned with chlorhexidine, and sterile drapes were installed in a standard fashion. Skin incision was performed 2.5 cm lateral to the midline on the appropriate side. The fascia was identified and incised, and sequential tubular dilators were used to split the muscle fibres. A fixed 21 mm spotlight tubular retractor was then positioned for operative access. Final positioning was confirmed with fluoroscopy. The surgical microscope (Zeiss Pentero) was brought in for the remainder of the procedure for standard microsurgical technique. The remaining soft tissue was cauterized and removed to expose the ipsilateral lamina. Laminotomy or hemilaminectomy was performed as required, taking great care to avoid disruption of the facet joints laterally. Identification and resection of ligamentum flavum exposed the dura mater, which was incised with a beaver blade and microsurgical hook. The dural borders were suspended with 4-0 Nurolon sutures. The tumour was identified and dissected away from surrounding cord, rootlets, and its arachnoid covering, with debulking performed as necessary with the ultrasonic aspirator. Once the tumour could be mobilized and its cranial and caudal edges were clearly delineated, final dissection from its dural attachment was performed and the tumour was removed. The underlying dura was coagulated. Spinal cord pulsation and expansion after tumour removal were sought. The dura was closed in a watertight fashion using either 4-0 Nurolon sutures or vascular clips. The fascia was closed with an absorbable 0 Vicryl suture, and the subcutaneous layer closed with 2-0 Vicryl sutures. The skin was closed using various techniques ranging from a subcuticular 4-0 monocryl suture to staples or steristrips, and a Medpore dressing was placed.
An exemplary case describing the aforementioned surgical technique will be submitted as a surgical video article.
Review Results
Study selection
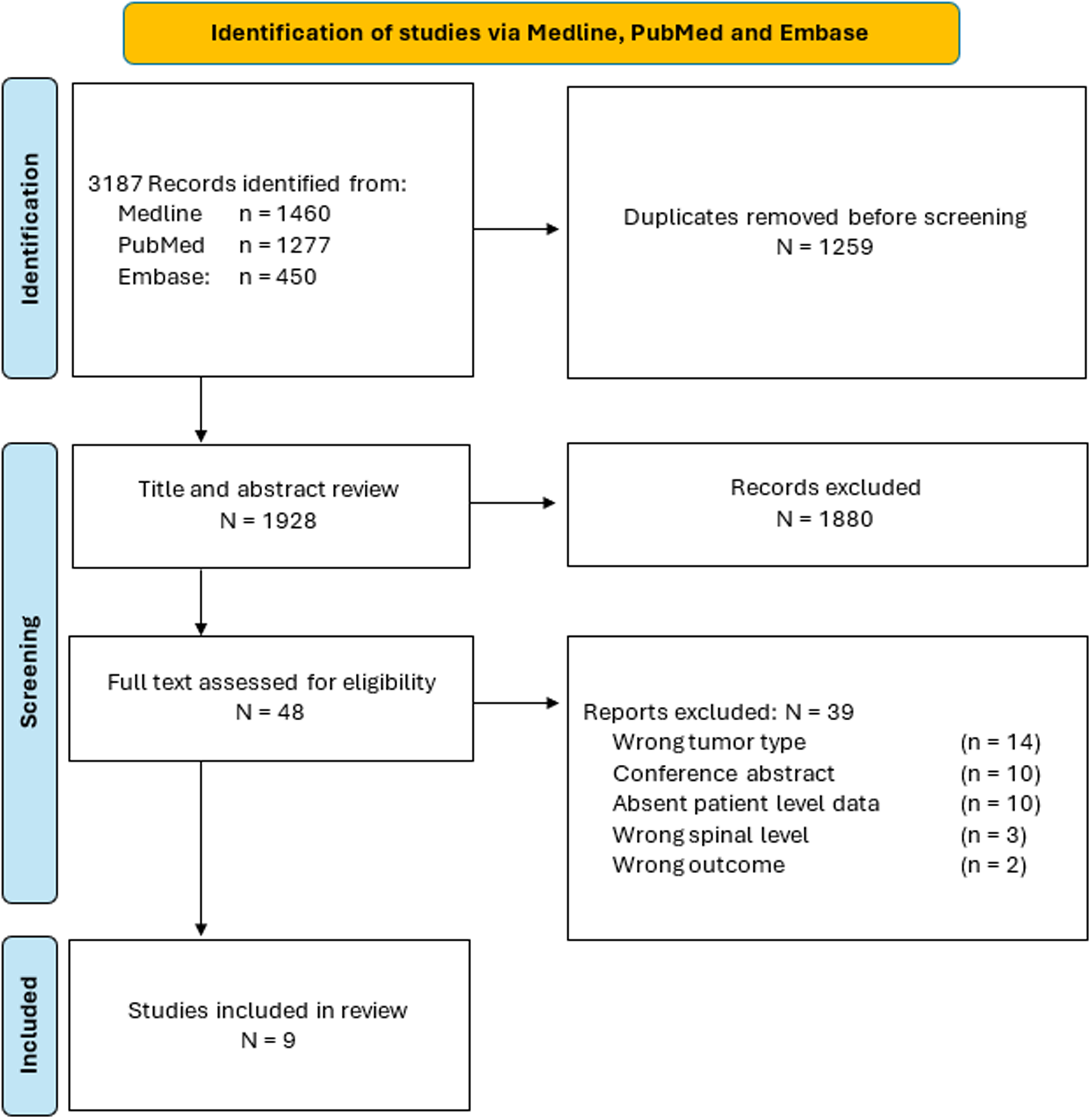
The search strategy yielded a total of 3187 articles from all databases. This number reflects the combined results of two distinct search strategies: one broad strategy including all intradural spinal tumours and another specifically targeting meningioma. From those, 1259 duplicates were removed (Figure 1). The search in Grey literature yielded no articles. During the title and abstract screening process, 1880 records were excluded and 48 were retained for full-text assessment. Of those, 39 were disqualified as they did not meet the inclusion criteria. Therefore, a total of 9 studies were included in this review.
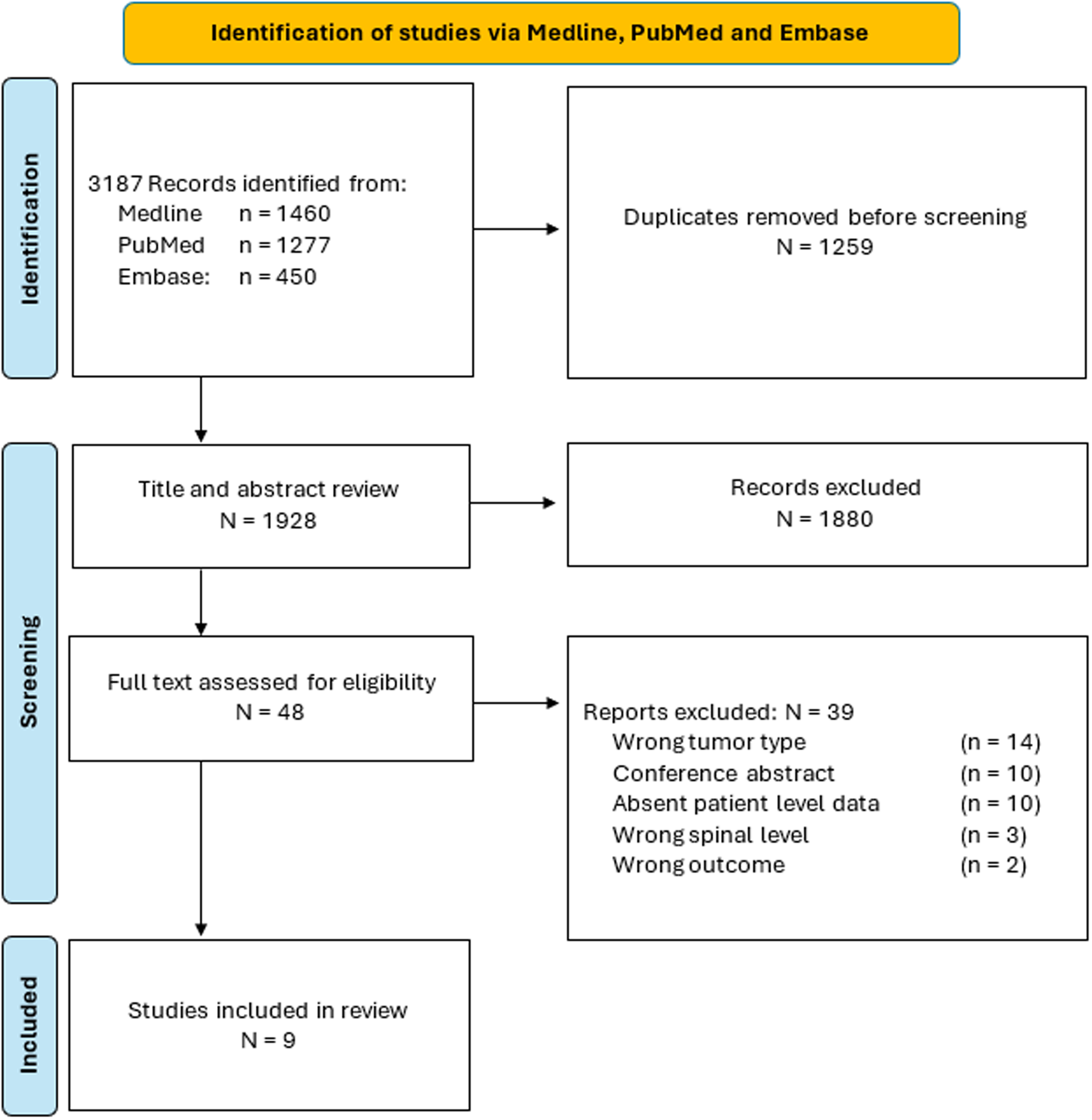
Figure 1. PRISMA flow chart of article selection process from the Medline, PubMed and Embase databases.
Patient characteristics
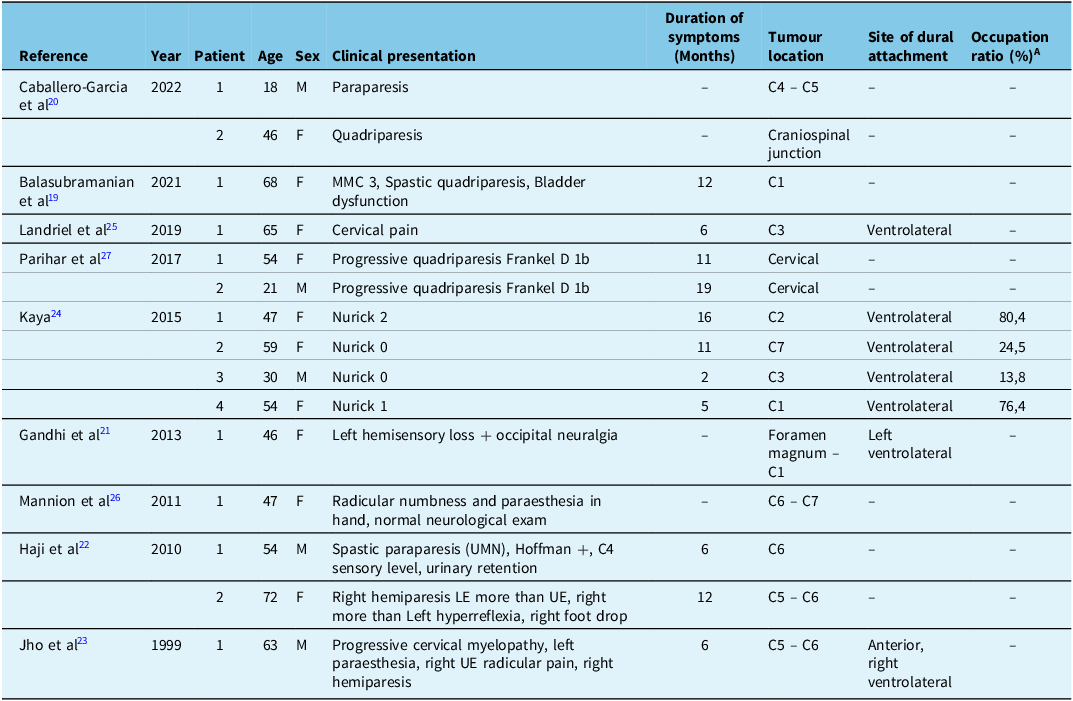
The patient’s demographic data gathered from the articles included in this review are described in detail in Table 1. A total of 15 patients were identified across the 9 included articles. Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19–Reference Parihar, Yadav, Yadav, Ratre, Bajaj and Kher27 Most patients presented with symptoms related to the spinal cord or nerve root involvement. Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19–Reference Kaya24,Reference Mannion, Nowitzke, Efendy and Wood26,Reference Parihar, Yadav, Yadav, Ratre, Bajaj and Kher27 However, two of the four patients from the study by Kaya et al. had a Nurick score of 0, indicating they exhibited no spinal root or cord symptoms. Reference Kaya24 In the latter, no details are provided on how these two patients – patient 2, a 59-year-old female, and patient 3, a 30-year-old male – were identified as potentially having a cervical tumour. Reference Kaya24 That said, Kaya et al. was the only study among the nine to report a tumour occupation ratio. Reference Kaya24 This ratio was determined by measuring the greatest tumour size relative to spinal canal size (cm Reference Hussain, Schmidt, Kirnaz, Wipplinger, Schwartz and Härtl2 ) on axial cross-sections using a gadolinium-enhanced T1-weighted MRI. Reference Kaya24 Notably, the tumour occupation ratios of aforementioned patients 2 and 3, were 24.5 and 13.8, respectively, significantly lower than those of patients 1 and 4 from the same study, which were 80.4 and 76.4 respectively. Reference Kaya24 Among the nine studies, the duration of symptoms before surgery ranged from 2 to 19 months. Reference Kaya24,Reference Parihar, Yadav, Yadav, Ratre, Bajaj and Kher27 Most of the tumours were located at the craniospinal junction/foramen magnum–C1 region, Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19–Reference Gandhi and German21,Reference Kaya24 with the next most common location being the C6 vertebra. Reference Haji, Cenic, Crevier, Murty and Reddy22,Reference Jho and Ha23,Reference Mannion, Nowitzke, Efendy and Wood26 Interestingly, among the four studies that reported the site of dural attachment, all the tumours were found to have a ventrolateral dural attachment. Reference Gandhi and German21,Reference Jho and Ha23–Reference Landriel, Hem, Vecchi and Yampolsky25
Table 1. patient’s demographic data gathered from the articles included in the review process
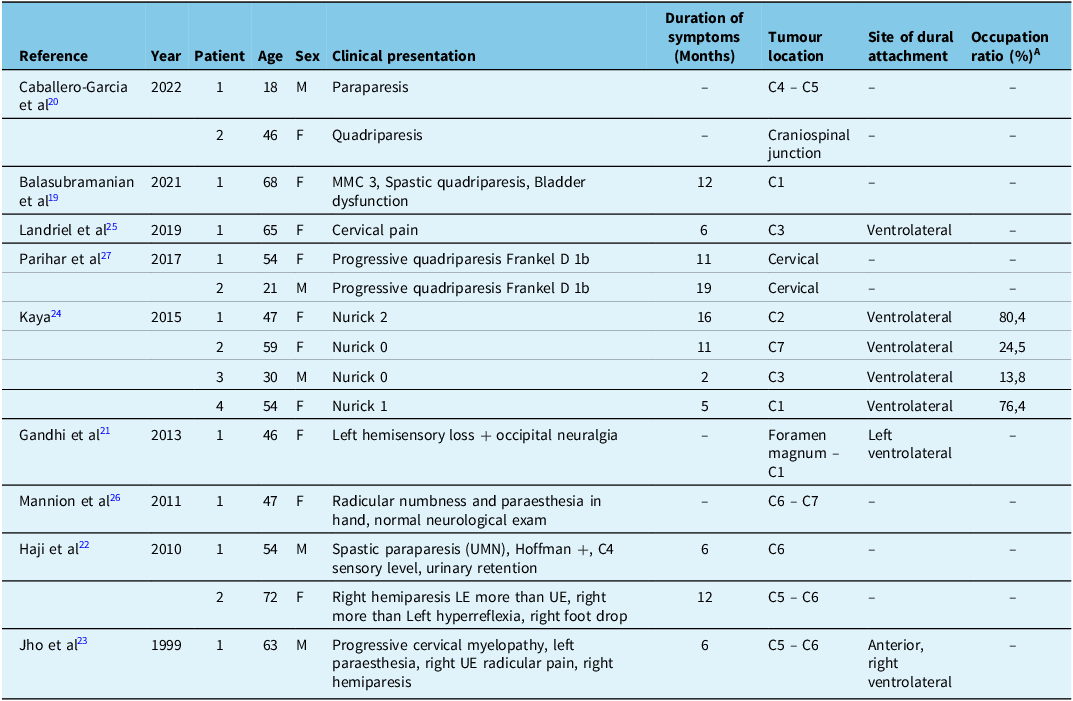
(-) describes data not available ; F = Female ; LE = Lower Extremities ; M = Male ; MMC = Modified McCormick scale ; UE = Upper Extremities ; UMN = Upper Motor Neurone ; VAS = Visual Analogue Scale.
A : Percentage of the spinal canal occupied by the tumour on axial MRI at the level of maximal compression.
Surgical and operative data
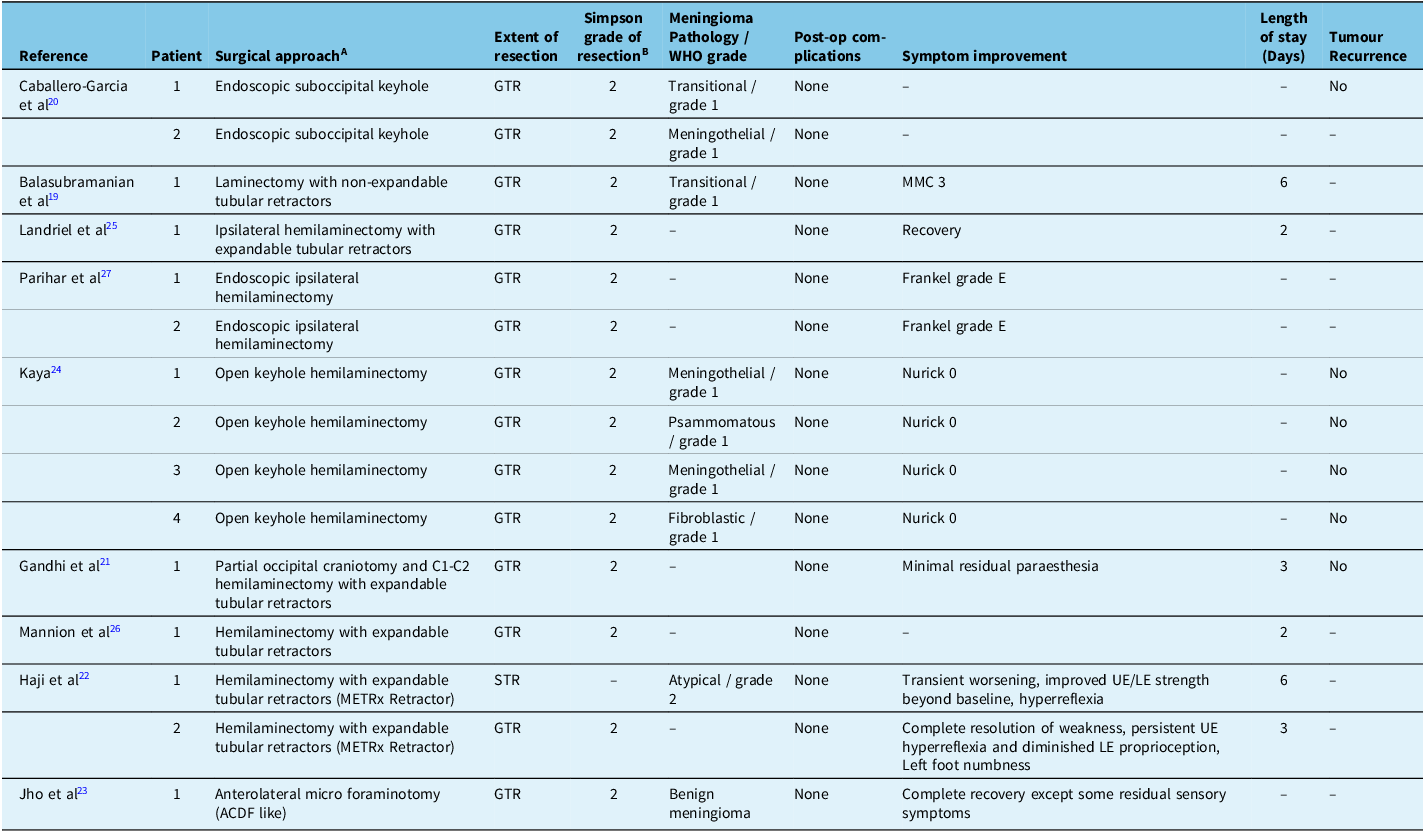
Surgical and operative data gathered from the articles included in this review are thoroughly described in Table 2. Among the nine studies, five favoured an MIS approach with tubular retractors (expandable + non-expandable), Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19,Reference Gandhi and German21,Reference Haji, Cenic, Crevier, Murty and Reddy22,Reference Landriel, Hem, Vecchi and Yampolsky25,Reference Mannion, Nowitzke, Efendy and Wood26 while two studies opted for endoscopic method Reference Caballero-Garcia, Linares-Benavides, Leitao, Aparicio-Garcia and Lopez-Sanchez20,Reference Parihar, Yadav, Yadav, Ratre, Bajaj and Kher27 and another two opted for mini-open/keyhole techniques. Reference Jho and Ha23,Reference Kaya24 Among the 15 patients, gross total resection (GTR) was achieved in 14 of them, Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19–Reference Parihar, Yadav, Yadav, Ratre, Bajaj and Kher27 while one patient underwent a subtotal resection (STR). Reference Haji, Cenic, Crevier, Murty and Reddy22 We carefully reviewed the extent of resection reported by the authors in each of the included articles and determined that a Simpson grade 2 resection was achieved in 14 out of 15 patients. Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19–Reference Parihar, Yadav, Yadav, Ratre, Bajaj and Kher27 Of the nine studies included, five reported the WHO grade of their meningiomas. Among these, three identified grade 1 meningiomas, Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19,Reference Caballero-Garcia, Linares-Benavides, Leitao, Aparicio-Garcia and Lopez-Sanchez20,Reference Kaya24 one reported a grade 2, Reference Haji, Cenic, Crevier, Murty and Reddy22 and one described a benign meningioma. Reference Jho and Ha23 None of the 15 patients across the nine studies experienced post-operative complications, and most patients either fully recovered or had only minor residual symptoms following surgery. Among the five studies that reported LOS after surgery, the duration ranged from two to six days. Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19,Reference Gandhi and German21,Reference Haji, Cenic, Crevier, Murty and Reddy22,Reference Landriel, Hem, Vecchi and Yampolsky25,Reference Mannion, Nowitzke, Efendy and Wood26 Three studies Reference Caballero-Garcia, Linares-Benavides, Leitao, Aparicio-Garcia and Lopez-Sanchez20,Reference Gandhi and German21,Reference Kaya24 reported no tumour recurrence at follow-up visits ranging from 6 to 22 months, while the others did not provide information on this matter.
Table 2. Operative data gathered from the articles included in the review process
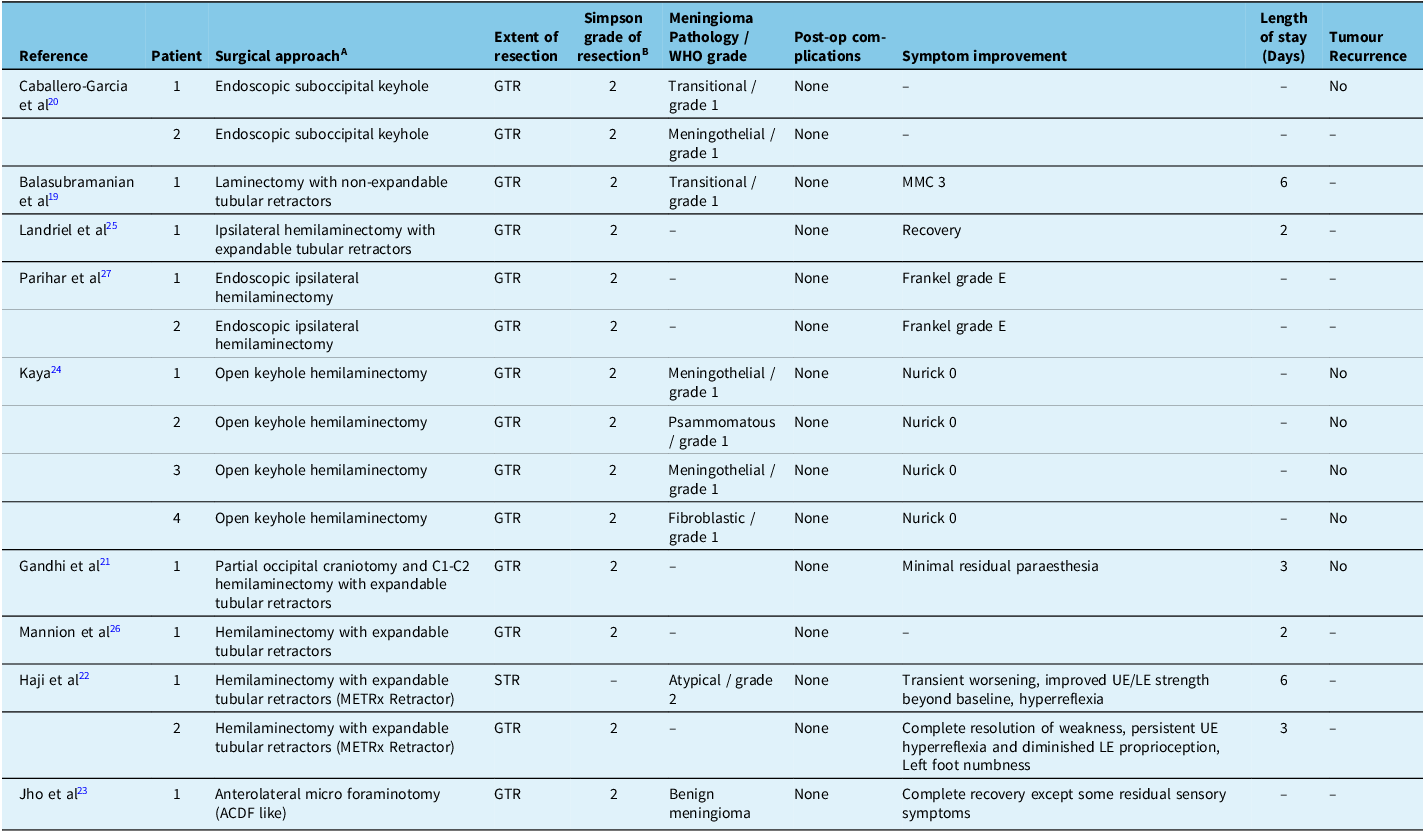
(-) describes data not available ; ACDF = Anterior Cervical Discectomy and Fusion ; GTR = Gross Total Resection ; LE = Lower Extremities ; MMC = Modified McCormick scale ; STR = Sub Total Resection ; UE = Upper Extremities ; VAS = Visual Analogue Scale ; WHO = World Health Organization.
A All posterior lateral approach, to preserve midline structures, unless specified otherwise. B Simpson grade correlates degree of meningioma resection with symptomatic recurrence. Since authors performed a GTR, a Simpson grade 2 was presumed unless otherwise specified.
Risk of bias assessment
All of the nine studies were evaluated as having a low risk of bias. Reference Balasubramanian, Nair, Saphiya, Madan and Mathews19–Reference Haji, Cenic, Crevier, Murty and Reddy22,Reference Kaya24–Reference Parihar, Yadav, Yadav, Ratre, Bajaj and Kher27 As such, the narrative synthesis and conclusions of this review remained unaffected. The risk of bias in each study is described in Appendices F and G.
Illustrative Case Series
Patient characteristics
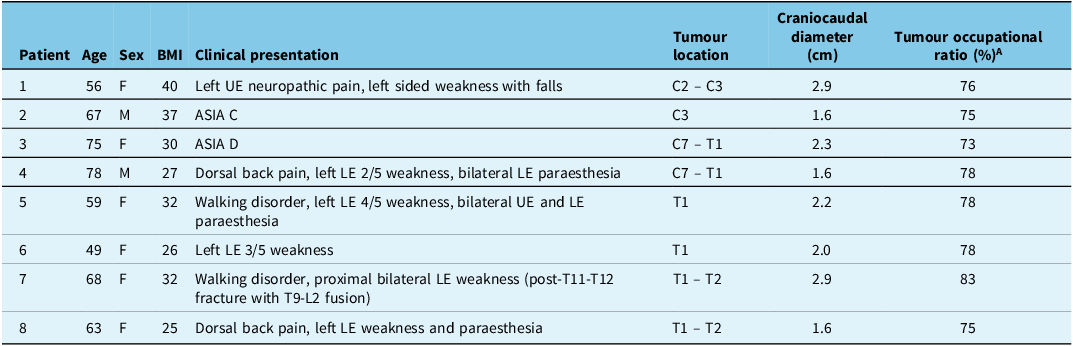
Between July 2020 and July 2024, eight patients with cervical meningiomas were managed by MIS. The demographic details of the patients included in this case series are presented in Table 3. They were mostly female (6 females and 2 males), with a mean and median age of 64 years old. The average BMI in our patient population was 31. Tumour location primarily involved the T1 vertebrae with an average craniocaudal diameter of 2.1 cm. Tumour occupation ratio in our patient population ranged from 73 to 83% with a mean and median value of 77%.
Table 3. demographic data of the patients included in our series
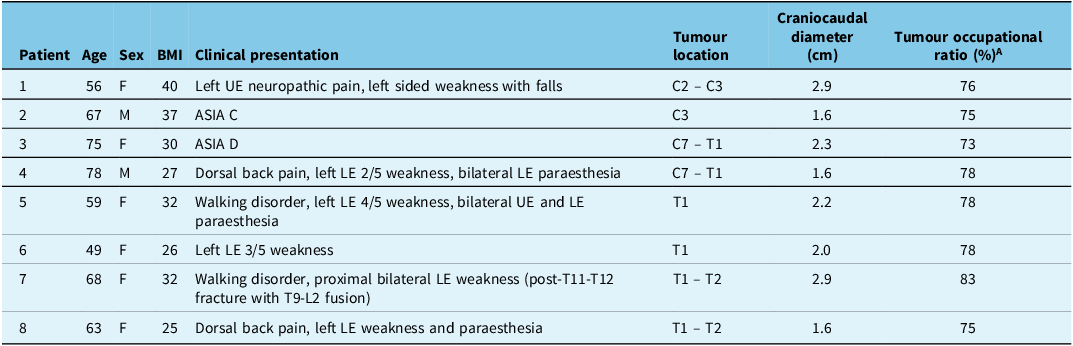
(-) describes data not available ; ASIA = American Spinal Injury Association ; BMI = Body Mass Index ; F = Female ; LE = Lower Extremities ; M = Male ; MIS = Minimally Invasive Surgery ; UE = Upper Extremities.
A : Percentage of the spinal canal occupied by the tumour on axial MRI at the level of maximal compression.
Surgical and operative data
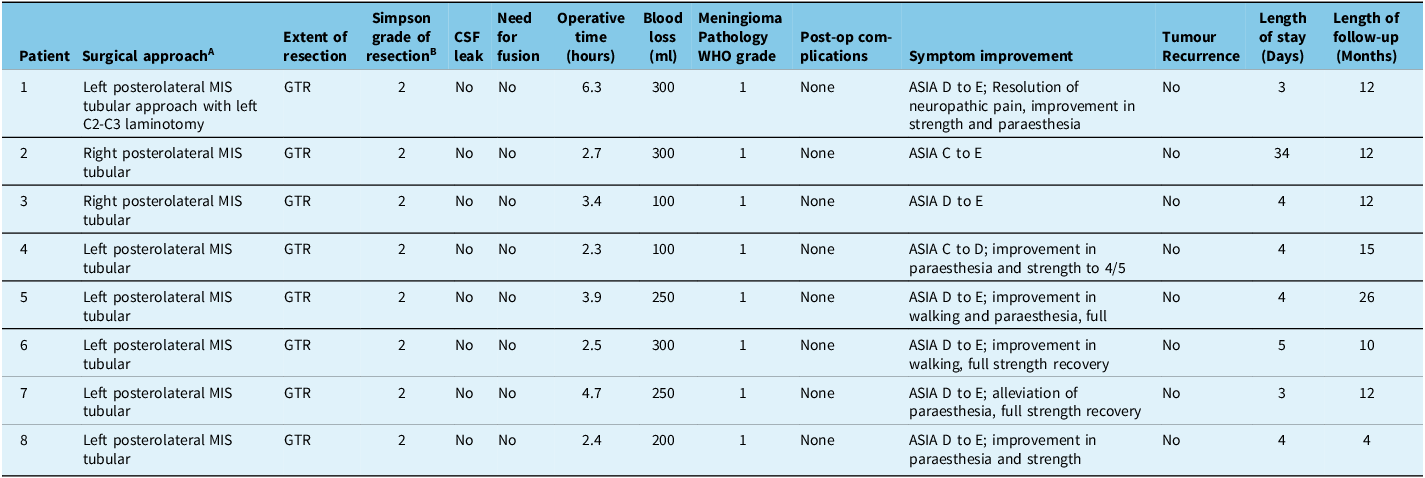
The surgical and operative data of the patients included in this case series are presented in Table 4. All our patients were treated using fixed tubular retractors and achieved GTR. There were no instances of post-operative cerebrospinal fluid (CSF) leaks, and fusion was not required in any of our patients. Mean operative time was 3.5 hours with minimal blood loss. All our patients had a grade 1 meningioma. There were no intraoperative or post-operative complications. Neurological function improved in all our patients. There was no tumour recurrence during a mean follow-up of 12.875 months. The mean LOS was 3.9 days when excluding patient two, as he was deemed suitable for post-operative in-house rehabilitation after full evaluation by our multidisciplinary team. When patient two is included in the analysis, the mean LOS was 7.6 days and the median 4.0 days. We observed no major neurological complications nor neurological deterioration.
Table 4. Operative data of the patients included in our series
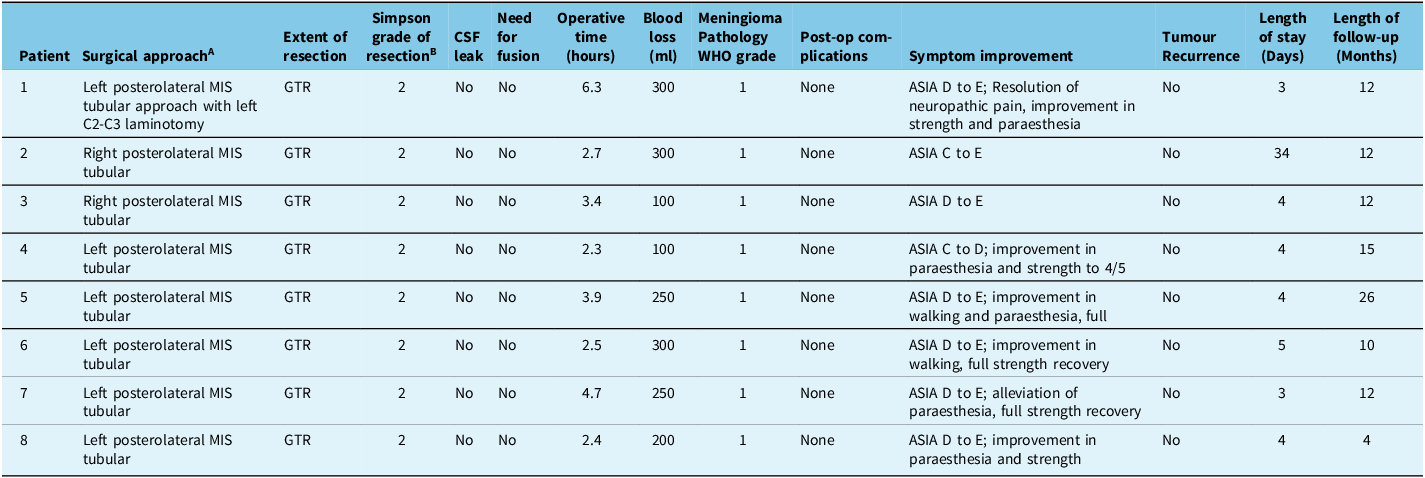
(-) describes data not available ; ASIA = American Spinal Injury Association ; CSF = Cerebrospinal Fluid ; GTR = Gross Total Resection ; MIS = Minimally Invasive Surgery ; WHO = World Health Organization.
A All posterior lateral approach, to preserve midline structures, unless specified otherwise. All procedures were performed under neuromonitoring. BSimpson grade correlates degree of meningioma resection with symptomatic recurrence
Illustrative surgical case: patient 1
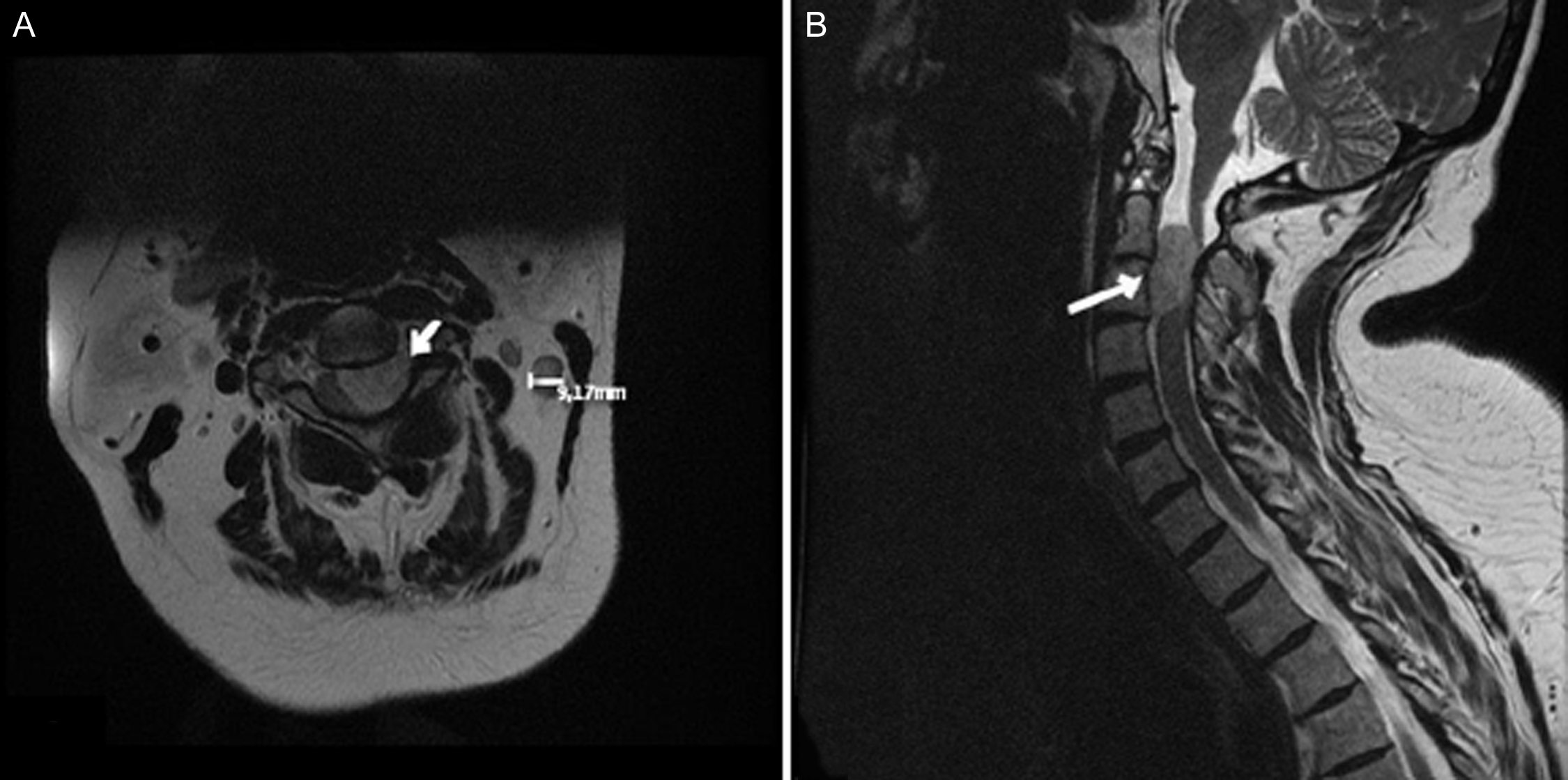
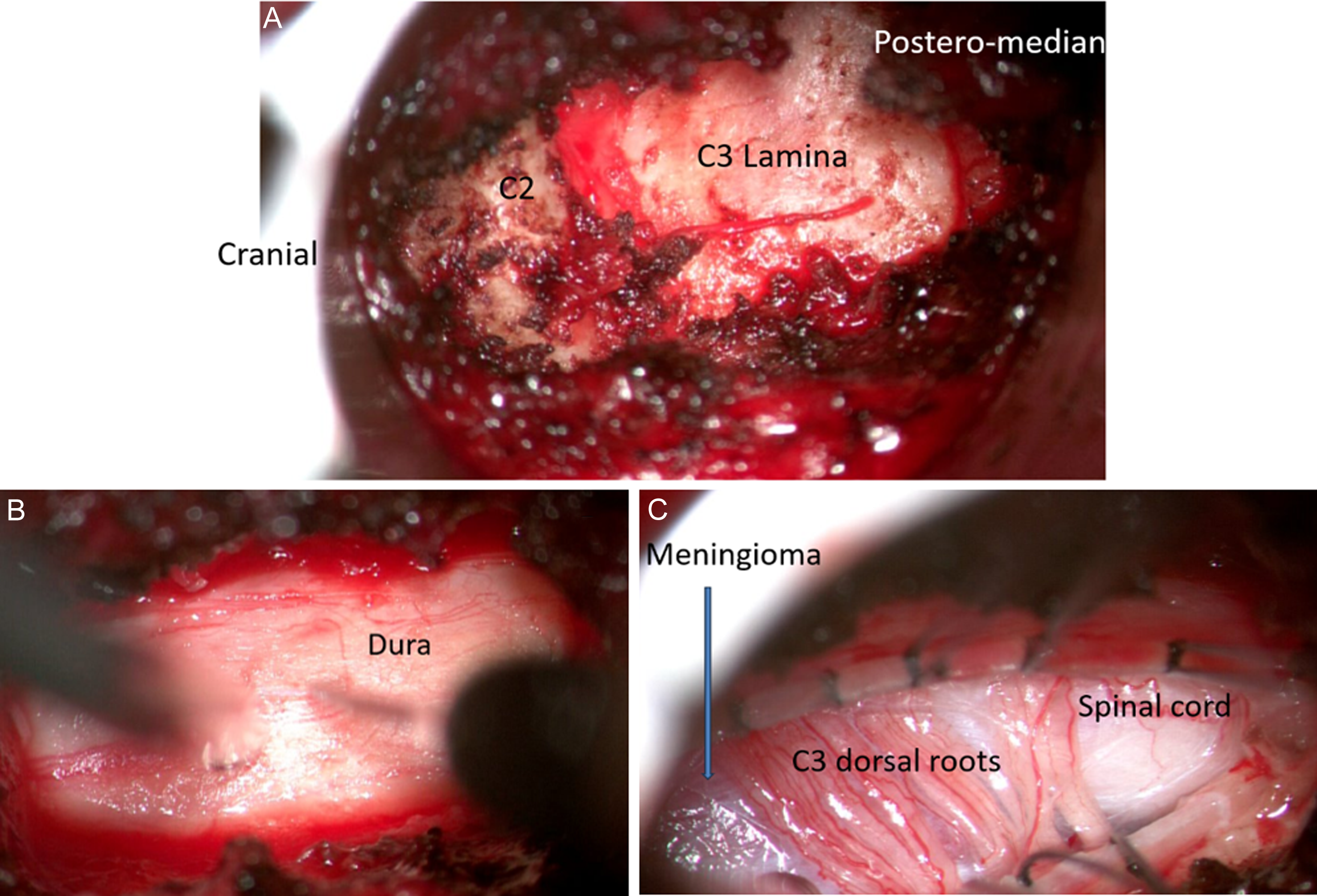
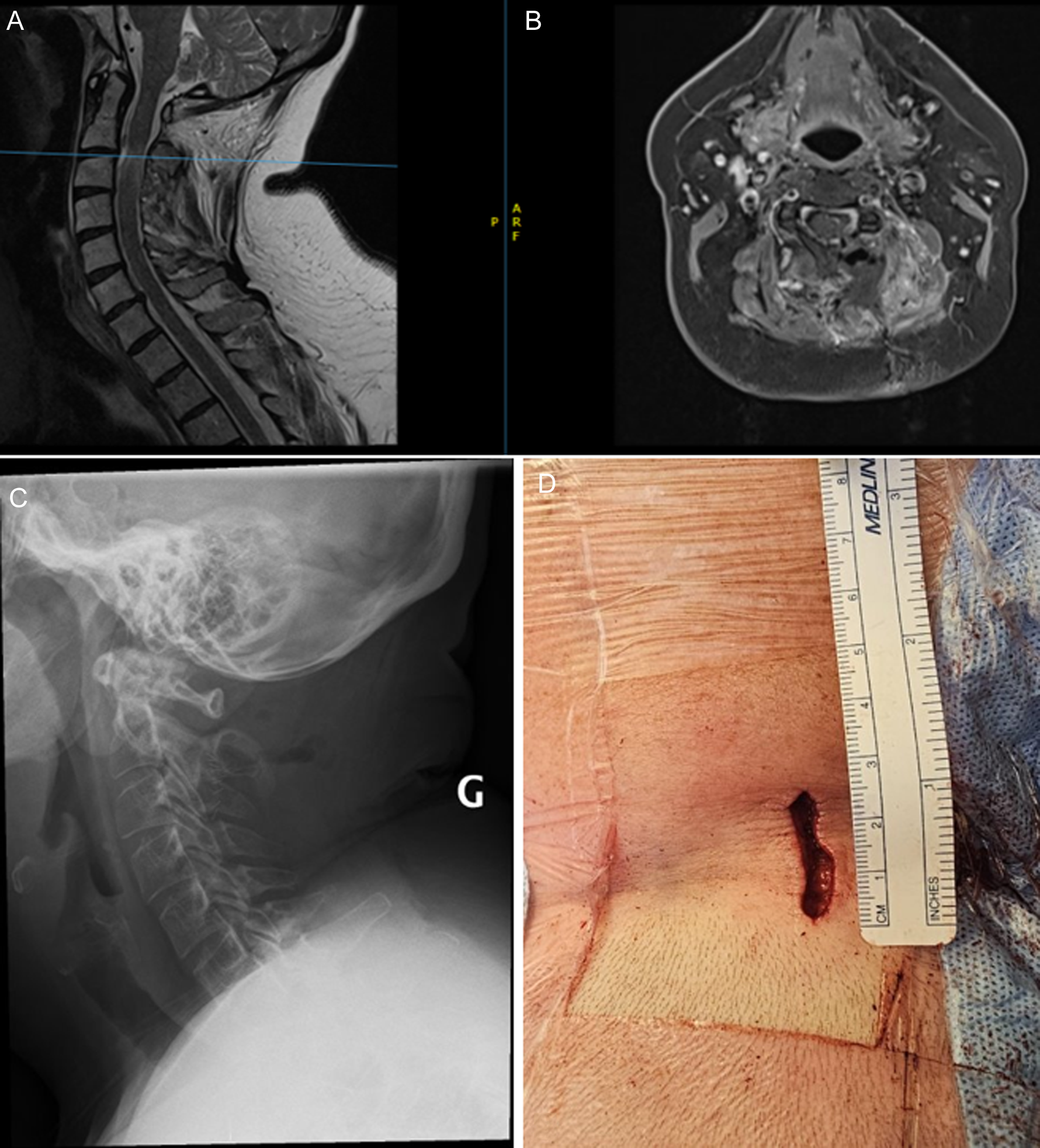
A 56-year-old female presented to our department with left upper extremity neuropathic pain accompanied by left-sided weakness (Table 3). Imaging revealed C2 – C3 lesion with a craniocaudal diameter of 2.9 cm (Figure 2). Intraoperative bony resection, dural opening and tumour exposure are illustrated in Figure 3. Surgery was performed as described in the Methods section. Intraoperative neuromonitoring confirmed proper neurological function. Post-operative imaging confirmed GTR, adequate spinal cord decompression with preserved joint integrity and spinal stability (Figure 4). The patient experienced no surgical complications and was discharged home on post-operative day 2. At 12-month follow-up, no tumour recurrence was reported (Table 4).
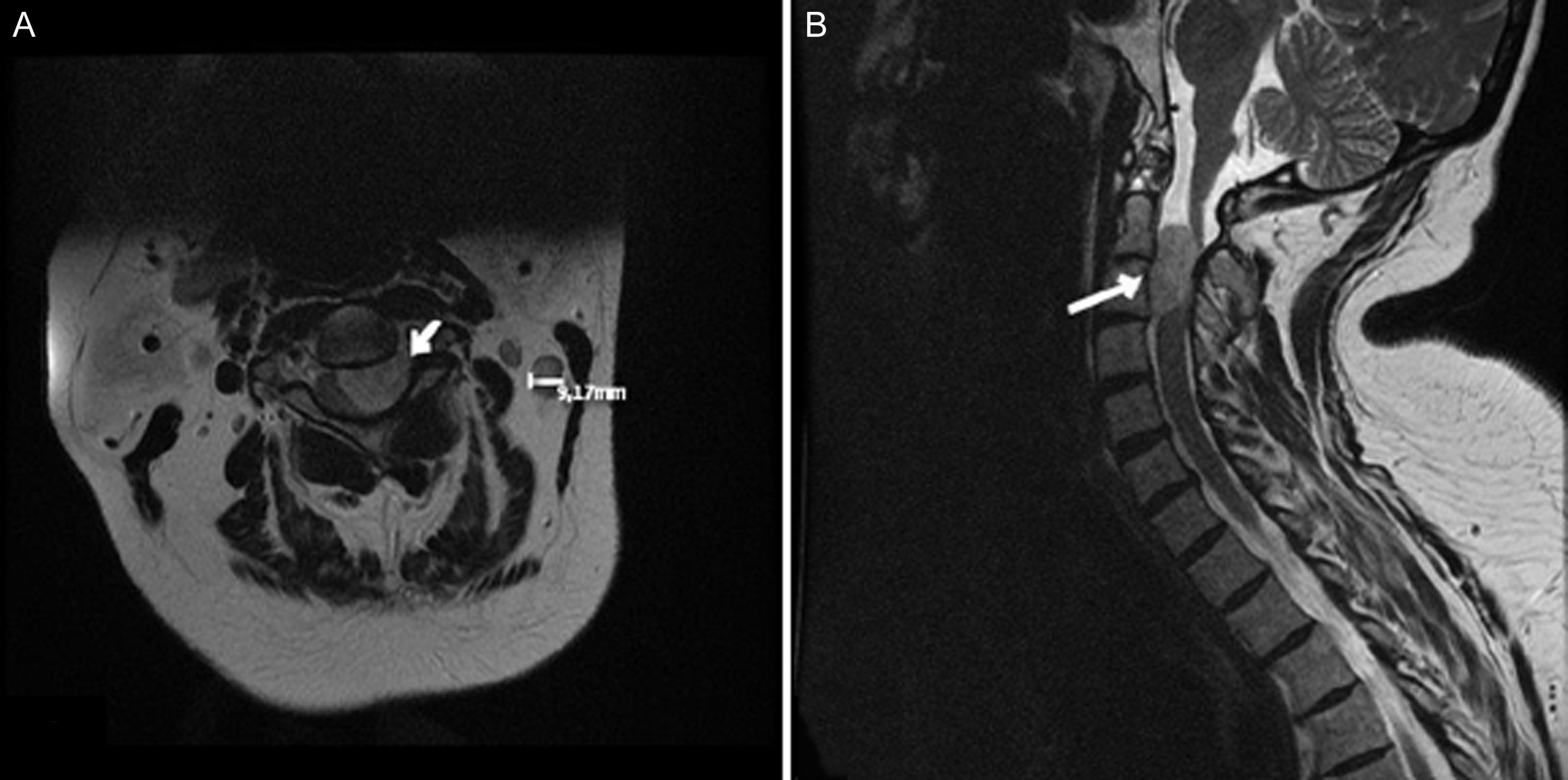
Figure 2. Patient 1 preoperative imaging. (A) Axial T2 MRI showing left meningioma (arrow). (B) Sagittal T2 MRI showing spinal cord compression by tumour (arrow). Image obtained with permission from the patient.
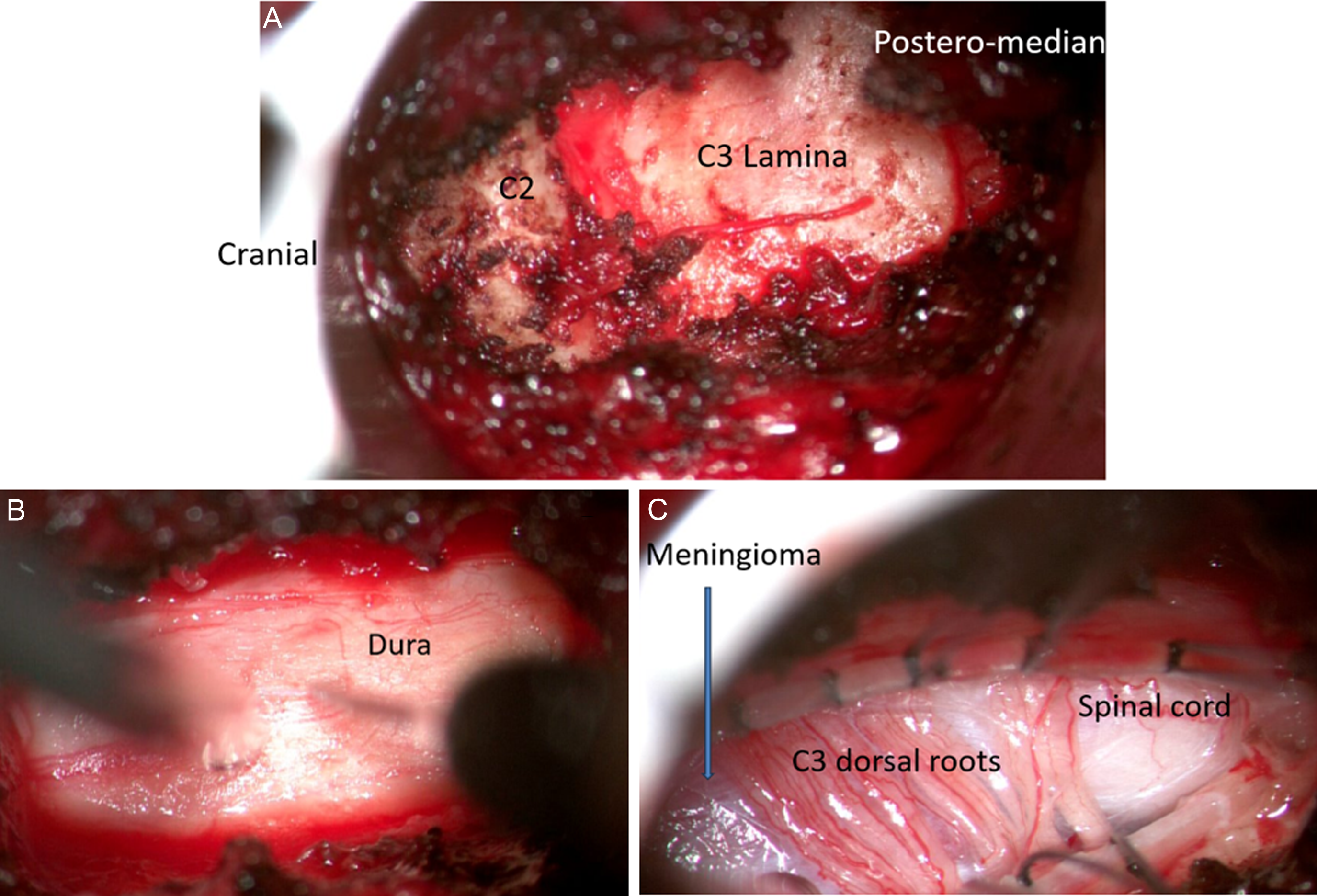
Figure 3. Patient 1 intraoperative imaging. (A) Lamina exposure. (B) Dural opening (C) Tumour exposure and debulking. Image obtained with permission from the patient.

Figure 4. Patient 1 post-operative imaging. (A) Sagittal T2 MRI and (B) Axial T2 MRI showing complete spinal cord decompression. (C) Post-op X-ray showing preserved spinal alignment. (D) Post-operative surgical corridor measuring 2.6 cm. Image obtained with permission from the patient.
Discussion
General discussion
The results of this case series parallel those of the systematic review in terms of surgical outcomes and safety. All patients in our series underwent GTR with Simpson grade 2 resection, as in most of the patients in our review. No post-operative complications nor tumour recurrence are reported in either our series or review. We noted neurological improvements in all our patients. That being said, tumour location differed slightly in our patient data set compared to the literature. Most of our patients had tumours involving the cervicothoracic region versus the craniospinal junction, as evidenced by our review. Overall, our results compare with the literature in terms of LOS and surgical outcomes.
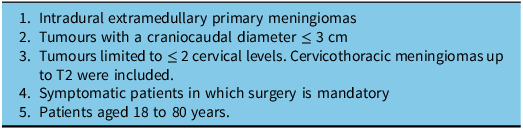
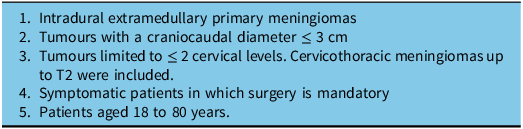
The analysis of our case series has enabled us to identify and outline key patient criteria defining suitable candidacy for cervical meningioma resection using MIS (Table 5). Adult patients with IDEM meningiomas less than 3 cm in craniocaudal diameter and limited to two or fewer cervical levels were suitable candidates for MIS. The 3 cm threshold was selected as a conservative and practical guideline during our initial experience with MIS for cervical meningiomas. It reflects our intent to prioritize patient safety by starting with smaller, more manageable lesions while building technical proficiency. As our familiarity with the approach increases, we plan to expand our indications to include larger and more complex tumours and are even considering raising the 3 cm cutoff in selected cases, provided oncologic and surgical safety can be maintained. Interestingly, we observed that an average spinal cord tumour occupation ratio of 77% was consistently associated with significant neurological symptoms warranting surgical intervention. This finding suggests a potential threshold beyond which spinal cord compression becomes clinically critical. While this ratio may not represent an absolute cutoff, it raises important questions about the relationship between tumour volume and symptom onset. Further prospective studies with larger sample sizes are needed to determine whether this ratio holds statistical significance and to explore its potential use as a prognostic marker or surgical indication guideline. Incorporating functional imaging and longitudinal clinical outcomes could also help refine this threshold and improve decision-making in spinal tumour management.
Table 5. Key patient criteria for minimally invasive surgery for cervical meningioma
MIS for tumours beyond the cervical region
In our review of the literature, the study from Raygor et al., despite not meeting our inclusion criteria as it involves lumbar tumours, stands out. Reference Raygor, Than, Chou and Mummaneni28 First, they compared thoracolumbar IDEM tumours using MIS expandable retractors versus open techniques. No cervical nor cervicothoracic junction lesions were studied. They had a total of 51 cases, with 25 managed by MIS and 26 through open surgery. In their study, the mean tumour size was not statistically significant between the MIS and open surgery groups, with mean tumour sizes of 1.9 and 3.0 cm respectively (p-value = 0.07). Reference Raygor, Than, Chou and Mummaneni28 Similar to our study, Raygor’s study found that all patients treated with MIS did not require spinal instrumentation and fusion, unlike four of their patients treated with open surgery (p-value <0.001). Reference Raygor, Than, Chou and Mummaneni28 Overall, both our study and that of Raygor’s demonstrated improved patient outcomes and safety of MIS for management of spinal tumours. This similar safety profile is of clinical relevance especially since lumbar procedures are technically more permissive due to the ability to mobilize the cauda equina, an option not available when operating around the cervical spinal cord. As such, we believe some might shy away from performing MIS at cervical levels due to the more unforgiving anatomy.
Minimally invasive surgery vs. open surgery
Mannion and colleagues describe three criteria that must be met to argue that MIS techniques are superior compared to traditional open surgery techniques. Reference Mannion, Nowitzke, Efendy and Wood26 First, the same surgical goal can be accomplished with a smaller surgical corridor. Reference Mannion, Nowitzke, Efendy and Wood26 Second, the risks to the patient are not increased. Reference Mannion, Nowitzke, Efendy and Wood26 Third, the use of MIS techniques provide advantages over open techniques. Reference Mannion, Nowitzke, Efendy and Wood26 In our experience, MIS is particularly well suited for dorsal and anterolateral lesions, as these can be accessed directly through a paramedian tubular approach. Ventrally located lesions can also be effectively accessed using a minimally invasive approach as demonstrated by Eicker et al., who employed MIS techniques for ventral tumours located at the craniovertebral junction. Reference Eicker, Mende, Duhrsen and Schmidt29
MIS has accomplished GTR without additional complications when compared to traditional open surgery, and presents several advantages, especially regarding patient-centred benefits. Traditional posterior open surgery for these lesions often necessitates extensive bony resection and the removal of facets, which can result in spinal instability requiring instrumented fusion. Reference Pan, Ma, Feng, Chen, Qin and Huang30–Reference Wang, Jiang, Jiang and Dai32 While sometimes necessary, fusion can severely limit the range of motion in the cervical spine. Reference Patel, Canseco, Houlihan, Gabay, Grasso and Vaccaro3,Reference Lee, Kim, Park and Kang33 MIS techniques minimize these risks by allowing surgeons to limit bony resection, circumventing the need for fusion all while providing direct tumour access. Reference Hussain, Schmidt, Kirnaz, Wipplinger, Schwartz and Härtl2,Reference Patel, Canseco, Houlihan, Gabay, Grasso and Vaccaro3 Another benefit of MIS is preservation of the posterior ligamentous complex, which helps maintain spinal stability and avoid post-operative kyphosis, which can occur in approximately 20% of patients following multilevel cervical laminectomy. Reference Deutsch, Haid, Rodts and Mummaneni34,Reference Fassett, Clark, Brockmeyer and Schmidt35 Furthermore, MIS is associated with reduced post-operative pain, shorter hospital stays, lower rates of surgical site infections and quicker return to daily activities, factors that are particularly important in elderly or comorbid populations. Nonetheless, open surgery remains essential in select complex cases where MIS may fall short. In cases involving extensive anatomical distortion, poor bone quality or the need for robust biomechanical stabilization, open surgery with advanced fixation techniques remains the most reliable option to achieve durable decompression and stability. Reference Ndongo Sonfack, Bergeron, Wang, Boubez, Shedid and Yuh36,Reference Lak, Lamba and Pompilus37 Additionally, open approaches may offer superior visualization and manoeuvrability in certain tumour resections, particularly those involving extensive dural involvement or requiring en bloc removal. Nevertheless, MIS help patients maintain better mobility and quality of life post-surgery. Reference Patel, Canseco, Houlihan, Gabay, Grasso and Vaccaro3,Reference Lee, Kim, Park and Kang33
There are several distinct MIS techniques currently in use, each with its own advantages and limitations. Reference Sharif, Shaikh and Peev1 Fixed tubular retractors provide a stable, well-defined working channels and are favoured for their familiarity and ease of setup. Reference Sharif, Shaikh and Peev1,Reference Joris, Weil, Gennari and Yuh38,Reference Kanter, Tempel, Ozpinar and Okonkwo39 However, they offer limited visualization and working space, which can be challenging in larger or more complex lesions. However, this can be overcome by slightly adjusting the angle of the working channel. Expandable tubular systems overcome this by allowing surgeons to directly dilate the retractor to increase the working angle or footprint, thereby maintaining a minimally invasive profile while improving versatility and visibility. Reference Sharif, Shaikh and Peev1,Reference Kim and Kim40 Endoscopic techniques take MIS further by enabling the use of high-definition cameras and angled visualization, which can enhance illumination and exposure in anatomically constrained space. Reference Sharif, Shaikh and Peev1,Reference Sofoluke, Barber, Telfeian, Hofstetter and Konakondla41 Endoscopic techniques in oncology, while promising, is limited by several significant factors including a steep learning curve for surgeons due to constrained working space and lack of bimanual instrumentation, restricted availability of specialized tools for tasks like firm tumour resection and hemostasis, technical challenges in achieving secure dural closure, and difficulty managing large or multilevel tumour. Reference Sofoluke, Barber, Telfeian, Hofstetter and Konakondla41 Additionally, its application remains largely exploratory, as current evidence is based predominantly on small case reports and case series, making it difficult to draw definitive conclusions about long-term outcomes, safety and efficacy. Reference Sofoluke, Barber, Telfeian, Hofstetter and Konakondla41
Strengths and limitations
This case series serves as a preliminary study to assess the safety of MIS for cervical meningiomas in comparison to existing literature. The strength of this article lies in its extensive review of the literature in accordance with the PRISMA guidelines. This ensures a thorough, rigorous and transparent assessment of the available literature, thereby reducing selection bias. However, the article does have some limitations. In our case series, we focused on IDEM lesions, specifically meningiomas, to gain experience with MIS in intradural oncological pathologies before attempting more complex lesions. This limits applicability to patients with larger and more complex tumours. Moreover, tumour size was inconsistently reported across the included studies, which restricted our ability to analyse its influence on surgical approach and outcomes. While our findings provide valuable insights, their generalizability is limited by the small sample size and retrospective nature of the study. As a next step, we plan to conduct a multicentre study with a larger patient population and extended follow-up duration. A control group will be included to compare patient outcomes and quality of life data between those undergoing MIS and open surgery. As our experience continues to grow, technical nuances and surgeon learning curves will become better defined.
Conclusion
We believe we have shown that clinicians should not shy away from using MIS for the resection of cervical and cervicothoracic IDEM lesions. In well-selected patients, MIS is a safe and effective option, allowing direct access to the tumour with minimal bony resection, thereby avoiding fusion and improving post-operative patient mobility and quality of life.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cjn.2025.10366.
Acknowledgements
We thank all our patients and staff for making this work possible. We thank our librarian Frederic Bergeron for verifying our search strategy.
Authors contributions
Conception and design: SY, DS
Acquisition of data: DJNS, TBC, LO, SY
Analysis and interpretation of data: DJNS, TBC
Drafting the article: DJNS, TBC
Revision of article: DJNS, TBC, LO, AG, DS, SY
Submission of article: DJNS
Funding statement
No funding was obtained for this study.
Competing interests
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Declaration Of Generative AI And AI-assisted Technologies In The Writing Process
During the preparation of this work, the authors used ChatGPT 4 to improve clarity of English language in some sections of the text. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.


Target article
Minimally Invasive Surgery for Cervical Meningioma: A Systematic Review and Case Series
Related commentaries (2)
Reviewer Comment on Ndongo Sonfack et al. “Minimally Invasive Surgery for Cervical Meningioma: Systematic Review and Case Series”
Reviewer Comment on Ndongo Sonfack et al. “Minimally Invasive Surgery for Cervical Meningioma: Systematic Review and Case Series”